Open reduction; Cerclage compression wiring
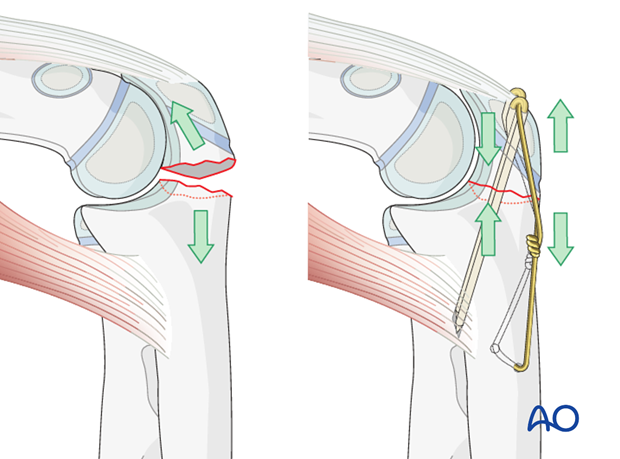
The philosophy behind cerclage compression wiring for the olecranon is that it converts tensile forces on the posterior side of the olecranon into compression forces at the joint line during flexion. The fixation is simple and inexpensive and works well if executed properly.
Choose a wire of sufficient strength to withstand the tensile forces generated in the figure-of-eight loop (1.0 mm). Positioning the K-wires as close to the joint while also penetrating the volar cortex is paramount.
Note: “Cerclage compression wire fixation” was referred to as “Tension band fixation”. We now prefer the term “Cerclage compression wire fixation” because the tension band mechanism cannot be applied consistently to each component of the fracture fixation. An explanation of the limits of the Tension band mechanism/principle can be found here.
1. Instruments and implants
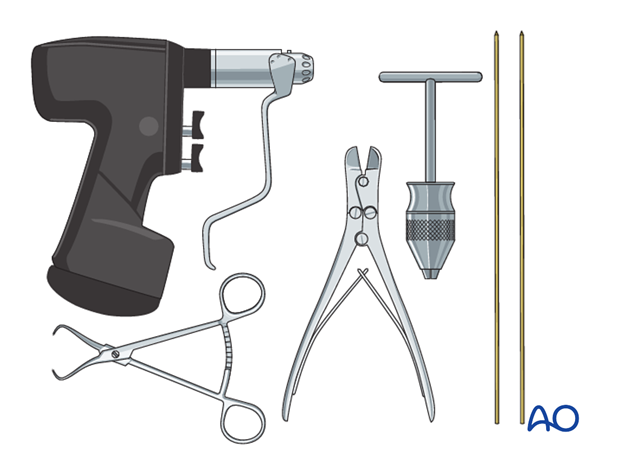
The following equipment is needed:
- K-wires of appropriate sizes
- Wire of appropriate strength
- Drill or a T-handle for manual insertion
- Two pliers for wire twisting
- Wire cutting instruments
- Standard orthopedic instrument set
Alternative: Use a high-strength, braided composite suture or tape instead of figure-of-eight wire.
2. Patient preparation and approach
Patient preparation
This procedure may be performed with the patient in either a supine position or a lateral decubitus position.
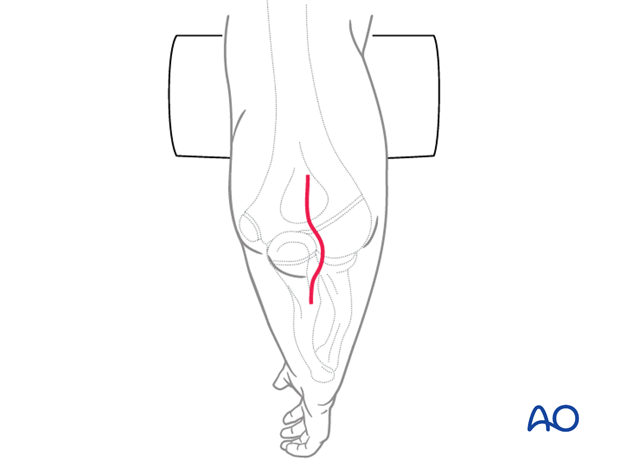
Approach
For this procedure a posterior approach is normally used.
3. Reduction
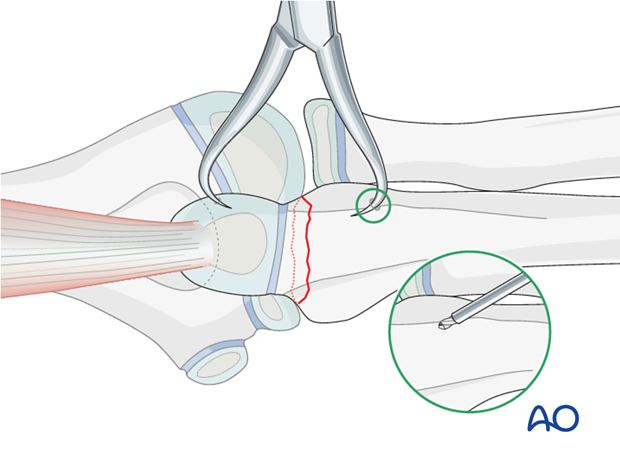
There is almost always a small spike on one of the fragment sides that exactly fits into a gap on the opposite fragment.
Reduce and hold the reduction of the transverse olecranon fracture with a small pointed reduction forceps.
Pearl: Drill a small unicortical hole in the distal fragment to secure the reduction forceps.
4. Prepare wire insertion
Drilling
Drill a hole through the ulna approximately 2-4 cm distal to the fracture line and 5 mm from the posterior cortex.
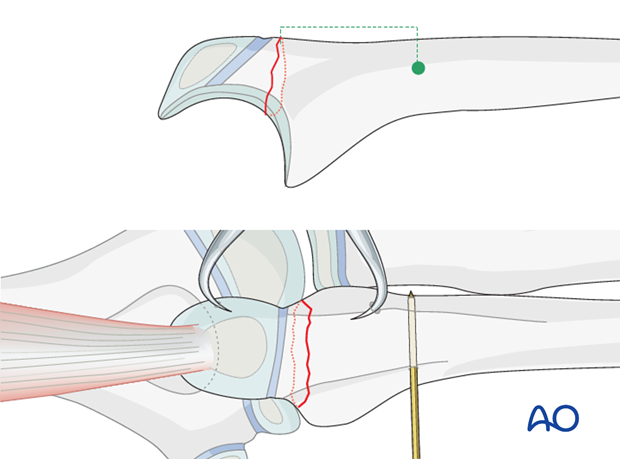
Wire preparation and insertion
Prepare the wire by making a loop approximately one third along its length.
Insert the shorter segment of the wire through the drilled hole from medial to lateral. As the ulnar nerve is medial it is safer to introduce the wire from this side.
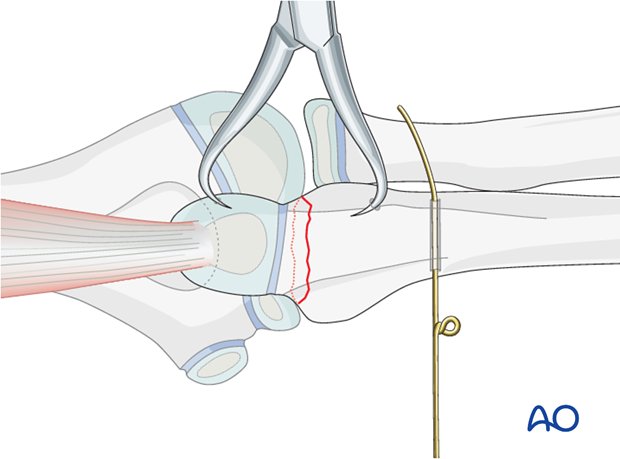
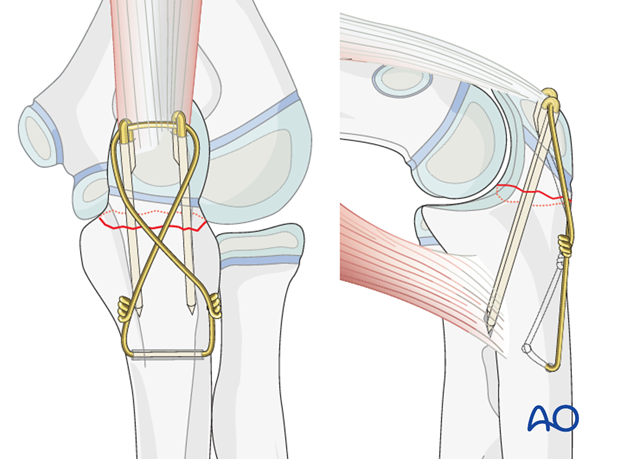
5. Insertion of K-wires
First K-wire
Using the drill guide, introduce the first K-wire medially through the olecranon apophysis.
Aim the drill towards the anterior cortex, passing as close as possible to the joint. Leave enough space on the lateral side for the second K-wire.
Drill the K-wire through both cortices.
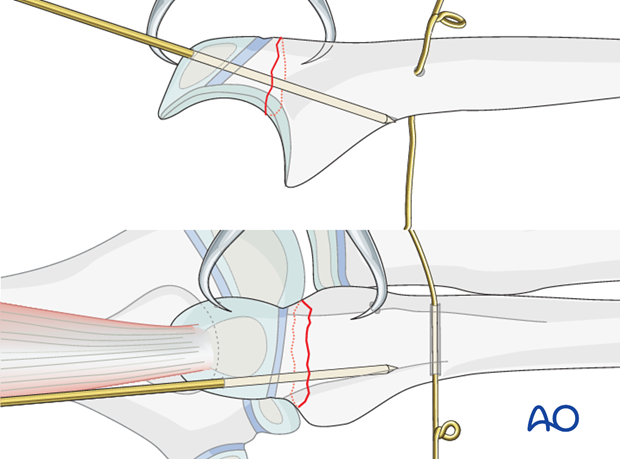
Second K-wire
Insert a second parallel K-wire.
Check the position of both K-wires with image intensification.
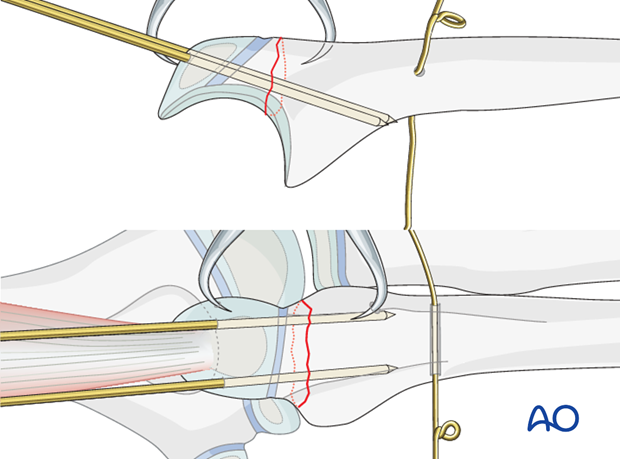
6. Wire fixation
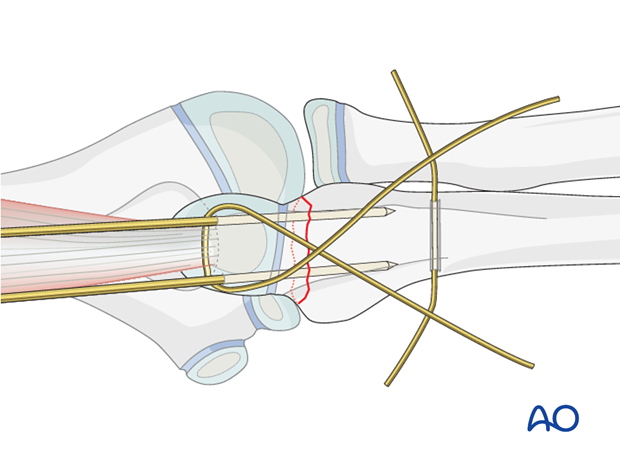
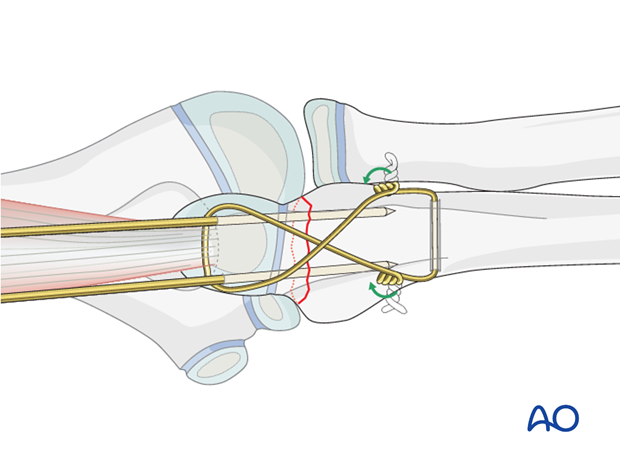
Figure-of-eight configuration
Remove the small pointed reduction forceps.
Pass the long segment of the wire (bearing the loop) in a figure-of-eight configuration beneath the triceps tendon around the protruding ends of the K-wires.
Twist the two wires ends together.
Note: Make sure that the loop and wire twist do not lie too close to the wire hole to avoid unnecessary tension at the wire hole.
Placing the loops more proximally will allow a smaller incision when removing them after healing.
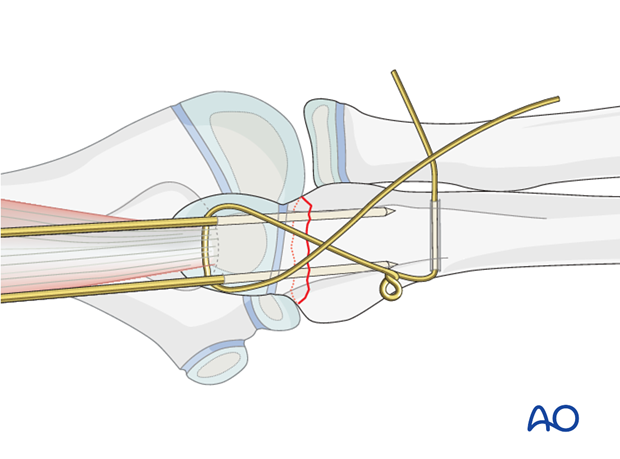
Some surgeons find it easier to use two separate pieces of wire instead of one loop to create the cerclage compression wiring.
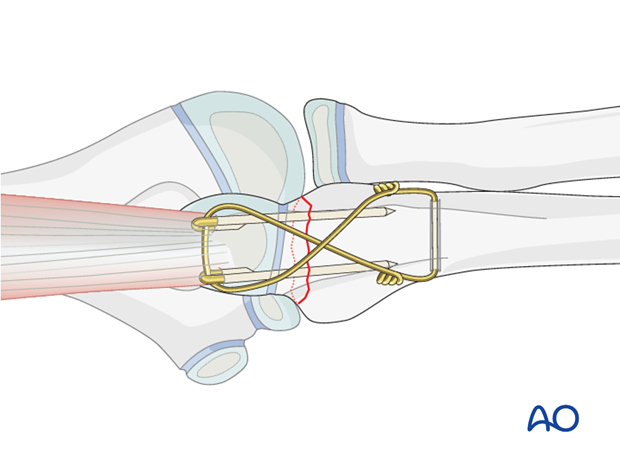
Tightening the wire
Ensure that each end of the wire spirals equally - the twist should not comprise one spiral around a straight wire.
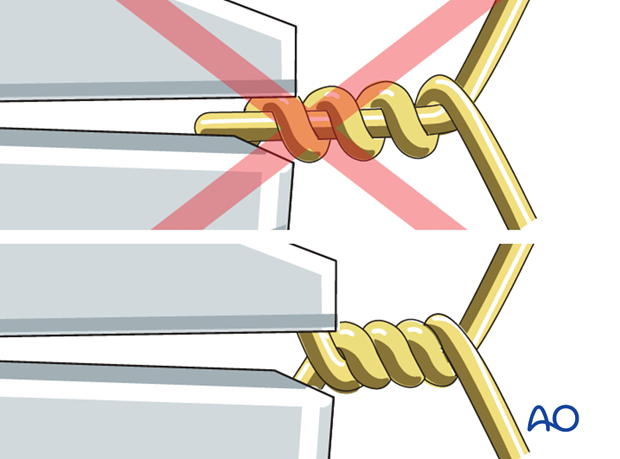
Cut the wire ends short.
The slack is then taken up by further twisting. Repeat this until the desired tension is achieved. Both loops must be tightened at the same time and in the same direction, to achieve equal tension on both arms of the wire.
By tightening the twist and the loop with two pliers simultaneously, the two fragments are drawn together such that the fracture is placed under compression.
Note: Avoid excessive tensioning.
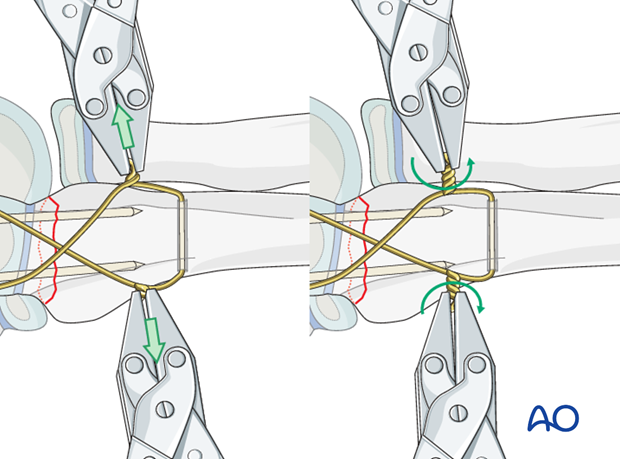
Prevention of later soft-tissue irritation
Trim the twisted wire and turn both ends towards the ulna/olecranon to minimize soft-tissue irritation.
Sinking the K-wires
Bend the proximal end of the K-wires 180° with pliers, bending irons or forceps and cut the K-wires.
Sink the curved ends into the olecranon or triceps tendon to prevent backing out and skin irritation.
7. Final assessment
Confirm fracture stability and range of motion, including supination-pronation.
Exclude K-wire penetration into the humeroulnar or radioulnar joint.
Final x-rays or image intensifier views should show good reduction and correct hardware position.
8. Aftercare following cerclage compression wiring
Immediate postoperative care
Whilst the child remains in bed, the elbow and forearm should be elevated on pillows to reduce swelling and pain.

Cast or splint immobilization
Fixation of olecranon fractures with cerclage compression wiring is intrinsically stable and supplementary casting or splinting is therefore not required.
Analgesia
Ibuprofen and paracetamol should be administered regularly during the first 24-48 hours after surgery, with opiate analgesia for breakthrough pain.
Opiates should not be necessary after 48 hours and regular ibuprofen and paracetamol should be sufficient until 4-5 after injury or surgery.
The child should be examined if the level of pain is increasing or prolonged analgesia is needed.
Neurovascular examination
The child should be examined regularly, to ensure finger range of motion is comfortable and adequate.
Neurological and vascular examination should also be performed.
Compartment syndrome should be considered in the presence of increasing pain, especially pain on passive stretching of muscles, decreasing range of active finger motion or deteriorating neurovascular signs, which is a late phenomenon.
See also the additional material on complications and postoperative infections.
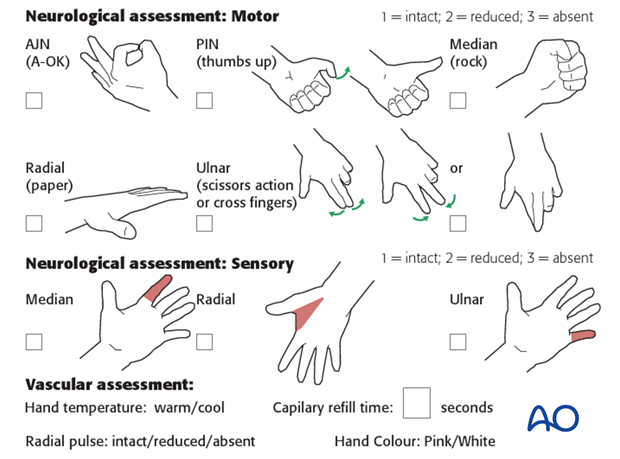
Compartment syndrome
Compartment syndrome is a possible early postoperative complication that may be difficult to diagnose in younger children.
The presence of full passive or active finger extension, without discomfort, excludes muscle compartment ischemia.
If there are signs of a compartment syndrome:
- Remove or split constrictive dressings or casts.
- Elevate the limb.
- Encourage active finger movement.
- Reexamine the child after 30 min.
If a definitive diagnosis of compartment syndrome is made, then a fasciotomy should be performed without delay.

Discharge care
Discharge from hospital follows local practice and is usually possible after 1-3 days.
The parent/carer should be taught how to assess the limb.
They should also be advised to return if there is increased pain or decreased range of finger movement.
It is important to provide parents with the following additional information:
- The warning signs of compartment syndrome, circulatory problems and neurological deterioration
- Hospital telephone number
- Information brochure
For the first few days, the elbow and forearm can be elevated on a pillow, until swelling decreases and comfort returns.
The arm can be placed in a sling for a few days until the patient is pain free. Many children are more comfortable without support.
Mobilization
Early movement of the elbow should be encouraged as soon as the patient is pain free.
Formal physiotherapy is normally not indicated, but children should have a sheet of exercises to stimulate mobilization. See also the additional material on elbow stiffness.
Follow-up
The first clinical and radiological follow-up is usually undertaken 2-3 weeks postoperatively.
At this point, the child should be able to move the elbow with only slight restriction.
AP and lateral x-rays are required.
See also the additional material on complications and healing times.
Cerclage wire removal
Cerclage wire removal is delayed until function has fully recovered and can be performed as a day case, under general anesthesia.
Usually the incision is smaller than for open reduction if the twisted wire ends lay close to the olecranon tip. Sometimes for cosmetic reasons, it is best to resect the whole scar and use cosmetic wound closure.
Make a small incision over the olecranon tip and extract the two K-wires with pliers.
Unwind or cut the twisted wire and pull it out of the bony track.
Close the wound in layers.













