ESIN
1. General considerations
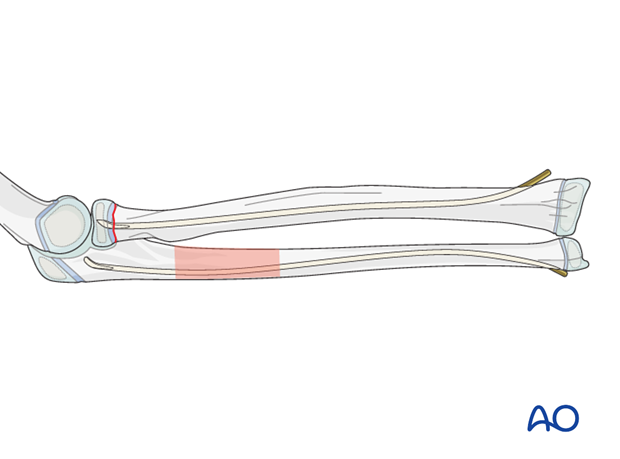
Most ulnar fractures are in the proximal 1/3 and retrograde nailing of both bones is therefore recommended.
The ESIN method involves closed reduction and internal fixation of both fractures with elastic nails or K-wires.
It can be used in any age group and any combination of fracture types.
Note: The risk of avascular necrosis of the radial head is higher after open reduction, which should be avoided if possible.
2. Patient preparation
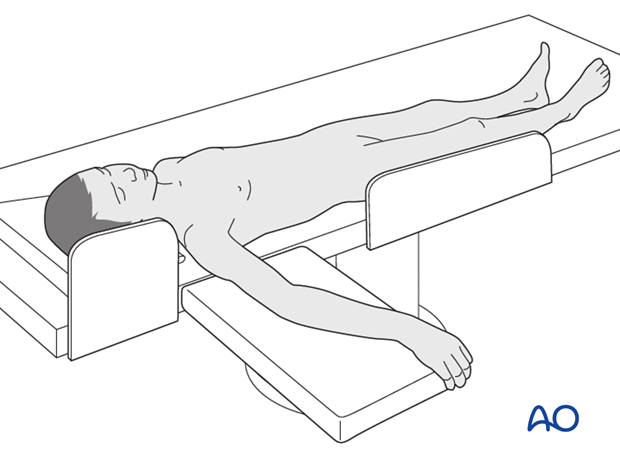
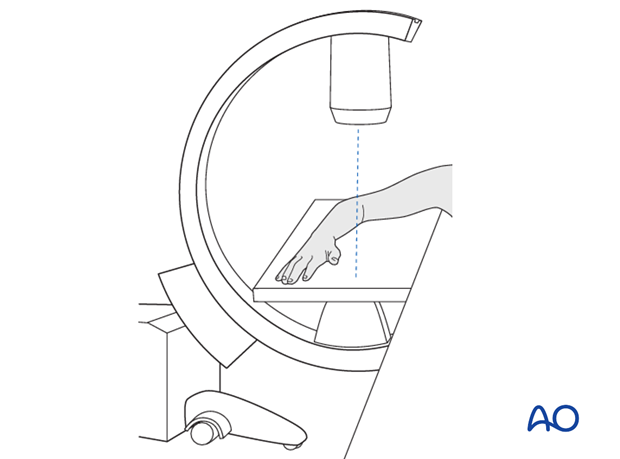
This procedure is normally performed with the patient in a supine position.
3. Entry points
Entry point to the ulna
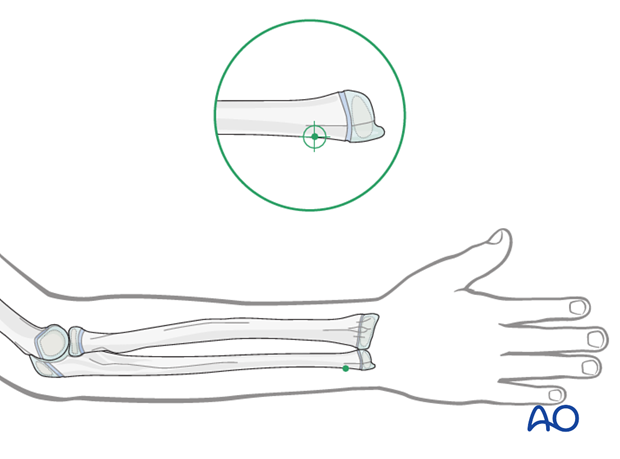
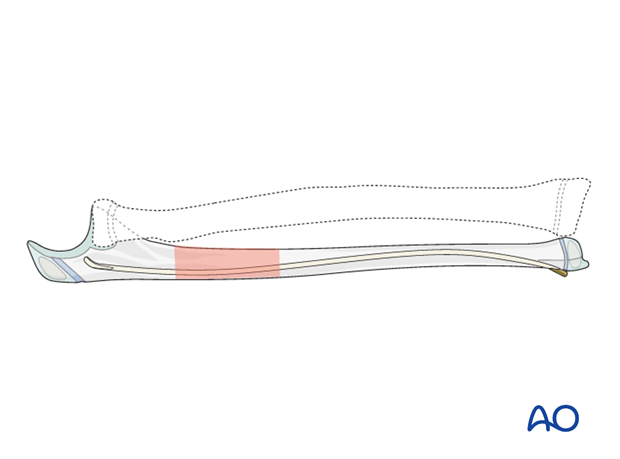
In the ulna use the distal medial entry point.
Entry points to the radius
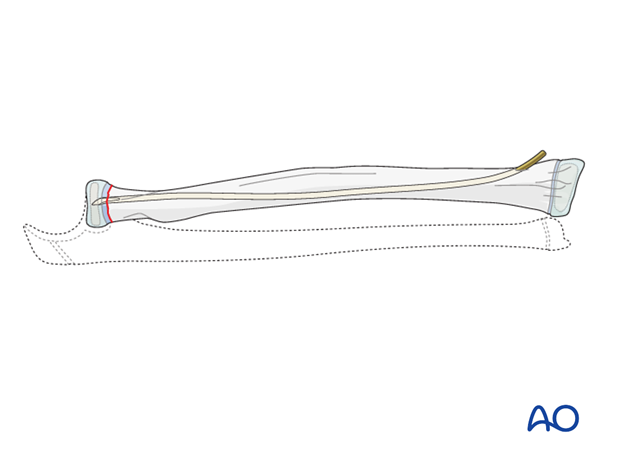
The distal lateral entry point is in common use and shown in this example.
The dorsal entry point ((Lister’s tubercle)) is also well established and offers more versatile nail manipulation.
Find more details in ESIN entry points (radius).

4. Reduction and fixation
Order of reduction and fixation
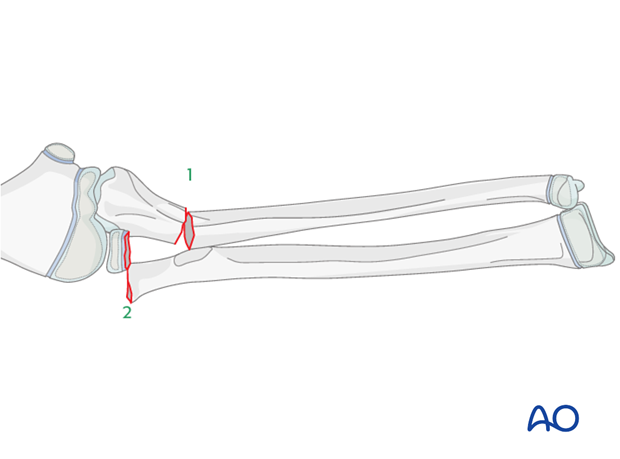
The ulnar fracture (1) is treated first.
The radial neck fracture (2) may spontaneously reduce after anatomical reduction and fixation of the ulna.
The radial neck fracture should also be fixed with an intramedullary nail to prevent redisplacement and to allow early joint mobilization.
Reduction and fixation of the ulna
The steps for ulnar fracture fixation are described in the ESIN procedure (retrograde nail insertion).
Reduction and fixation of radial head/neck
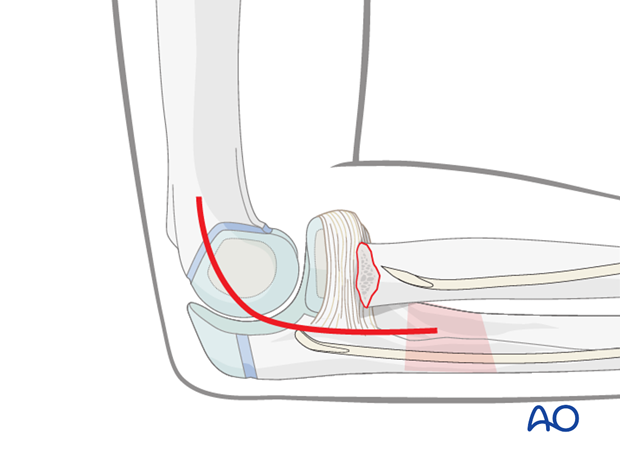
The steps required for proximal radial fracture fixation are described in the ESIN procedure, illustrated with a 21r-E/1.1 fracture.
This technique is also appropriate for reduction and fixation of other proximal radial fracture types.
If an open reduction of the radial neck fracture is necessary a lateral approach to the proximal radius may be used.
5. Final assessment
Check the completed osteosynthesis with image intensification. These images should be retained for documentation.
If an image intensifier is not available an x-ray should be obtained before discharge.
Make sure that the desired reduction has been achieved and the nails are of appropriate length.
6. Aftercare following ESIN
Immediate postoperative care
Whilst the child remains in bed, the elbow and forearm should be elevated on pillows to reduce swelling and pain.
They should be encouraged to use the arm.

Cast immobilization
Cast immobilization is not necessary and hinders early recovery of joint movement.
Analgesia
Ibuprofen and paracetamol should be administered regularly during the first 24-48 hours after surgery, with opiate analgesia for breakthrough pain.
Opiates should not be necessary after 48 hours and regular ibuprofen and paracetamol should be sufficient until 4-5 after injury or surgery.
The child should be examined if the level of pain is increasing or prolonged analgesia is needed.
Neurovascular examination
The child should be examined regularly, to ensure finger range of motion is comfortable and adequate.
Neurological and vascular examination should also be performed.
Compartment syndrome should be considered in the presence of increasing pain, especially pain on passive stretching of muscles, decreasing range of active finger motion or deteriorating neurovascular signs, which is a late phenomenon.
See also the additional material on complications and postoperative infections.
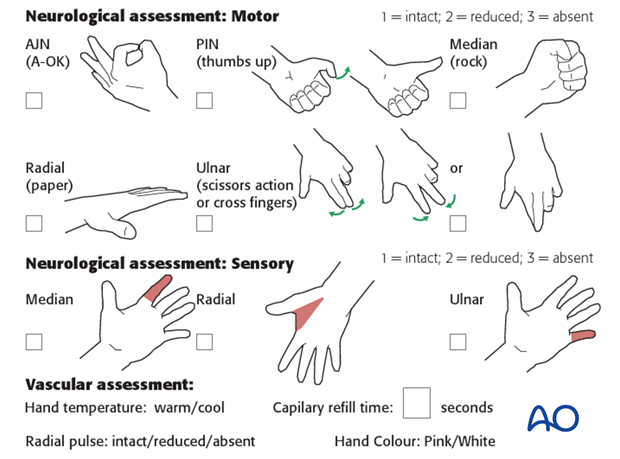
Compartment syndrome
Compartment syndrome is a possible early postoperative complication that may be difficult to diagnose in younger children.
The presence of full passive or active finger extension, without discomfort, excludes muscle compartment ischemia.
If there are signs of a compartment syndrome:
- Remove or split constrictive dressings or casts.
- Elevate the limb.
- Encourage active finger movement.
- Reexamine the child after 30 min.
If a definitive diagnosis of compartment syndrome is made, then a fasciotomy should be performed without delay.

Discharge care
Discharge from hospital follows local practice and is usually possible after 1-3 days.
The parent/carer should be taught how to assess the limb.
They should also be advised to return if there is increased pain or decreased range of finger movement.
It is important to provide parents with the following additional information:
- The warning signs of compartment syndrome, circulatory problems and neurological deterioration
- Hospital telephone number
- Information brochure
For the first few days, the elbow and forearm can be elevated on a pillow, until swelling decreases and comfort returns.
The arm can be placed in a sling for a few days until the patient is pain free. Many children are more comfortable without support.
Mobilization
Early movement of the elbow and forearm should be encouraged as soon as the patient is pain free.
Formal physiotherapy is normally not indicated, but children should have a sheet of exercises to stimulate mobilization. See also the additional material on elbow stiffness.
Follow-up
The first clinical and radiological follow-up depends on the age of the child and is usually undertaken 4-6 weeks postoperatively.
At this point, the child should be able to move the elbow and forearm almost fully with some limited rotation caused by callus formation.
AP and lateral x-rays are required.
See also the additional material on complications and healing times.
Nail removal
Nail removal is delayed until the fracture has modelled completely and can be performed as a day case, under general anesthesia.
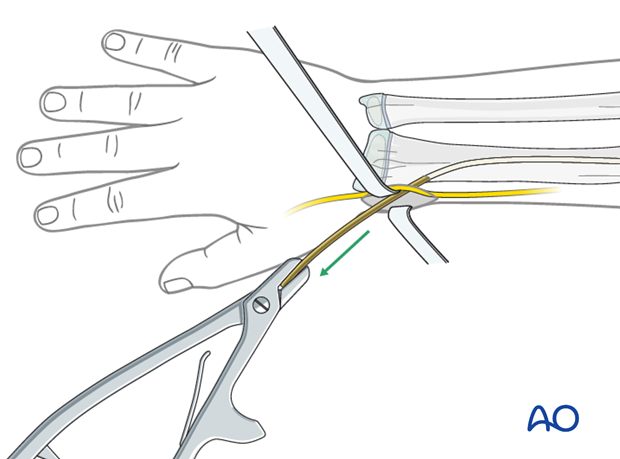
The nail end may slip under tendons and nerves. This may irritate the soft tissues and make it difficult to palpate the nail tip.
Exposure of the nail end should be performed under direct vision with small retractors.
In most cases, a small bursa forms over the nail tip. Once this bursa is opened, the end of the nail can be seen.
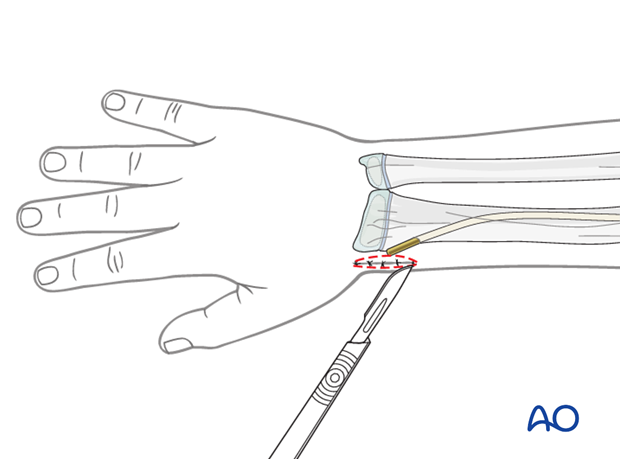
The nail can be removed with the extraction pliers, or a similar clamp. A strong needle holder is also useful.