Syndesmotic transfixation with screws
1. General considerations
Introduction
Syndesmotic injuries and isolated injuries to ligaments are rare before skeletal maturity.
Ligaments are generally stiffer than bone, and failure tends to occur through the physis or by avulsion of the ligament attachment at the epiphysis.
The physis begins to close in adolescents approaching skeletal maturity, and the fracture pattern and treatment are similar to adults.
Pronation/external rotation injuries of the ankle may result in a high fibular fracture with disruption of the syndesmosis and tibiofibular instability.
If the syndesmosis is disrupted, the anatomical relationship between the fibula and tibia must be maintained while the ligaments heal. This can be stabilized with transfixation screw(s). Ensure that insertion does not damage the distal tibial physis.
The syndesmotic screws are typically removed after 2–3 months to avoid breakage.
Skeletal maturity
The fracture pattern and treatment of skeletally mature adolescents is identical to adult patients. Isolated ligament injuries are more common in this age group.
The radiological appearance of the distal tibial physis should be assessed and the remaining growth estimated.
Treatment of an associated medial collateral (deltoid) ligament injury
Avulsed or ruptured medial collateral (deltoid) ligament does not usually need fixation. It may, however, block tibiotalar reduction and the incarcerated ligament must be removed from the joint.
Associated high fibular fractures
A fracture of the middle or proximal third of the fibular shaft may be part of a more complex injury and is often underestimated.
High fibular fractures may be associated with instability of the syndesmotic complex.
Restoration of length, axis, and rotation of the fibula at the level of the ankle joint is of primary concern.
The proximal fibular fracture is usually indirectly reduced and rarely requires separate fixation to increase the overall stability.
After transfixation of the syndesmosis, ankle joint stability should be assessed.
2. Instruments and implants
As this is a minimally invasive surgical technique, only a few instruments are necessary.
For the syndesmotic positioning screw, a 3.5 mm fully threaded screw (ideally self-tapping) may be used.
The following equipment is needed:
- Drill
- Image intensifier
3. Patient preparation
Place the patient in a supine position on a radiolucent table with a block under the lower leg proximal to the heel.

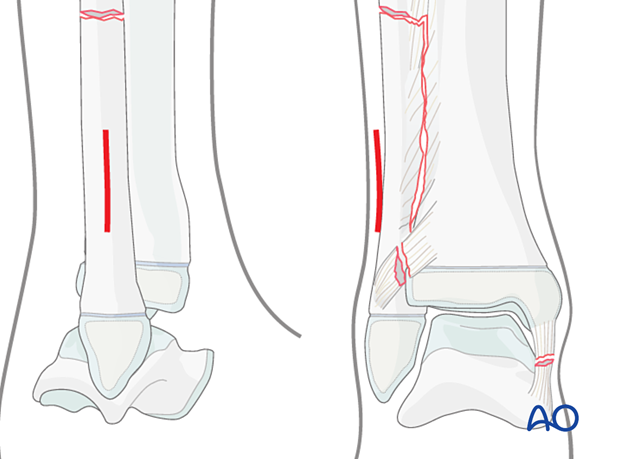
4. Skin incision for syndesmosis stabilization
Use an image intensifier to determine the correct level.
Incise the skin slightly posterior and lateral to the fibula, proximal to the tibial physis.
5. Reduction
Restoring length, axis, and rotation of the fibula
A small bone hook may be inserted above the fibular physis to pull the lateral malleolus distally until perfect reduction of the distal tibiofibular joint is achieved.
If the fibula/talus does not reduce anatomically, there may be entrapment of the deltoid (medial collateral) ligament which must be removed through a medial approach.
Use an image intensifier to check rotation, length, and anteroposterior translation of the fibula.
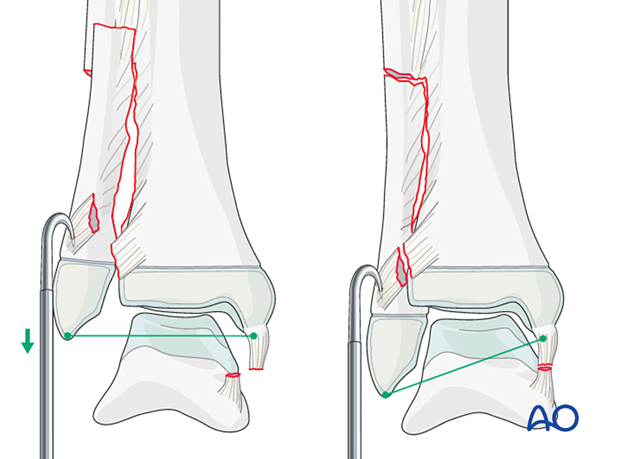
Preliminary fixation with a K-wire
Stabilize the reduction with a 2.0 mm K-wire, inserted from the lateral side, distal to the planned distal screw and proximal to the tibial physis.
The ankle joint should be in the neutral position during this maneuver.
Confirm reduction with an image intensifier in both planes.
The reduction must be anatomical and should be confirmed by comparison with images of the uninjured ankle.
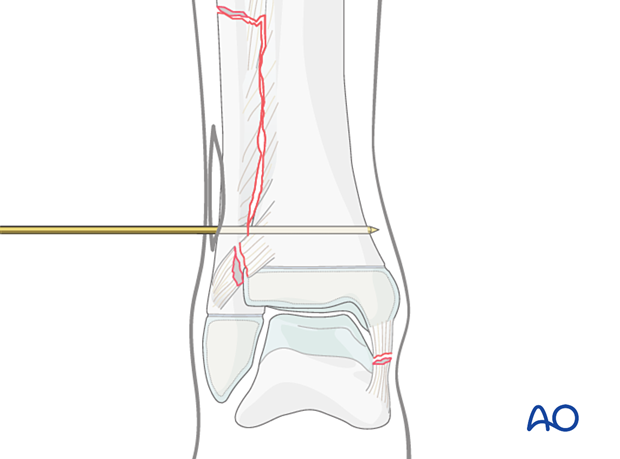
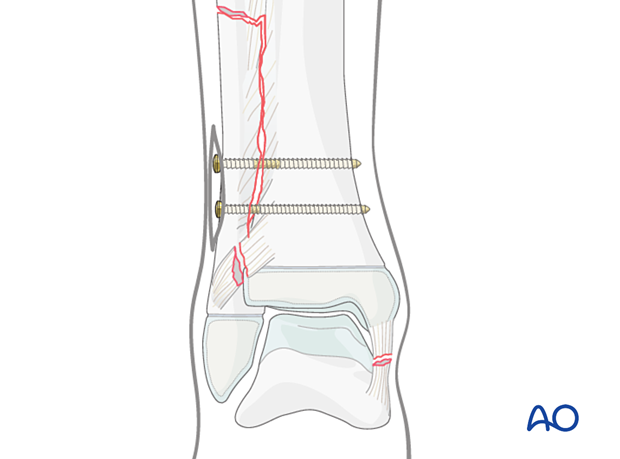
6. Screw fixation of the syndesmotic complex
Drilling
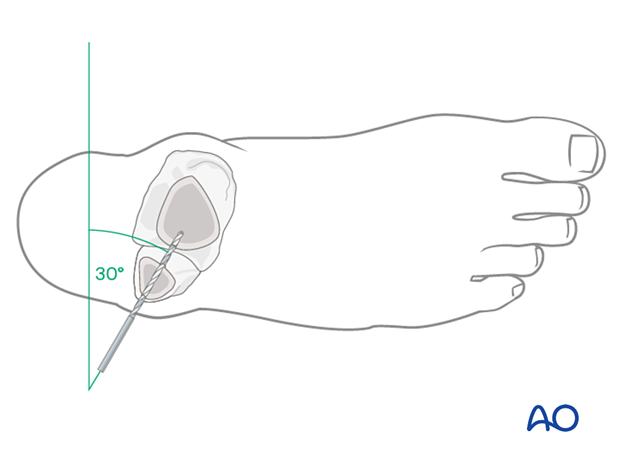
With the ankle joint in the neutral position, drill a 2.5 mm hole through the fibula and tibia, just proximal to the inferior tibiofibular joint, parallel to the tibial physis and …
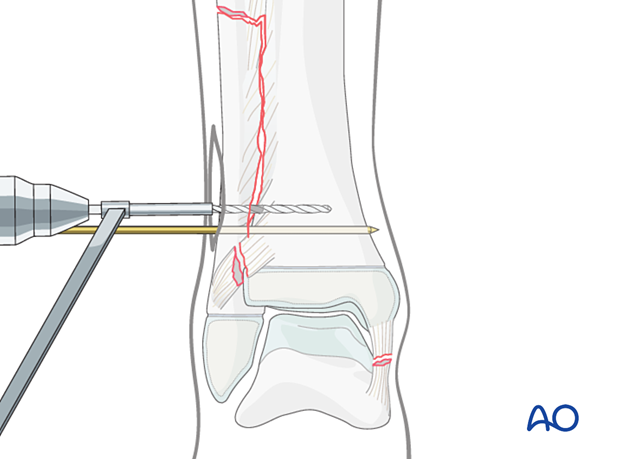
… 30° from posterior to anterior.
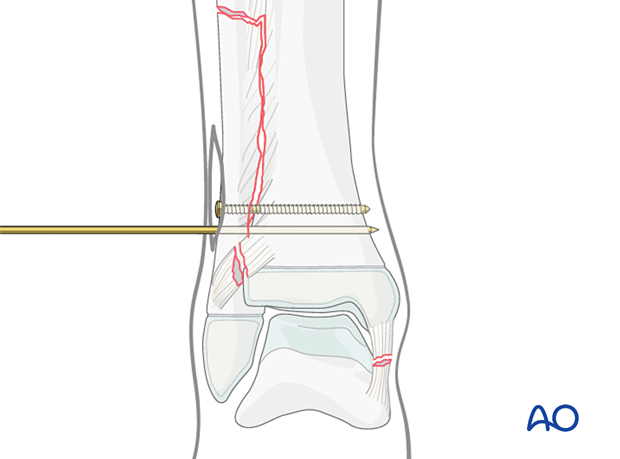
Screw insertion
Use a depth gauge to determine the length of the screw.
As this screw is not intended to act as a compression lag screw, the thread must be tapped in both fibula and tibia.
If non-self-tapping screws are to be used, tap the thread and insert a 3.5 mm cortex screw.
The foot should be in neutral position during insertion of the positioning screw.
Confirm reduction with an image intensifier in both planes.
The reduction must be anatomical and should be confirmed by comparison with images of the uninjured ankle.
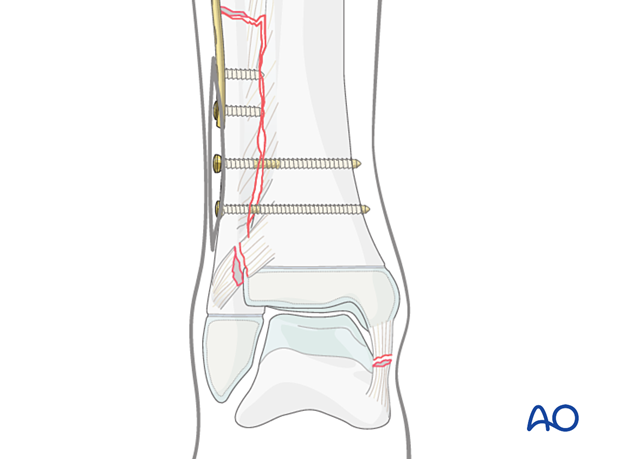
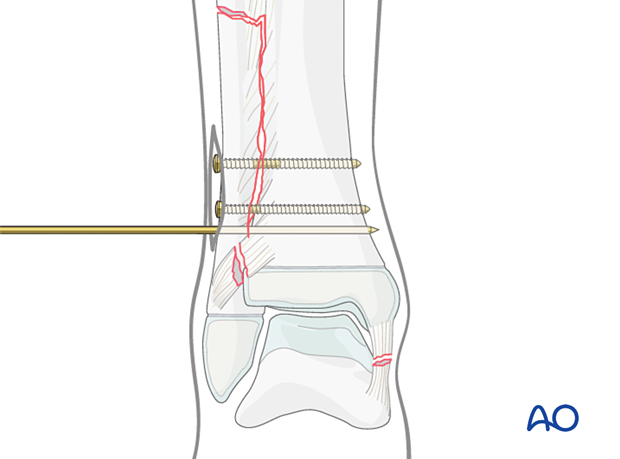
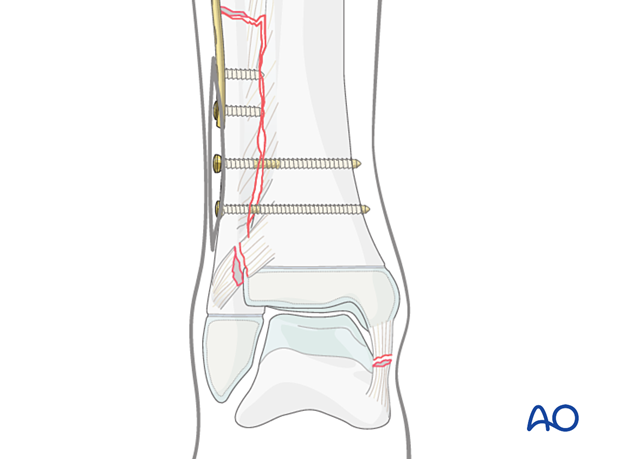
Two small fragment screws can be used to stabilize the syndesmosis, especially in high fibular fractures, such as the Maisonneuve injury.
Prepare and insert the second positioning screw as described above, parallel to and 1.5–2 cm proximal to the first screw.
Once satisfactory reduction and screw placement have been confirmed, remove the K-wire.
Final construct
Confirm the position of the screw and the distal tibiofibular joint with an image intensifier.
7. Treatment of associated high fibular fractures
A high fibular fracture requires direct fixation if the degree of displacement compromises the soft tissues.
The fracture may be fixed with standard techniques for long-bone fracture management, eg, 1/3 tubular plate or 3.5 LCP.
8. Medial collateral (deltoid) ligament reattachment
Skin incision
Center the skin incision on the tip of the medial malleolus.
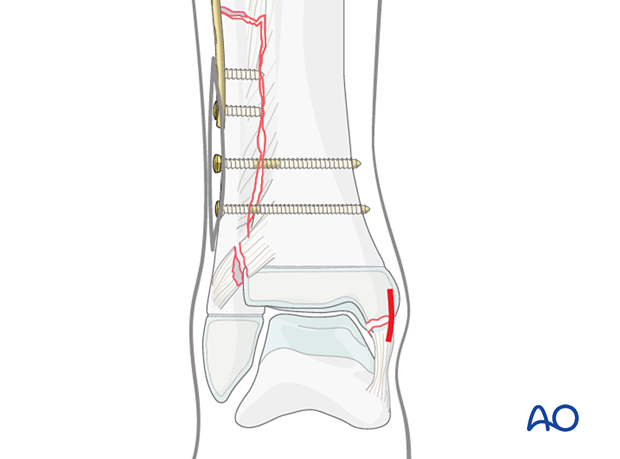
In younger children, the ligament may be repaired with an absorbable suture through the epiphyseal cartilage.
In an older child, use a suture anchor in the medial malleolus.
Check the stability of the fixation by clinical examination and fluoroscopy.
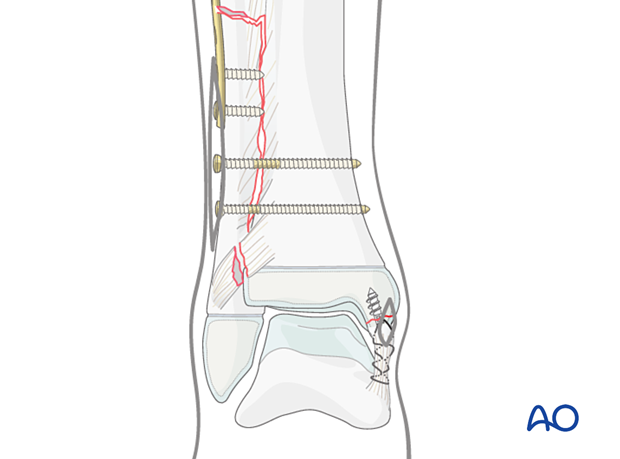
9. Final assessment
Recheck the fracture alignment and implant position clinically and with an image intensifier before anesthesia is reversed.
Confirm stability of the fixation by moving the ankle through a range of dorsi/plantar flexion.
10. Immobilization
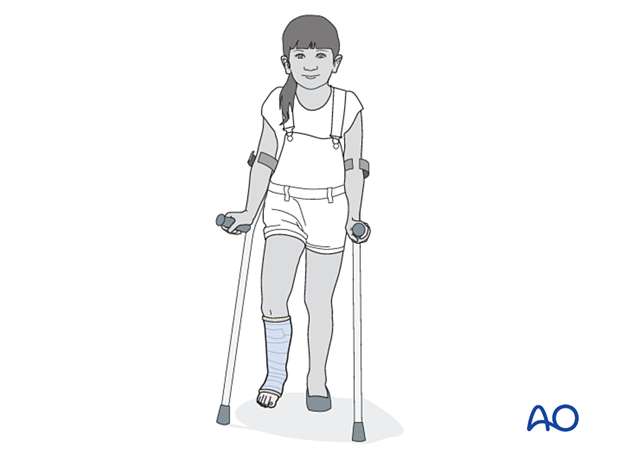
A molded below-knee cast or fixed ankle boot is recommended for a period of 2–6 weeks as the strength of fixation may not provide sufficient stability for unrestricted weight-bearing.
11. Aftercare
Immediate postoperative care
Weight-bearing is encouraged.
Older children may be able to use crutches or a walker.
Younger children may require a period of bed rest followed by mobilization in a wheelchair.
Pain control
Patients tend to be more comfortable if the limb is splinted.
Routine pain medication is prescribed for 3–5 days after surgery.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Discharge care
Discharge follows local practice and is usually possible within 24–48 hours.
Follow-up
The first clinical and radiological follow-up is usually undertaken 5–7 days after surgery to check the wound and confirm that reduction has been maintained.
Cast removal
A cast or boot can be removed 2–6 weeks after injury.
Mobilization
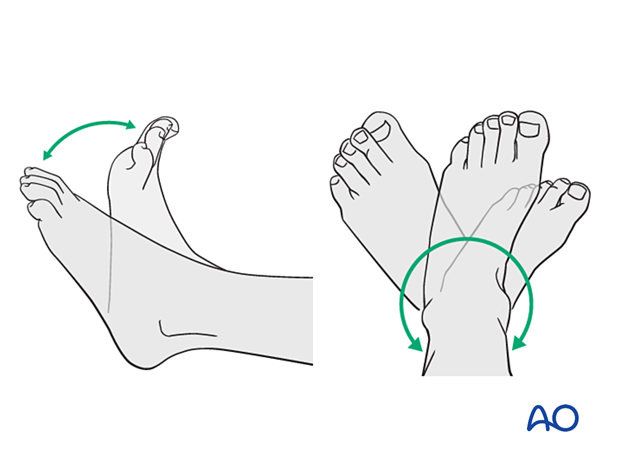
After cast removal, graduated weight-bearing is usually possible.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be required in some cases but is not mandatory.
Sports and activities that involve running and jumping are not recommended until full recovery of local symptoms.
Implant removal
To prevent screw breakage, the syndesmotic screws are typically removed 2–3 months after placement.













