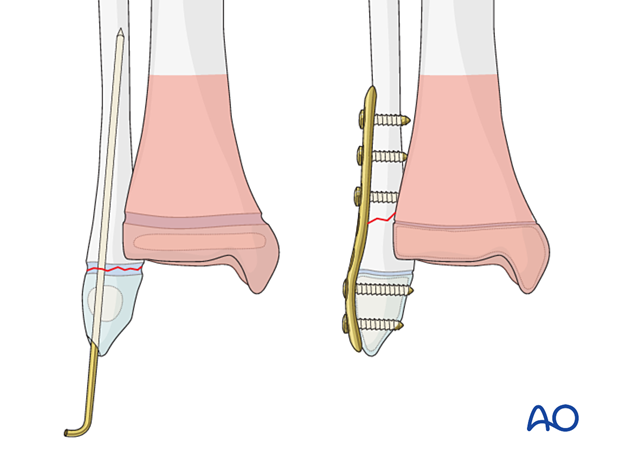
Open reduction; screw fixation
1. General considerations
Introduction
Fractures or avulsions of the medial malleolus that do not involve the physis require open reduction if the fragment is:
- Displaced
- Sufficiently large to allow surgical stabilization.
Although rare, these fractures may be encountered in isolation or in combination with other bony or soft-tissue injuries.
Screw fixation may be performed with a headless compression screw (shown in this procedure) or a cannulated lag screw. K-wire fixation may be sufficient in younger, smaller patients.
The screw may cross the physis in skeletally mature patients.
Associated fibular fracture
A fibular fracture often reduces with reduction and fixation of the tibial fracture and does not require separate consideration.
If the alignment and stability of the fibular fracture are unsatisfactory after fixation of the tibial fracture, surgical treatment of the fibular fracture is also required.
Associated syndesmotic injury
Proximal tenderness and swelling may indicate an associated syndesmotic injury, which affects ankle joint stability.
After fixation of the primary tibial fracture, assessment of stability is performed by stressing the fibula under image intensification.
If the syndesmosis remains unstable, transfixation is usually required.
Treatment goals
The main treatment goals of these fractures are:
- Anatomical reduction
- Uncomplicated healing
- No secondary displacement
- Minimize injury to the physis
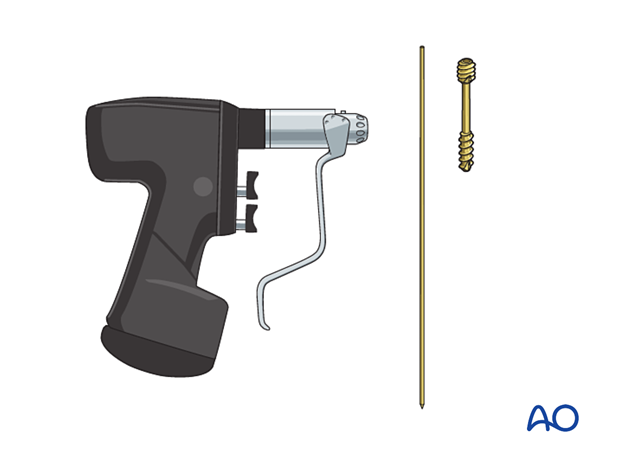
2. Instruments and implants
The screw type should be selected according to the fracture morphology and patient size. A headless compression screw or a solid or cannulated lag screw may be used.
The following equipment is typically used:
- Cannulated or noncannulated screw, or headless screw
- Drill
- Guide wire
- Image intensifier
3. Patient preparation and approach
Patient positioning
Place the patient in a supine position on a radiolucent table with a block under the lower leg proximal to the heel.

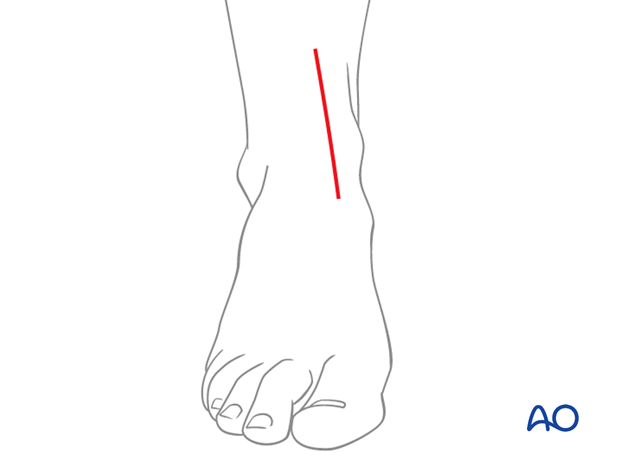
Approach
These fractures are typically treated through an anteromedial approach.
4. Reduction
Remove blood clots, soft callus, and entrapped periosteum.
Insert a smooth 1.5 mm K-wire into the fragment and use it as a joystick for reduction of the fracture and temporary stabilization.
Make sure that it does not interfere with the position of the intended implant.
If the K-wire has the correct diameter, it can also be used as a guide wire for cannulated screw insertion.

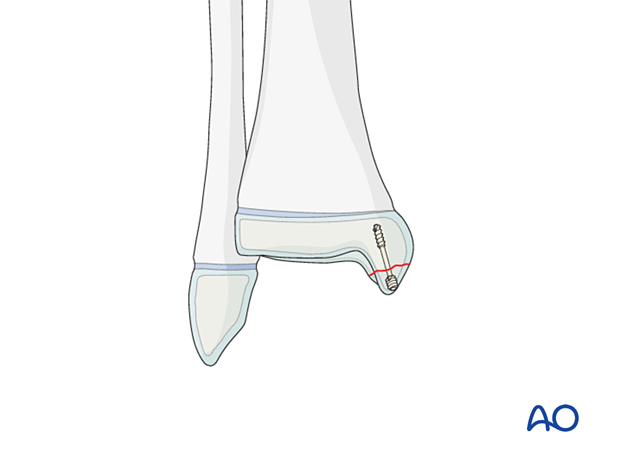
5. Screw fixation
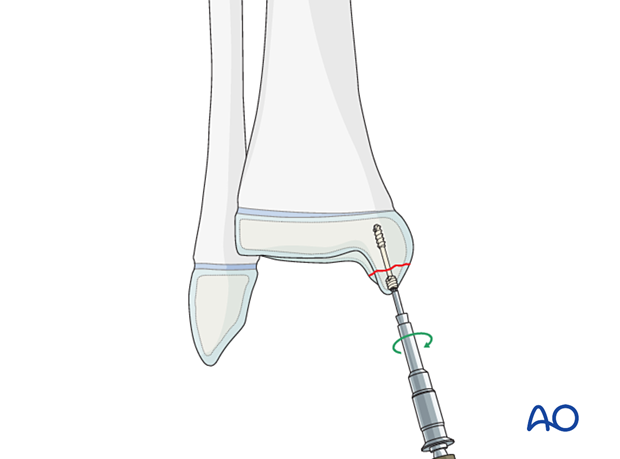
Insert a compression screw after predrilling or over a guide wire in a standard manner.
The screw length should be sufficient to provide adequate compression across the fracture.
The screw should be inserted perpendicular to the fracture plane and, if possible, located within the epiphysis and not crossing the physis.
The screw must be inserted until its head has completely penetrated the cartilage surface.
Confirm reduction, fixation, and stability with an image intensifier.
6. Fibular fracture management
Most fibular fractures do not require treatment. Indications for fixation include:
- Augmentation of the stability of tibial fracture fixation
- Significant displacement of the fibular fracture
The type of fracture pattern dictates the method of fixation of the fibular fracture.
In a younger child, these fractures may be fixed with K-wires in a standard manner. Multiple passes of the K-wire through the physis should be avoided.
In an older patient with a closing physis, these fractures may require plate fixation.
If screws are inserted on both sides of the physis, compression should be avoided and the periosteum and perichondral ring not be disturbed. To protect the perichondral ring, a dissector or elevator may be used to offset the plate during screw insertion. The plate should be removed soon after the fracture has healed.
7. Assessment of the syndesmotic complex
After appropriately stabilizing the tibial fracture, check the stability and reduction of the syndesmotic complex.
Assess AP and lateral translation of the fibula by stressing the ankle joint with a combination of lateral translation and external rotation with an image intensifier. If there is evidence of instability, stabilization of the syndesmosis may be necessary.

8. Final assessment
Recheck the fracture alignment and implant position clinically and with an image intensifier before anesthesia is reversed.
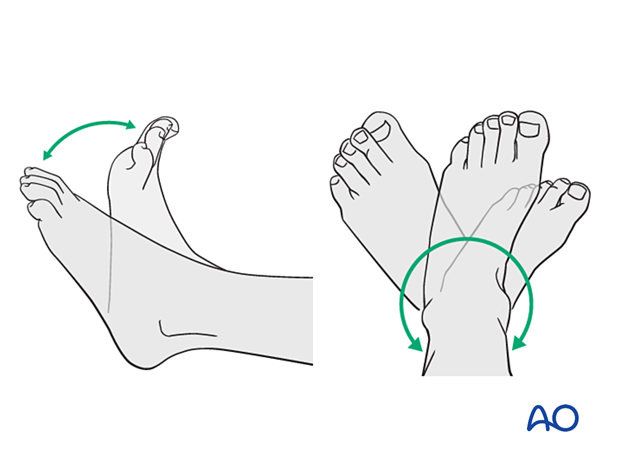
Confirm stability of the fixation by moving the ankle through a range of dorsi/plantar flexion.
9. Immobilization
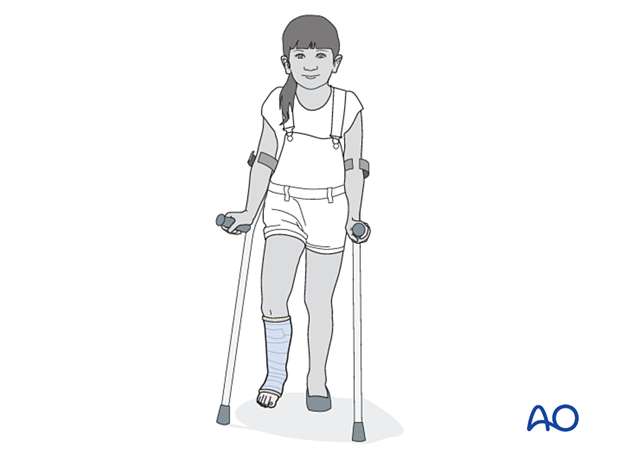
A molded below-knee cast or fixed ankle boot is recommended for a period of 2–6 weeks as the strength of fixation may not provide sufficient stability for unrestricted weight bearing.
10. Aftercare
General considerations
Protected weight-bearing for 3–4 weeks is recommended.
Pain control
Patients tend to be more comfortable if the limb is splinted.
Routine pain medication is prescribed for 3–5 days after surgery.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Discharge care
Discharge follows local practice and is usually possible within 48 hours.
Follow-up
The first clinical and radiological follow-up is usually undertaken 5–7 days after surgery to check the wound and confirm that reduction has been maintained.
Cast removal
A cast or boot can be removed 2–6 weeks after injury.
A screw crossing the physis should be removed as soon as possible after fracture healing.
Mobilization
After cast removal, graduated weight-bearing is usually possible.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be required in some cases but is not mandatory.
Sports and activities that involve running and jumping are not recommended until full recovery of local symptoms.
Implant removal
Implant removal is not mandatory and requires a risk-benefit discussion with patient and carers.













