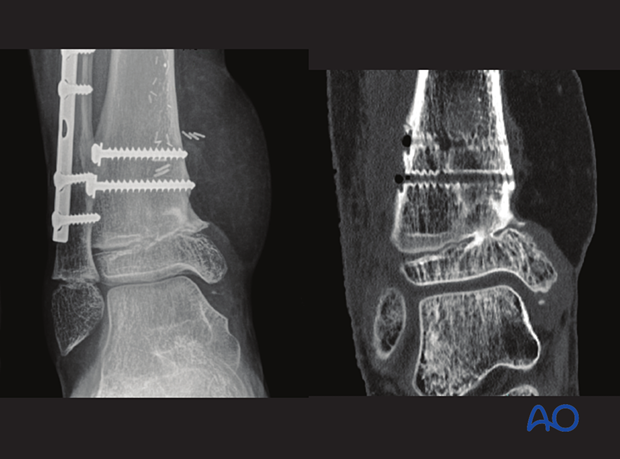
Open reduction; plate fixation
1. General considerations
Introduction
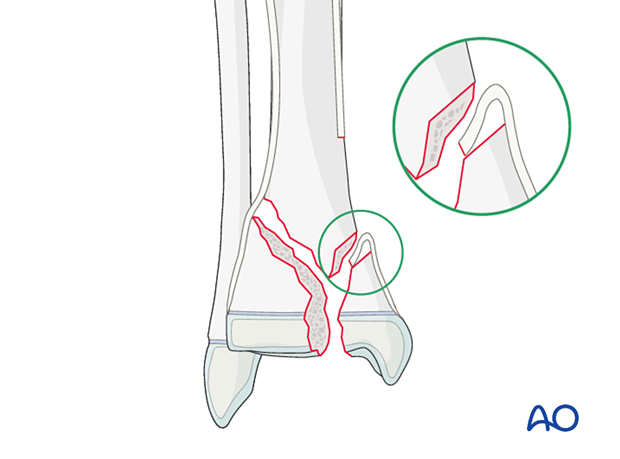
This type of physeal fracture has a high risk of growth disturbance, malunion, and subsequent osteoarthritis. Anatomical restoration of these fractures reduces these risks.
In older/larger patients with a comminuted Salter-Harris IV fracture, a plate may be necessary to provide a stable construct.
In fractures with insufficient distal metaphyseal length, it may be necessary to cross the physis.
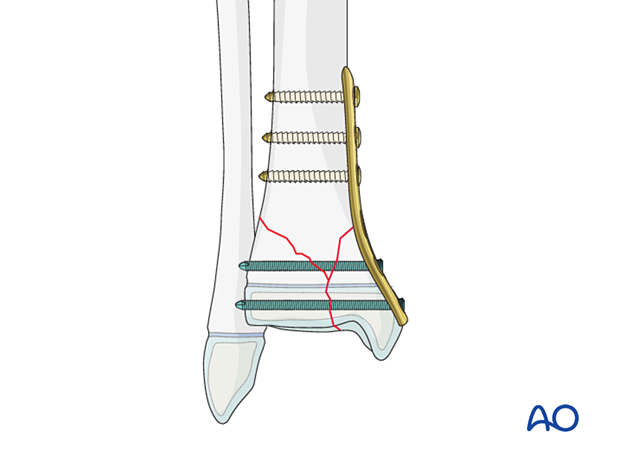
The plate is usually placed on the medial side of the tibia. Due to the lack of muscle coverage in this area, low-profile implants should be used. Avoid plate fixation if the skin is compromised.
In younger patients, crossing the physis will cause a clinically important difference in leg lengths and implant removal is necessary after the fracture has healed.
Associated fibular fracture
A fibular fracture often reduces with reduction and fixation of the tibial fracture and does not require separate consideration.
If the alignment and stability of the fibular fracture are unsatisfactory after fixation of the tibial fracture, surgical treatment of the fibular fracture is also required.
If the distal tibial fracture is highly comminuted, fixation of the fibular fracture may add to overall stability.
Associated syndesmotic injury
Proximal tenderness and swelling may indicate an associated syndesmotic injury, which affects ankle joint stability.
After fixation of the primary tibial fracture, assessment of stability is performed by stressing the fibula under image intensification.
If the syndesmosis remains unstable, transfixation is usually required.
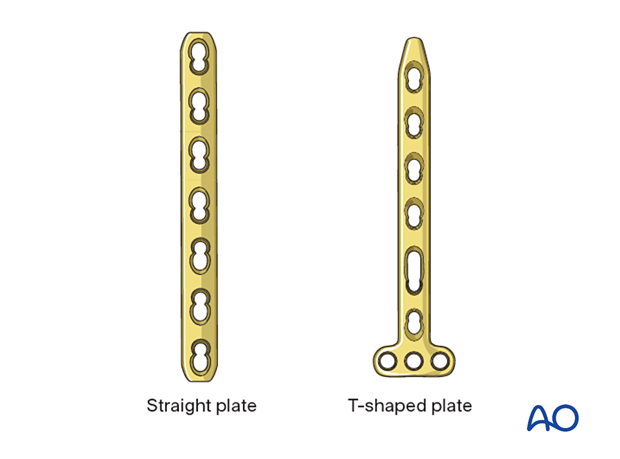
Size and type of implant
2.0–4.5 mm plates are typically used in pediatric practice.
The age and weight of the patient, the anatomical site, and the load to which they will be subjected dictate the size of the implant.
A straight or T-shaped plate can be used.
Adult anatomic plates for the distal tibia are contoured for periarticular placement. If they are applied proximal to the physis, an angular deformity may result.
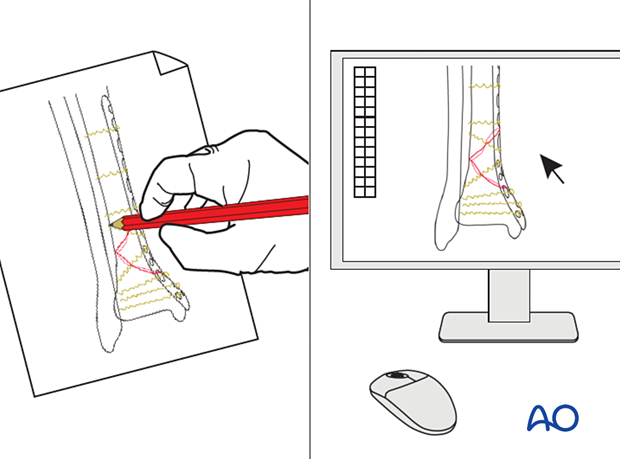
2. Preoperative planning
Preoperative planning is an essential part of the treatment of all distal tibial fractures because of the variability of the fracture pattern and patient characteristics.
This involves:
- Careful study of the x-rays
- Assessment of physis and growth remaining
- Definition of the fracture fragments and the desired result. This may be achieved with appropriate imaging software
- Choice of implants
3. Patient preparation and approach
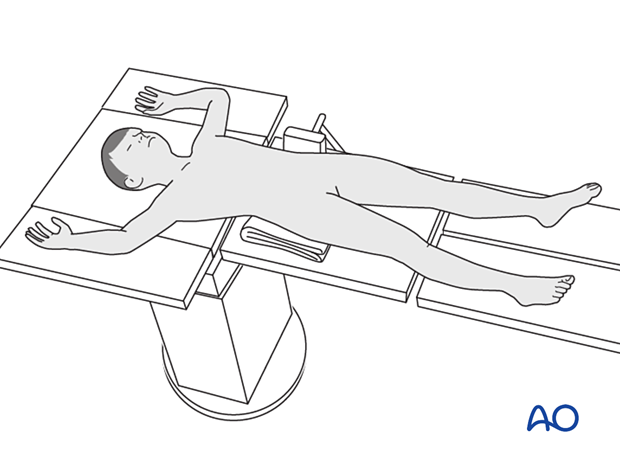
Patient positioning
Place the patient in a supine position on a radiolucent table.
Approach
These fractures are typically managed with an anteromedial approach.
Confirm the location of the physis with an image intensifier and protect the perichondral ring and adjacent periosteum.

4. Reduction
Removal of impediments
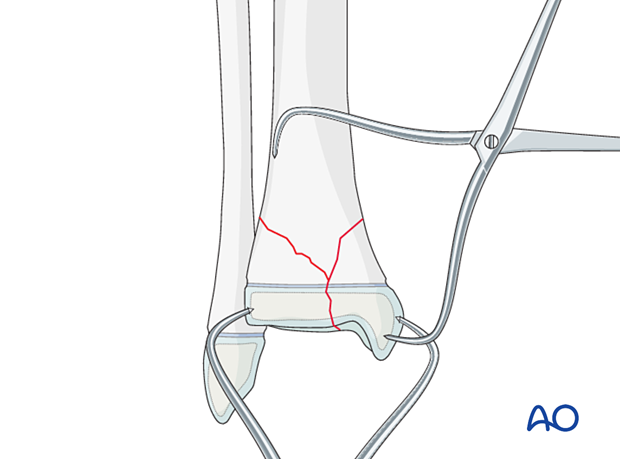
It may be necessary to remove interposed soft tissue and periosteum, without devitalizing the fracture fragments.
This is performed under direct vision, prior to fracture reduction.
Reduction maneuvers
Direct reduction can be performed with:
- Pointed reduction forceps
- A Hohmann retractor, used as a lever to correct translation
- K-wires, used as a joystick to control the distal fragment
If needed, temporarily stabilize the fracture with K-wire(s).
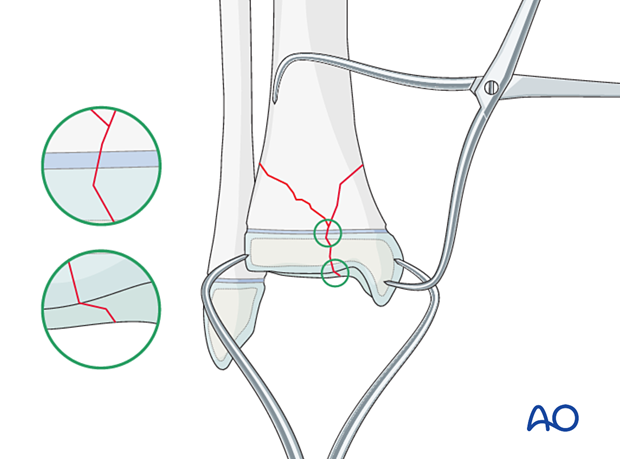
Confirm anatomical reduction of the articular surface visually and of the physis with an image intensifier.
5. Plate fixation
Apply the plate, inserting the distal screw first.
The periosteum and perichondral ring should not be disturbed.
To protect the perichondral ring, a dissector or elevator may be used to offset the plate during screw insertion.
If an anatomical plate is selected, locking screws should be used adjacent to the physis to prevent compression of the perichondral ring.
The dissector or elevator is removed after screw fixation.
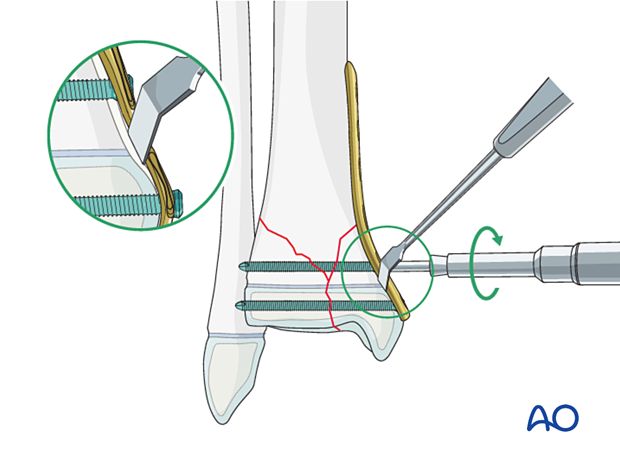
Check the final construct with an image intensifier.
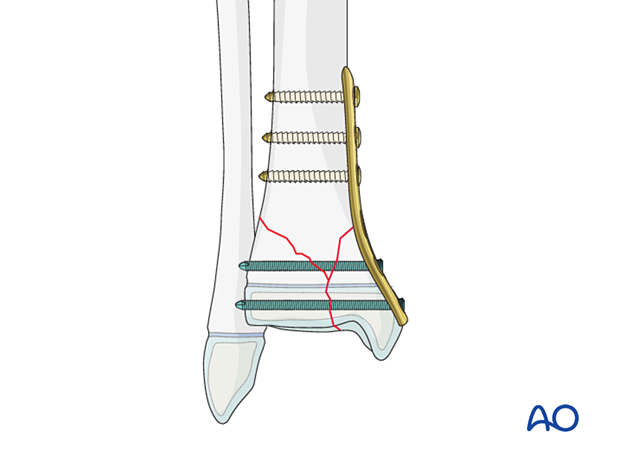
6. Fibular fracture management (Plating)
Most fibular fractures do not require treatment. Indications for fixation include:
- Augmentation of the stability of tibial fracture fixation
- Significant displacement of the fibular fracture
Fibular fractures may be stabilized with plate fixation.
If screws are inserted on both sides of the physis, compression should be avoided and the periosteum and perichondral ring not be disturbed. To protect the perichondral ring, a dissector or elevator may be used to offset the plate during screw insertion. The plate should be removed soon after the fracture has healed.
7. Assessment of the syndesmotic complex
After appropriately stabilizing the tibial fracture, check the stability and reduction of the syndesmotic complex.
Assess AP and lateral translation of the fibula by stressing the ankle joint with a combination of lateral translation and external rotation with an image intensifier. If there is evidence of instability, stabilization of the syndesmosis may be necessary.

8. Final assessment
Recheck the fracture alignment and implant position clinically and with an image intensifier before anesthesia is reversed.
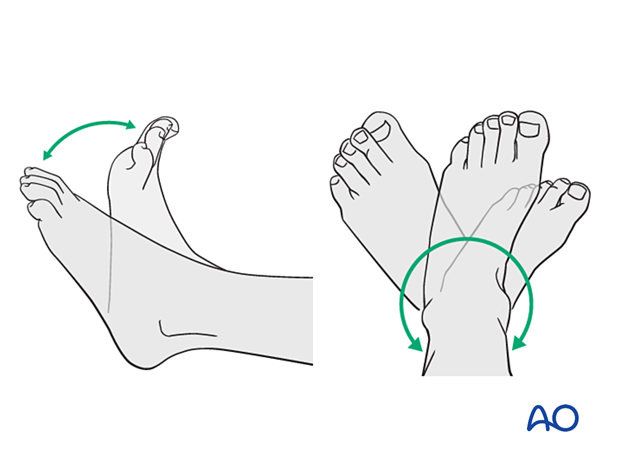
Confirm stability of the fixation by moving the ankle through a range of dorsi/plantar flexion.
9. Immobilization
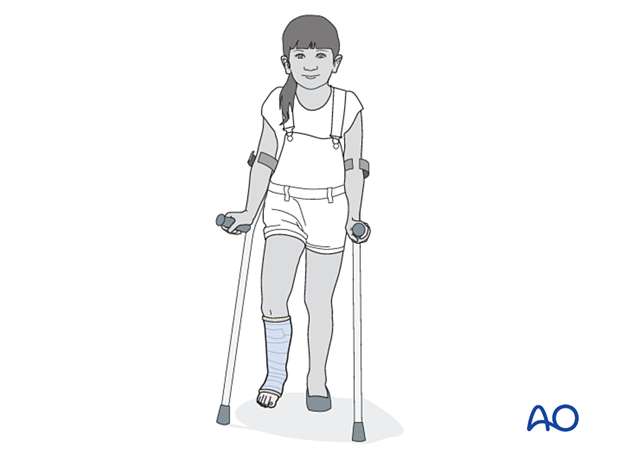
A molded below-knee cast or fixed ankle boot is recommended for a period of 2–6 weeks as the strength of fixation may not provide sufficient stability for unrestricted weight-bearing.
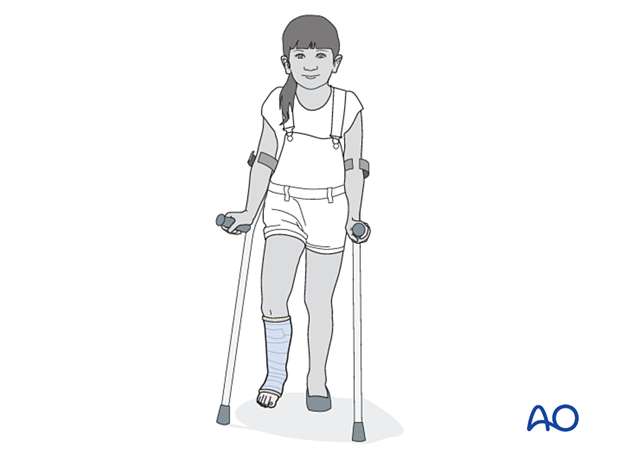
10. Aftercare
Immediate postoperative care
Toe-touch weight-bearing is encouraged.
Elevation is recommended for the first 2–5 days to decrease soft-tissue swelling.
Pain control
Patients tend to be more comfortable if the limb is splinted.
Routine pain medication is prescribed for 3–5 days after surgery.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Discharge care
Discharge follows local practice and is usually possible within 48 hours.
Follow-up
The first clinical and radiological follow-up is usually undertaken 5–7 days after surgery to check the wound and confirm that reduction has been maintained.
Cast removal
A cast or boot can be removed 2–6 weeks after injury.
Mobilization
After cast removal, graduated weight-bearing is usually possible.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be required in some cases but is not mandatory.
Sports and activities that involve running and jumping are not recommended until full recovery of local symptoms.
Implant removal
Implant removal is not mandatory and requires a risk-benefit discussion with patient and carers.
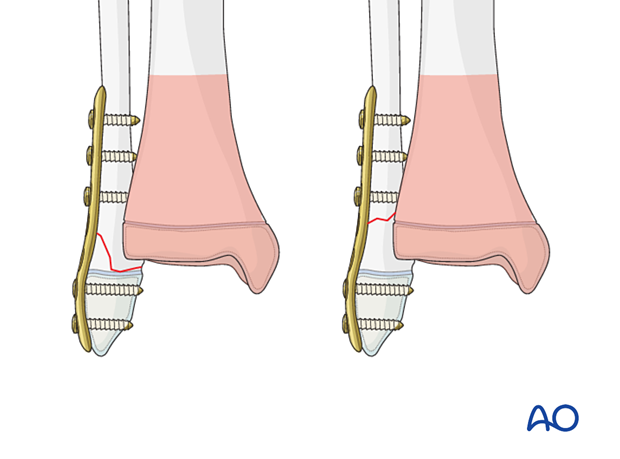
Follow-up for growth disturbance
All patients with distal tibial physeal fractures should have continued clinical and radiological follow-up to identify signs of growth disturbance.
Compare alignment and length clinically with the uninjured leg.
A Harris growth arrest line, parallel to the physis, is radiological evidence of continuation of normal growth.
Recommended reading:
- Nguyen JC, Markhardt BK, Merrow AC, et al. Imaging of Pediatric Growth Plate Disturbances. Radiographics. 2017 Oct;37(6):1791–1812.
Parallel Harris growth arrest line in the distal tibia of a 10-year-old patient, 6 months after injury (right image) excluding a physeal injury
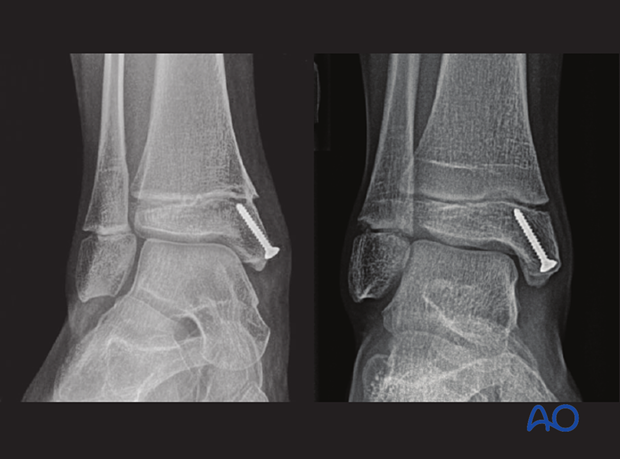
Growth disturbance (convergent Harris growth arrest lines) of an open Salter-Harris II fracture of the distal tibia in a 10-year-old patient, 6 months after injury