Open reduction; K-wire fixation
1. General considerations
Introduction
Displaced articular fractures require an open approach and anatomical reduction to restore the articular surface and align the physis.
The following should be considered to minimize secondary damage to the physis:
- Manipulation of the fracture must be gentle
- Multiple passes across the physis with a K-wire should be avoided
- Select smooth, appropriately sized K-wires
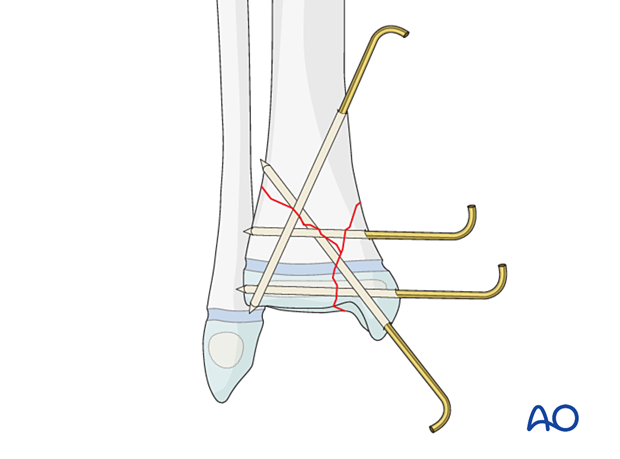
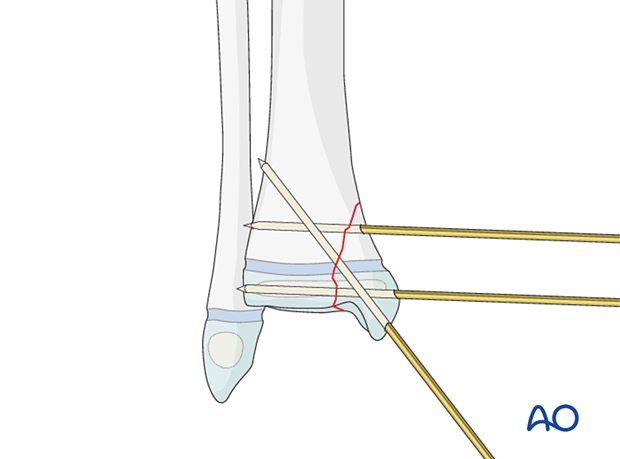
The K-wire construct depends on the fracture morphology and stability. This may include an epiphyseal and a metaphyseal K-wire parallel to the physis and a malleolar K-wire crossing the physis.
The K-wire construct depends on the fracture morphology and stability and usually includes an epiphyseal K-wire, inserted parallel to the physis. If the metaphyseal fragment is sufficiently large, an additional parallel K-wire may also be inserted. A malleolar K-wire crossing the physis adds additional stability.
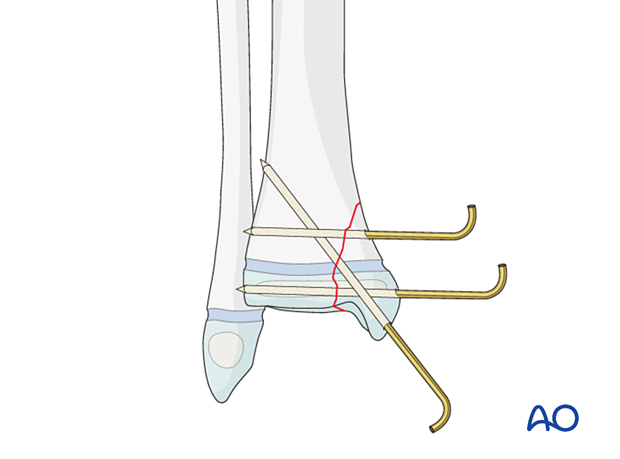
Multifragmentary fractures may require additional K-wire(s).
Associated fibular fracture
A fibular fracture often reduces with reduction and fixation of the tibial fracture and does not require separate consideration.
If the alignment and stability of the fibular fracture are unsatisfactory after fixation of the tibial fracture, surgical treatment of the fibular fracture is also required.
If the distal tibial fracture is highly comminuted, fixation of the fibular fracture may add to overall stability.
Associated syndesmotic injury
Proximal tenderness and swelling may indicate an associated syndesmotic injury, which affects ankle joint stability.
After fixation of the primary tibial fracture, assessment of stability is performed by stressing the fibula under image intensification.
If the syndesmosis remains unstable, transfixation is usually required.
Treatment goals
The goal is to maintain anatomical reduction and stability until healing, without additional damage to the physis.
This type of physeal fracture has a high risk of growth disturbance, nonunion, and subsequent osteoarthritis. Anatomical restoration of these fractures reduces these risks.
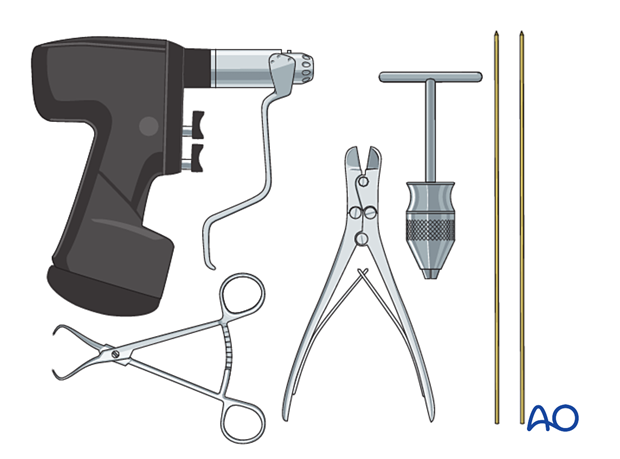
2. Instruments and implants
The following equipment is used:
- K-wires of appropriate sizes
- Drill or a T-handle for manual insertion
- Wire cutting instruments
- Standard orthopedic instrument set
3. Patient preparation and approach
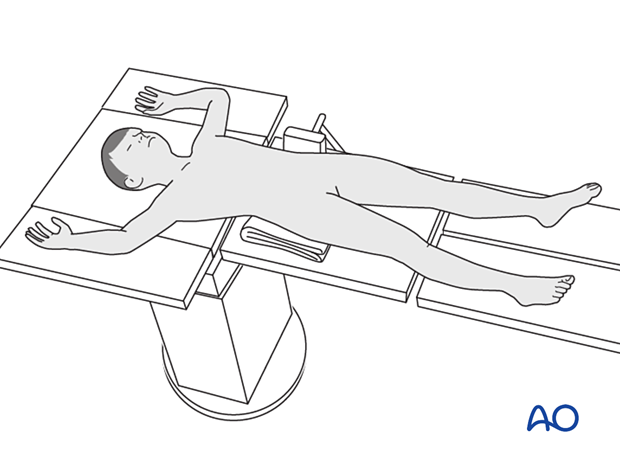
Patient positioning
Place the patient in a supine position on a radiolucent table.
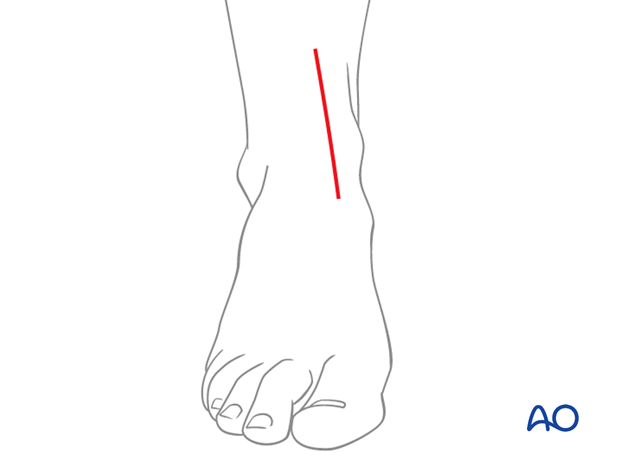
Approach
An anteromedial approach is typically used with an incision that provides sufficient exposure to visualize and reduce the fracture.
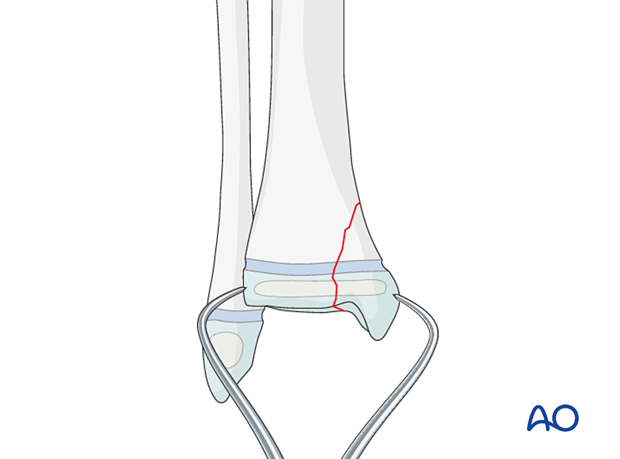
4. Reduction
Remove blood clots, loose fragments, soft callus, and entrapped periosteum.
Reduce the fracture with gentle manipulation, a dental pick, hook, or K-wire.
Hold the reduction with reduction forceps.
Confirm anatomical reduction of the articular surface visually and of the physis and metaphysis with an image intensifier before screw insertion.
5. Fixation
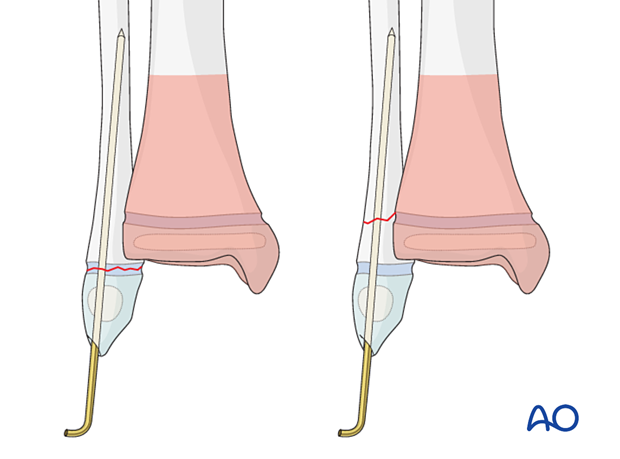
K-wire configuration
The K-wire construct depends on the fracture morphology and stability and includes two or three bicortical smooth K-wires, avoiding multiple passes through the physis.
The K-wires should either be parallel or divergent and not cross at the level of the fracture.
K-wire cutting and dressing
Bend the K-wires approximately 1 cm from the skin to allow for swelling.
Cut the K-wires and apply a dressing to protect the skin.
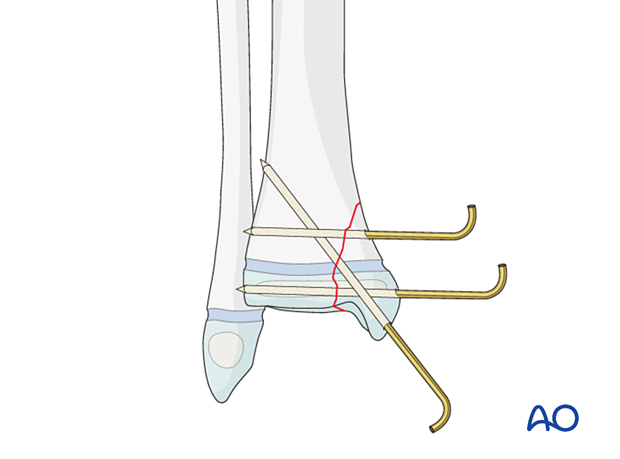
Release tethered skin around the K-wire by extending the incision.
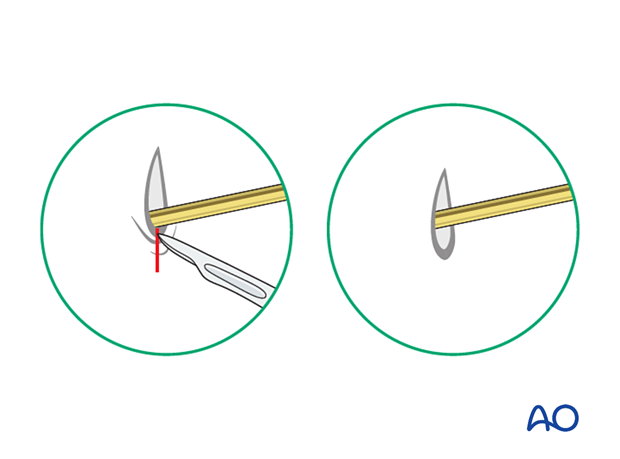
Alternatively, the K-wire may be placed under the skin with the bent end on the surface of the bone.
6. Fibular fracture management
Most fibular fractures do not require treatment. Indications for fixation include:
- Augmentation of the stability of tibial fracture fixation
- Significant displacement of the fibular fracture
The type of fracture pattern dictates the fixation of the fibular fracture.
K-wires are inserted in a standard manner. Multiple passes of the K-wire through the physis should be avoided.
In an unstable tibial eversion fracture, an associated diaphyseal fibular fracture may require plate fixation.
7. Assessment of the syndesmotic complex
After appropriately stabilizing the tibial fracture, check the stability and reduction of the syndesmotic complex.
Assess AP and lateral translation of the fibula by stressing the ankle joint with a combination of lateral translation and external rotation with an image intensifier. If there is evidence of instability, stabilization of the syndesmosis may be necessary.

8. Final assessment
Recheck the fracture alignment and implant position clinically and with an image intensifier before anesthesia is reversed.
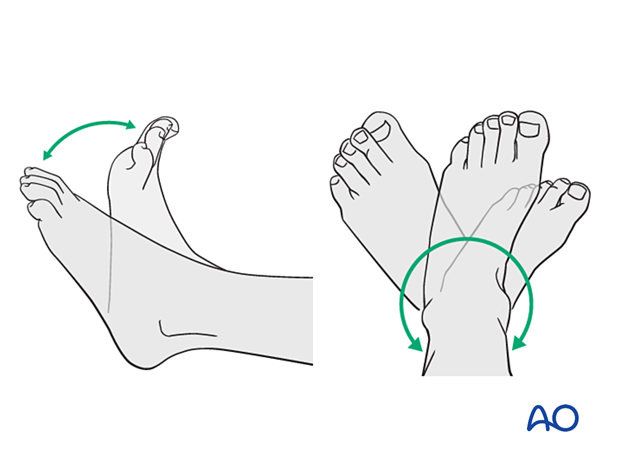
Confirm stability of the fixation by moving the ankle through a range of dorsi/plantar flexion.
9. Immobilization
A molded below-knee cast or fixed ankle boot is recommended for a period of 2–6 weeks as the strength of fixation may not provide sufficient stability for unrestricted weight-bearing.
10. Aftercare
Immediate postoperative care
Non-weight-bearing or touch weight-bearing is encouraged for unstable injuries.
Older children may be able to use crutches or a walker.
Younger children may require a period of bed rest followed by mobilization in a wheelchair.
Pain control
Patients tend to be more comfortable if the limb is splinted.
Routine pain medication is prescribed for 3–5 days after surgery.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Discharge care
Discharge follows local practice and is usually possible within 48 hours.
Follow-up
The first clinical and radiological follow-up is usually undertaken 5–7 days after surgery to check the wound and confirm that reduction has been maintained.
Cast and K-wire removal
Distal tibial and fibular fractures heal rapidly. Cast and K-wires are typically removed 3–6 weeks after injury, depending on the age and weight of the patient.
Mobilization
Once K-wires and cast are removed, gradual weight-bearing is usually possible.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be required in some cases but is not mandatory.
Sports and activities that involve running and jumping are not recommended until full recovery of local symptoms.
Follow-up for growth disturbance
All patients with distal tibial physeal fractures should have continued clinical and radiological follow-up to identify signs of growth disturbance.
Compare alignment and length clinically with the uninjured leg.
A Harris growth arrest line, parallel to the physis, is radiological evidence of continuation of normal growth.
Recommended reading:
- Nguyen JC, Markhardt BK, Merrow AC, et al. Imaging of Pediatric Growth Plate Disturbances. Radiographics. 2017 Oct;37(6):1791–1812.













