Open reduction; plate fixation
1. General considerations
Introduction
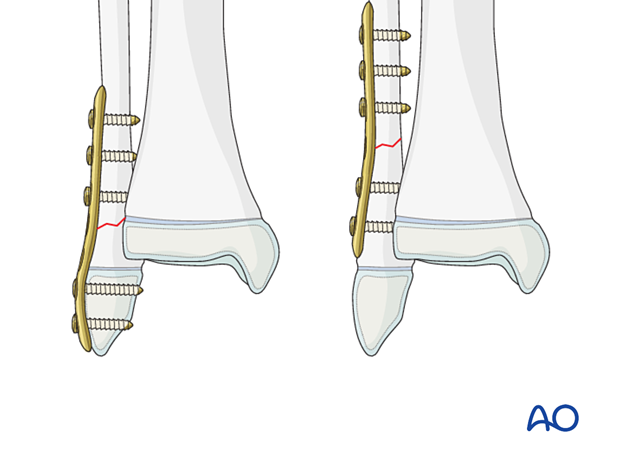
In adolescents close to skeletal maturity, these fractures are reduced and stabilized with a plate using the same principles as adult patients.
The technique depends on the fracture morphology but generally involves bridge plating.
Plating techniques
The technique depends on the fracture morphology and includes:
- Compression plating for transverse or slightly oblique fractures
- Lag screw and neutralization plate for oblique fractures
- Bridge plating for multifragmentary fractures
In fractures with an insufficient metaphyseal fragment, it may be necessary to cross the physis.
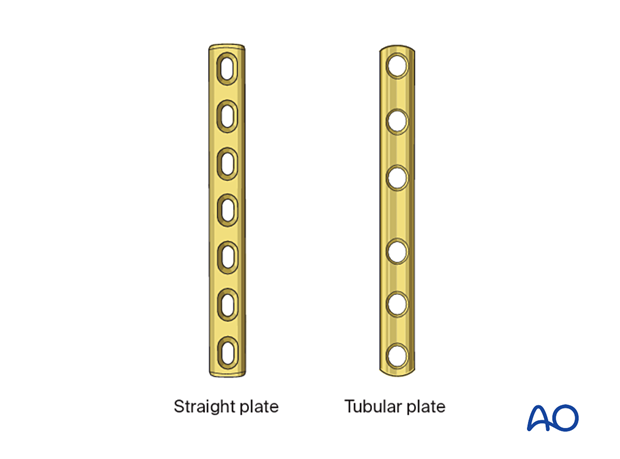
Size and type of implant
The size and type of implant are determined by the size and age of the patient and the fracture pattern. The range of plate sizes in pediatric distal fibular fractures is between 2.4 and 3.5 mm.
2. Patient preparation and approach
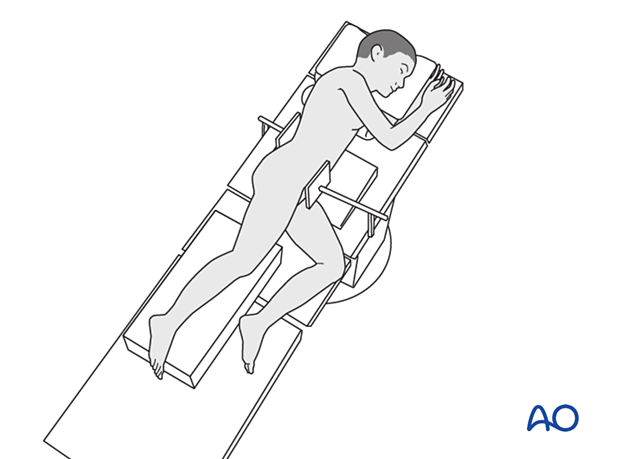
Patient positioning
Place the patient in a lateral decubitus position or supine with a bump under the buttock.
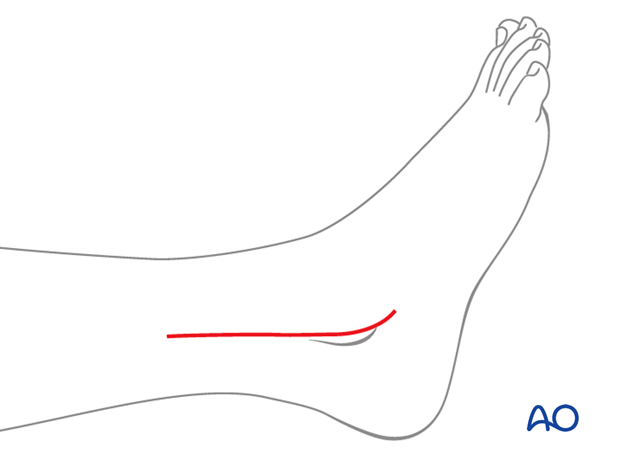
Approach
Most fibular fractures are treated with a lateral incision to visualize the fracture and remove blocks to reduction.
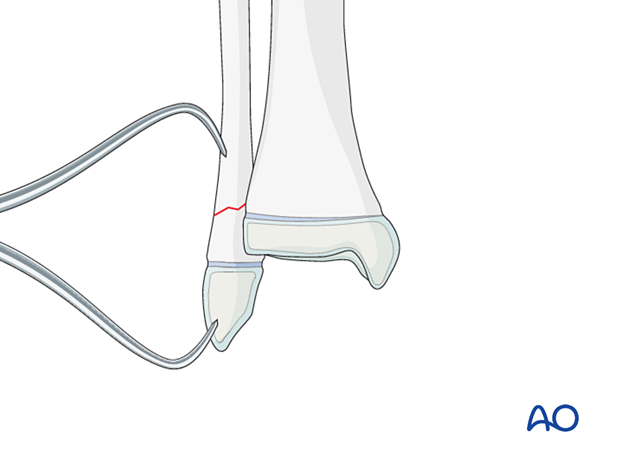
3. Reduction
It may be necessary to remove interposed soft tissue and periosteum without devitalizing the fracture fragments.
Anatomical reduction may require limited dissection of the periosteum adjacent to the fracture site.
This is performed under direct vision before fracture reduction.
Reduce and temporarily hold the fracture with pointed reduction forceps or K-wire.
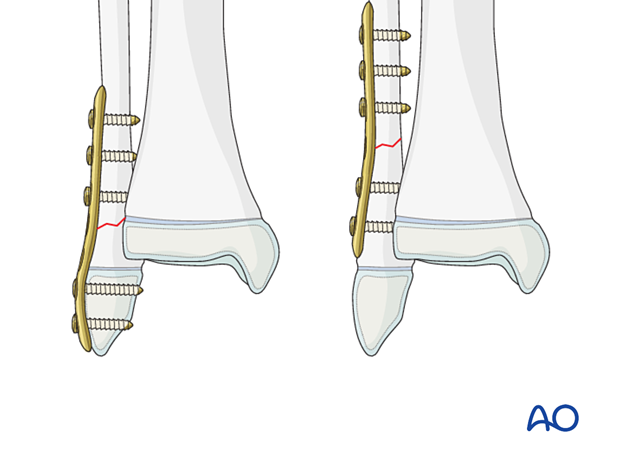
4. Plate fixation
Apply the plate in a standard manner. Simple transverse fractures in the adolescent may require compression.
The order of screw insertion depends on the fracture configuration.
If screws are inserted on both sides of the physis, compression should be avoided. The periosteum and perichondral ring should not be disturbed. To protect the perichondral ring, a dissector or elevator may be used to offset the plate during screw insertion.
5. Final assessment
Recheck the fracture alignment and implant position clinically and with an image intensifier before anesthesia is reversed.
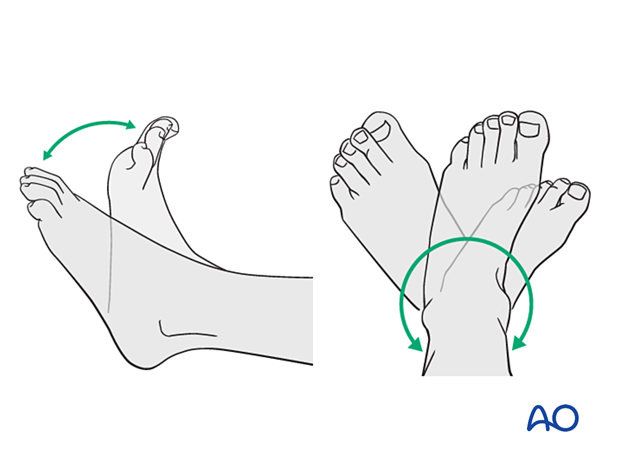
Confirm stability of the fixation by moving the ankle through a range of dorsi/plantar flexion.
6. Immobilization
A molded below-knee cast or fixed ankle boot is recommended for a period of 2–6 weeks as the strength of fixation may not provide sufficient stability for unrestricted weight-bearing.
7. Aftercare
Immediate postoperative care
The patient should get out of bed and begin ambulation with crutches on the day of surgery or the first postoperative day.
In most cases, the postoperative protocol will involve protected weight-bearing in a cast or splint.
Pain control
Patients tend to be more comfortable if the limb is splinted.
Routine pain medication is prescribed for 3–5 days after surgery.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Discharge care
Discharge follows local practice and is usually possible within 48 hours.
Follow-up
The first clinical and radiological follow-up is usually undertaken 5–7 days after surgery to check the wound and confirm that reduction has been maintained.
Cast removal
A cast or boot can be removed 2–6 weeks after injury.
Mobilization
After cast removal, graduated weight-bearing is usually possible.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be required in some cases but is not mandatory.
Sports and activities that involve running and jumping are not recommended until full recovery of local symptoms.
Implant removal
Implant removal is not mandatory and requires a risk-benefit discussion with patient and carers.













