Open reduction; screw fixation
1. General considerations
Introduction
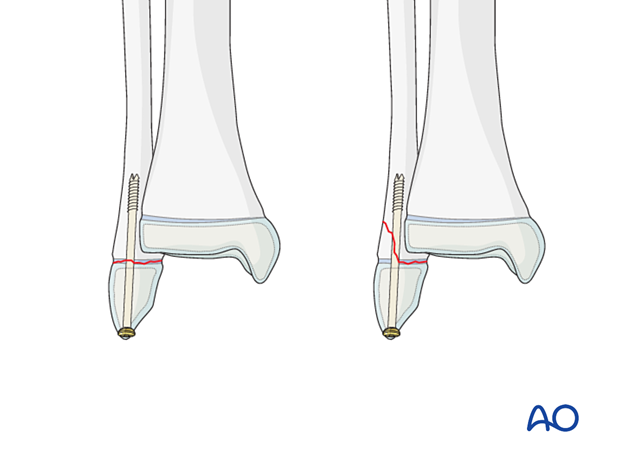
The physeal fragment is fixed with a retrograde intramedullary screw. This risks growth arrest and is only recommended in adolescents.
Open reduction is necessary if it is not possible to obtain or maintain adequate reduction by closed manipulation.
Treatment goals
The main treatment goals are:
- Stabilize the fracture
- Minimize further physeal injury
2. Instruments and implants
Appropriately sized cannulated or noncannulated screws can be used.
The following equipment is used:
- Screw set
- Drill
- Image intensifier

3. Patient preparation and approach
Patient positioning
Place the patient in a supine position on a radiolucent table with a block under the lower leg proximal to the heel.

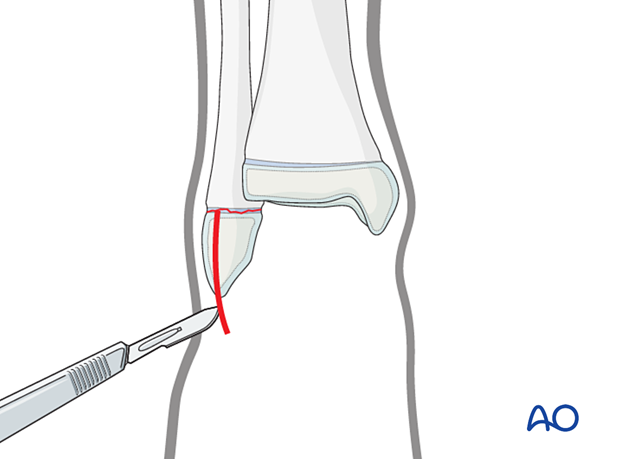
Approach
Perform a lateral incision from just distal to the tip of the fibula to the level of the fracture.
4. Reduction
It may be necessary to remove interposed soft tissue and periosteum before reducing the fracture under direct vision, without devitalizing the fracture fragments.
5. Fixation
Insert a screw in a standard manner.
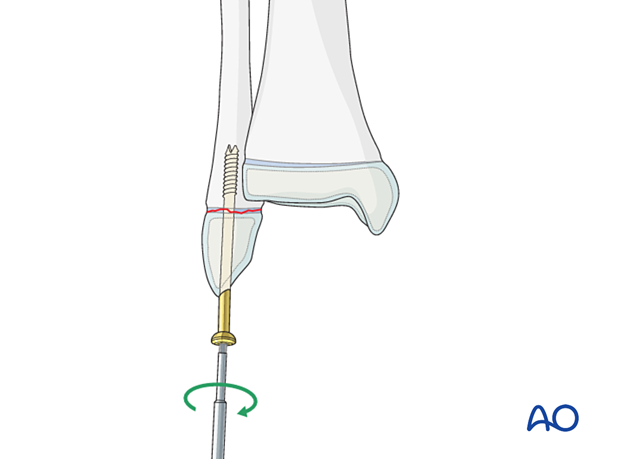
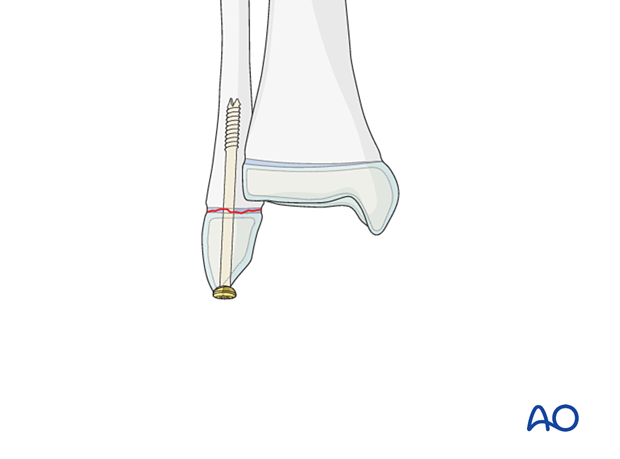
Confirm reduction, fracture stability, and screw placement with an image intensifier.
6. Final assessment
Recheck the fracture alignment and implant position clinically and with an image intensifier before anesthesia is reversed.
Confirm stability of the fixation by moving the ankle through a range of dorsi/plantar flexion.
7. Immobilization
A molded below-knee cast or fixed ankle boot is recommended for a period of 2–6 weeks as the strength of fixation may not provide sufficient stability for unrestricted weight bearing.
8. Aftercare
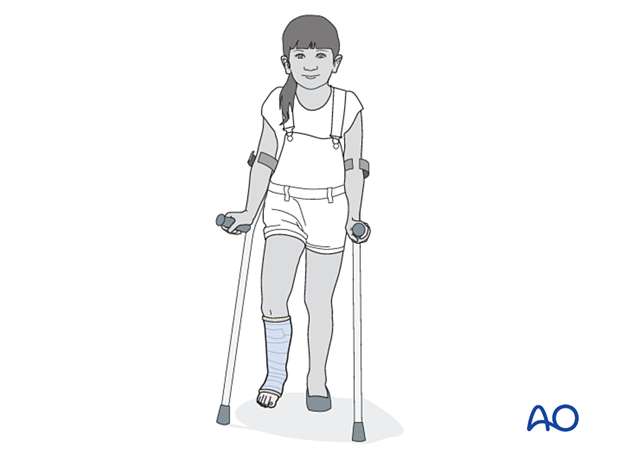
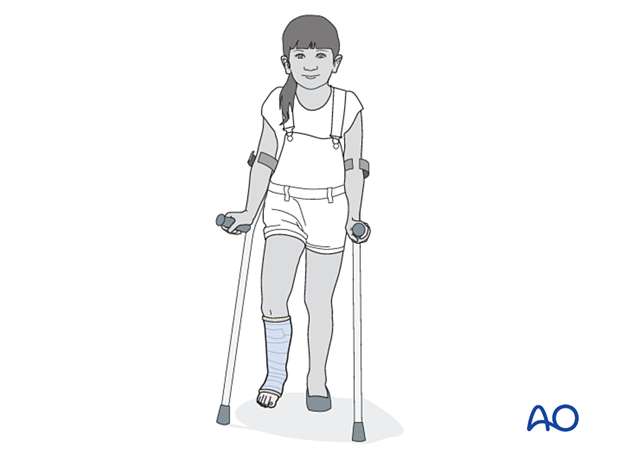
Immediate postoperative care
Weight-bearing is encouraged.
Older children may be able to use crutches or a walker.
Younger children may require a period of bed rest followed by mobilization in a wheelchair.
Pain control
Patients tend to be more comfortable if the limb is splinted.
Routine pain medication is prescribed for 3–5 days after surgery.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Discharge care
Discharge follows local practice and is usually possible within 48 hours.
Follow-up
The first clinical and radiological follow-up is usually undertaken 5–7 days after surgery to check the wound and confirm that reduction has been maintained.
Cast removal
A cast or boot can be removed 2–6 weeks after injury.
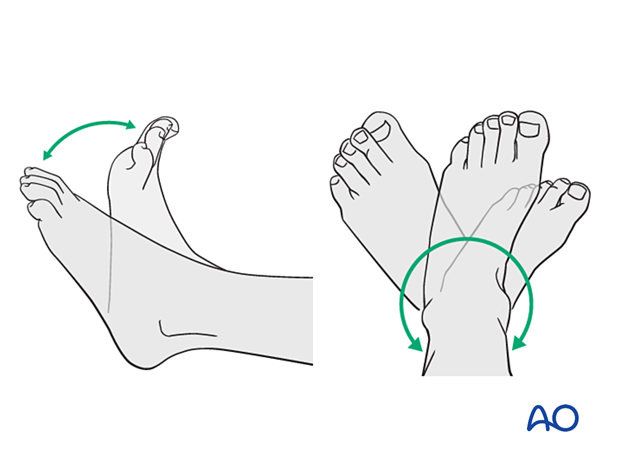
Mobilization
After cast removal, graduated weight-bearing is usually possible.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be required in some cases but is not mandatory.
Sports and activities that involve running and jumping are not recommended until full recovery of local symptoms.
Implant removal
Implant removal is not mandatory and requires a risk-benefit discussion with patient and carers.













