Open reduction; internal fixation
1. Principles
Introduction
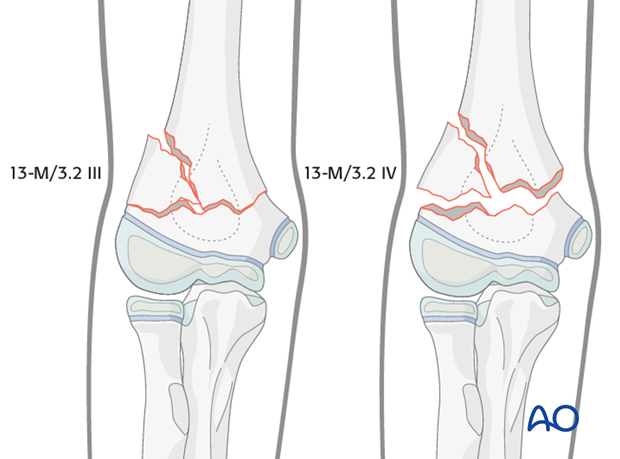
Minor comminution is common. Significant comminution is rare, particularly in younger children.
Closed reduction and percutaneous K-wiring therefore, usually result in accurate reduction and stability. The technique described for single fractures (13-M/3.1 III and 13-M/3.1 IV) is used.
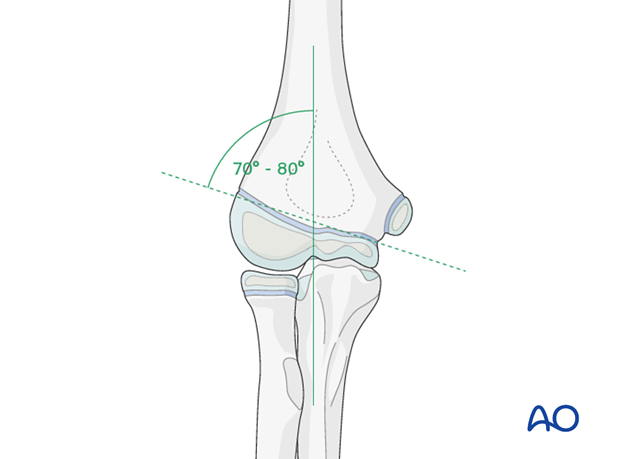
If there is medial impaction, particular attention should be paid to restoring Baumann's angle and thereby avoiding varus malposition.
Younger children
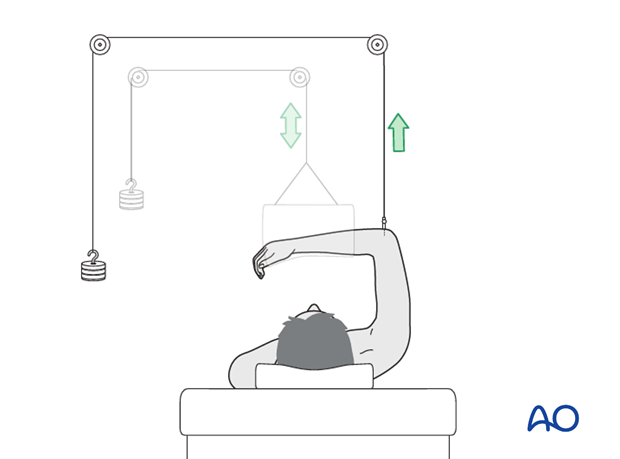
In unusual fractures that are axially unstable, alternative techniques, such as external fixation or overhead olecranon traction, can be applied.
Skeletally immature adolescents
Younger adolescents, with multifragmentary fractures can be managed using approaches described for adults, ie, prone, or lateral, positioning with two column exposure and fixation.
After provisional fixation of both columns with K-wires, the relative stability of the construct can be assessed and decisions about definitive fixation made.
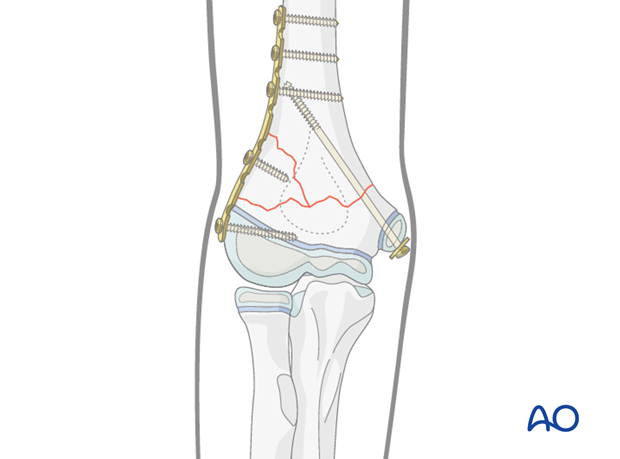
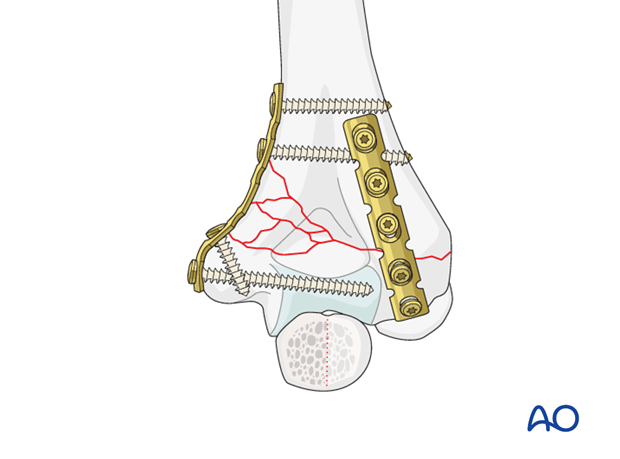
Plate fixation is usually appropriate for the more comminuted column but it is not always necessary to plate both columns.
The noncomminuted column may be treated with K-wires or cannulated screws. This limits dissection and reduces the bulk of implants.
A plate may be used on the noncomminuted column if additional stability is necessary.
Skeletally mature adolescents
High-energy, multifragmentary fractures may occur in skeletally mature adolescents.
These fractures cannot be adequately stabilized with K-wires alone.
The recommended treatment for a completely unstable, adult pattern fracture, involves two plates at right angles, to provide anatomical reduction and allow early motion.
This treatment is appropriate for the older adolescent and the more unstable comminuted fracture pattern.
Please refer to 13-A3.2 fractures in adult AO Surgery Reference.
2. Aftercare
Supracondylar humeral fractures heal rapidly and often within 3–5 weeks.
Immobilization with the elbow in 90° flexion is recommended after surgery until swelling resolves and comfort returns.
Analgesia, including ibuprofen and paracetamol, should be administered regularly.
Compartment syndrome
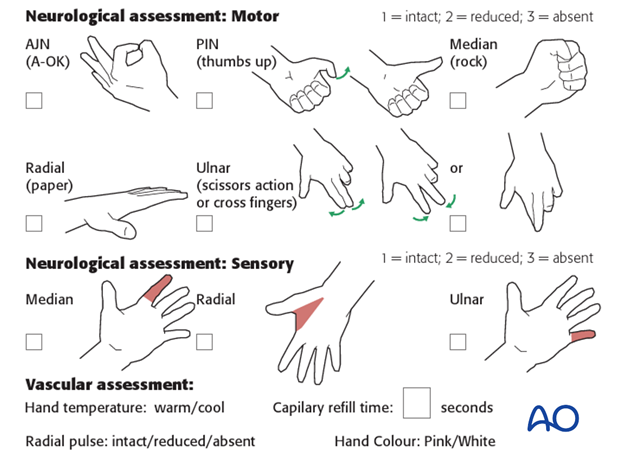
Compartment syndrome is a possible early postoperative complication that may be difficult to diagnose in younger children.
The child should be examined frequently, to ensure finger range of motion is comfortable and adequate.
Neurological and vascular examination should also be performed.
Increasing pain, decreasing range of finger motion, or deteriorating neurovascular signs should prompt consideration of compartment syndrome.
See also the additional material on postoperative infections.
Discharge care
When the child is discharged from the hospital, the parent/caregiver should be taught how to assess the limb.
They should also be advised to return if there is increased pain or decreased range of finger motion.
It is important to provide parents with the following additional information:
- The warning signs of compartment syndrome, circulatory problems and neurological deterioration
- Hospital telephone number
- Information brochure
For the first few days, the elbow and forearm can be elevated on a pillow, until swelling decreases and comfort returns.
At this point, the child may choose to use a sling to support the arm. Many children are more comfortable without a sling.

Follow-up x-rays
Control x-rays may be taken at one week following injury to assess fracture position. Further x-rays may be necessary at three weeks to assess fracture healing. This should be performed after the splint has been removed.
Recovery of motion
As symptoms recover, the child should be encouraged to remove the sling and begin active movements of the elbow.
The majority of elbow motion is recovered rapidly, usually within two months of splint removal. The older child may take a little longer.
Once the child is comfortable, with a nearly complete range of motion, he/she may resume noncontact sports incrementally. Resumption of unrestricted physical activity is a matter of judgment for the treating surgeon.
Implant removal
Implant removal is not mandatory and is a matter for discussion with patient and carer.
Implants are often removed in younger patients but should not be considered until return of a functional range of movement.













