Cast immobilization
1. Goals
The main goals of cast treatment of these fractures are:
- Primary healing
- No secondary displacement
2. Introduction
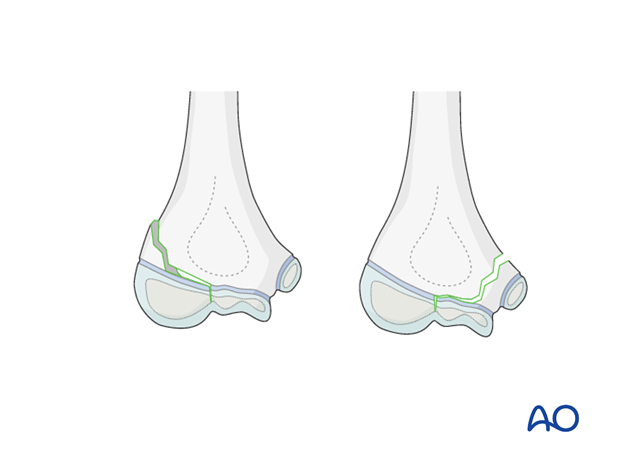
Only undisplaced and stable intraarticular fractures should be treated nonoperatively by plaster cast immobilization. Keep in mind that, for these fractures, the plaster cast cannot hold the fracture in place. It is only an immobilization of the joint.
All nonoperatively treated fractures should be controlled after some days (4-5 days) to identify whether the fracture is stable or not. If the fracture is not stable, operative treatment is required.
In children, it is recommended to immobilize the elbow joint by two splints (posterior and anterior) rather than a single posterior splint. The reason for this is that, when the child is pain-free activity will no longer be naturally restricted and stronger immobilization is required.
Additionally, two splints, as opposed to a full cast, avoid painful and stressful cast removal.
3. Posterior and anterior long arm splints
Preparation of padded splints
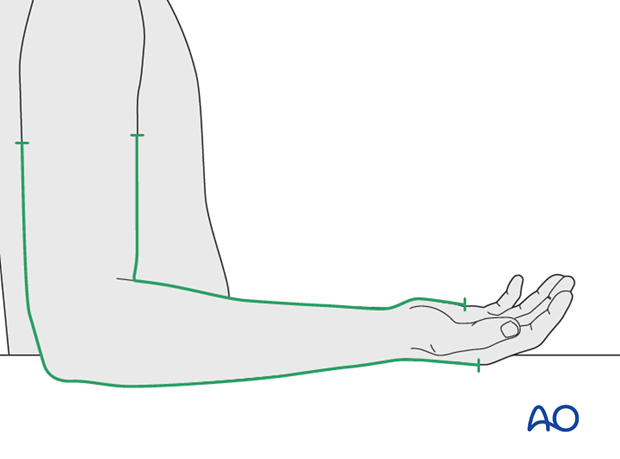
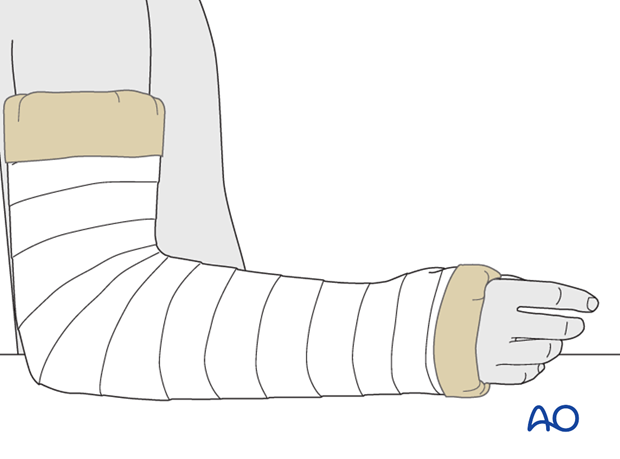
Two splints are prepared according to the correct posterior and anterior lengths. The posterior splint extends from the metacarpal heads to the proximal third of the humerus. The anterior splint extends from the palmar flexor crease to the proximal third of the humerus.
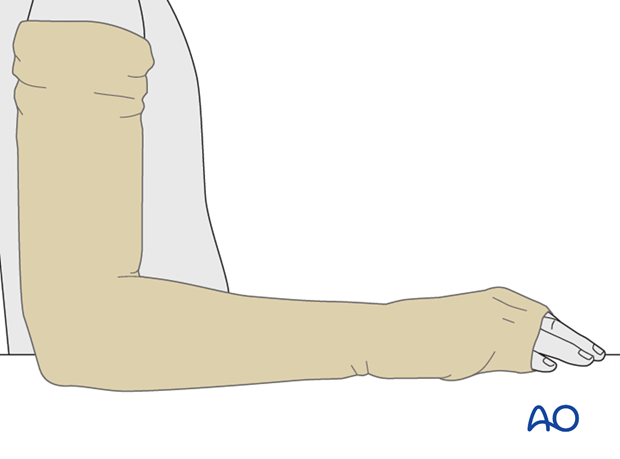
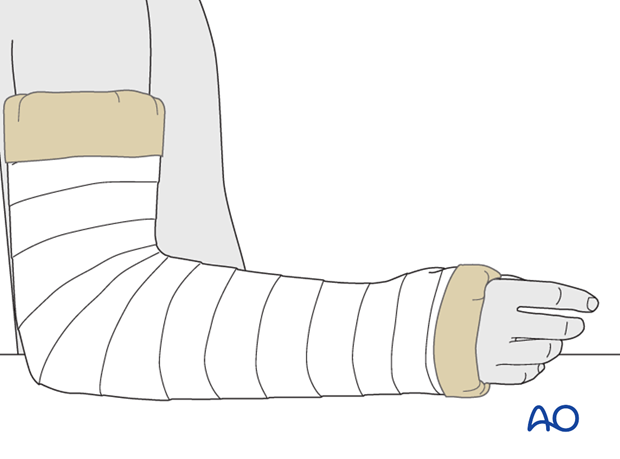
Tubular bandage
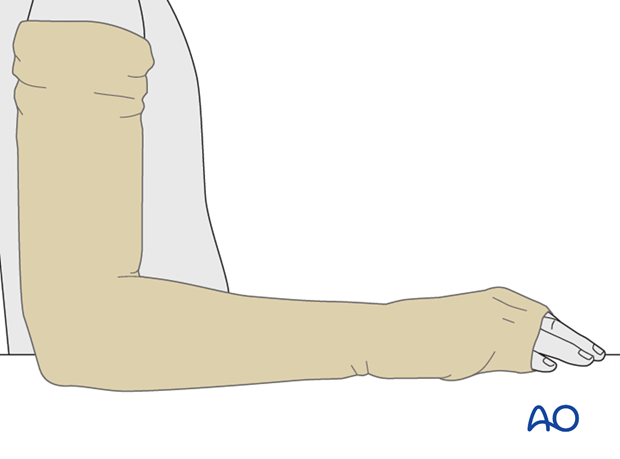
A tubular bandage, extending from the shoulder and over the hand, is applied directly to the skin with a hole cut for the thumb.
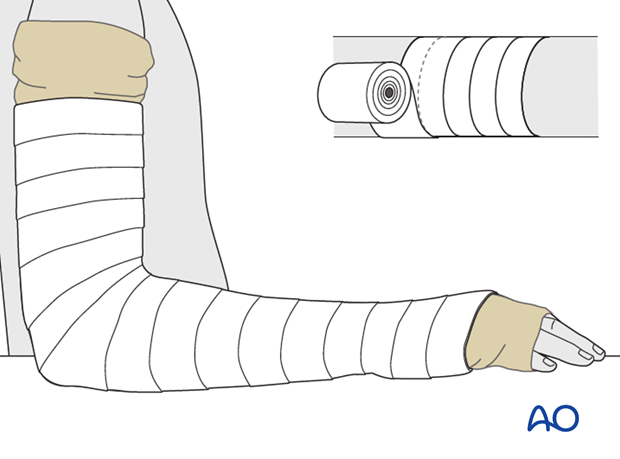
Cast padding
Circular cast padding is applied from the hand to the axilla.
Starting at the hand and moving up to the proximal third of the humerus, the cast padding is applied so that it is overlapping by half the width of the roll.
Alternative: padded splint
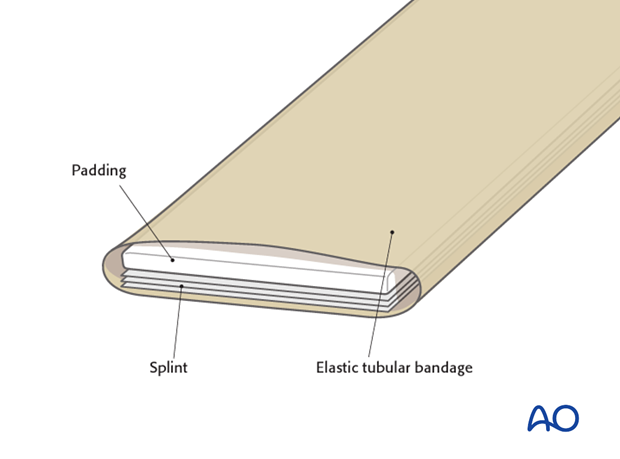
An alternative to a layer of spiral cast padding is to make padded splints as follows.
At least 3-4 layers of padding should be applied under the splint.
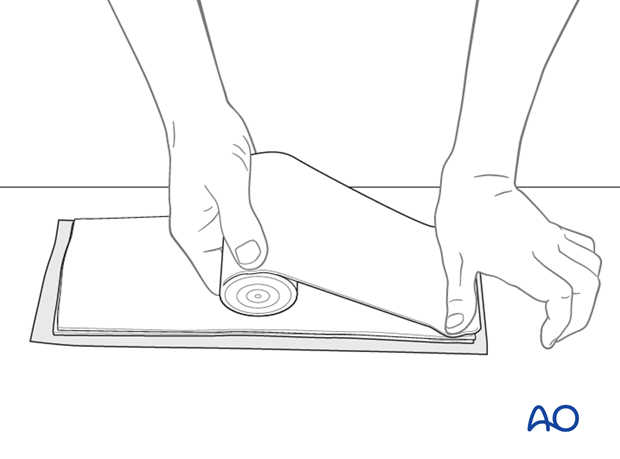
The splint is introduced into an elastic tubular bandage. After moistening the plaster, it can be applied directly to the tubular bandage.
Application of splints
The short splint on the anterior aspect is applied first.
The splint is held at the level of the wrist with two fingers. The long posterior splint is then applied to the hand, forearm and upper arm.
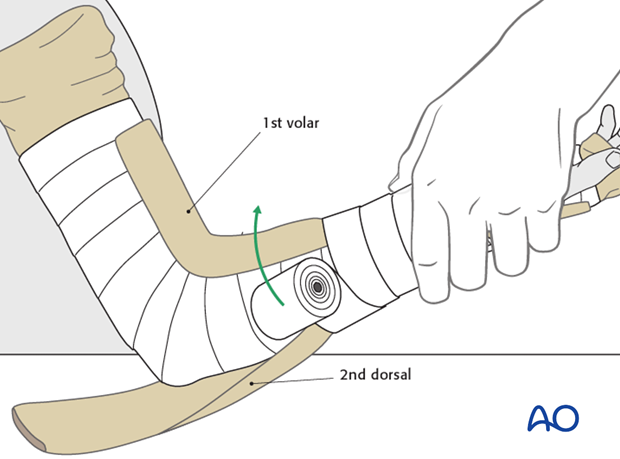
The two splints are held in place with an elastic spiral bandage. The tubular bandage is then folded back over the splints above and below.
4. Circular plaster cast
Tubular bandage
Tubular bandage is applied as described above for the posterior-anterior long arm splints.
Cast padding
Circular cast padding is applied from the metacarpal heads to the axilla.
Starting at the hand and moving up to the proximal third of the humerus, the cast padding is applied so that it overlaps by half the width of the roll.
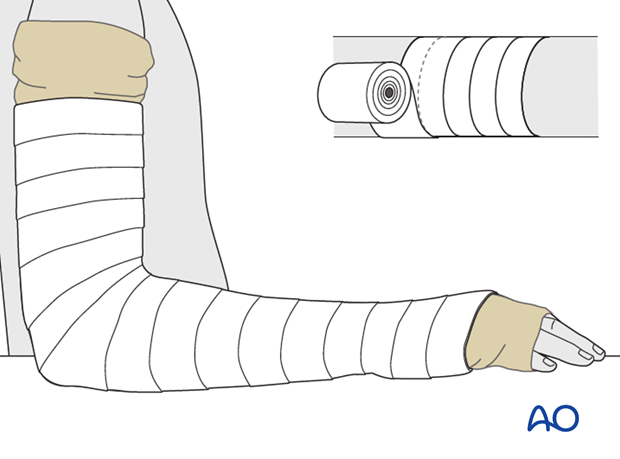
Application of plaster cast
Circular plaster cast is applied in the same way, starting from the hand and going up to the proximal humerus.
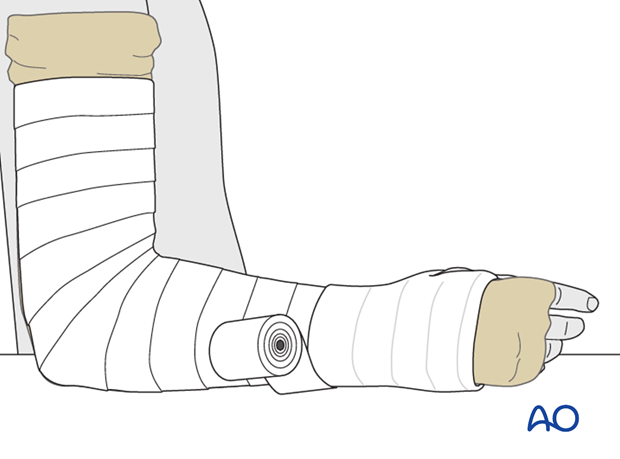
Application of splint
After 2-3 layers of circular plaster cast, it is recommended to apply an additional splint to increase stability.
2-3 more layers of elastic spiral bandage are applied to fix the splint before the plaster cast is finished.
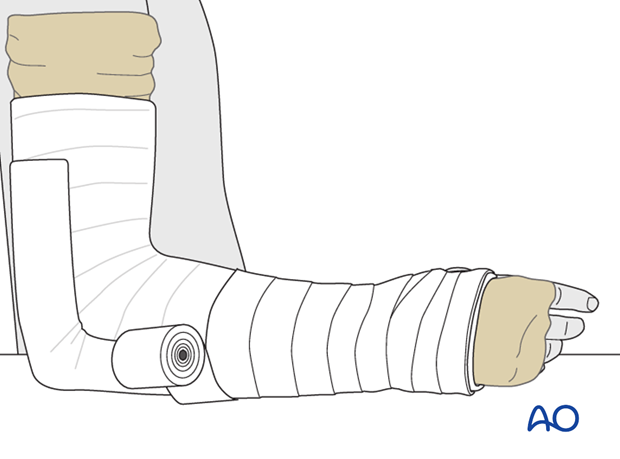
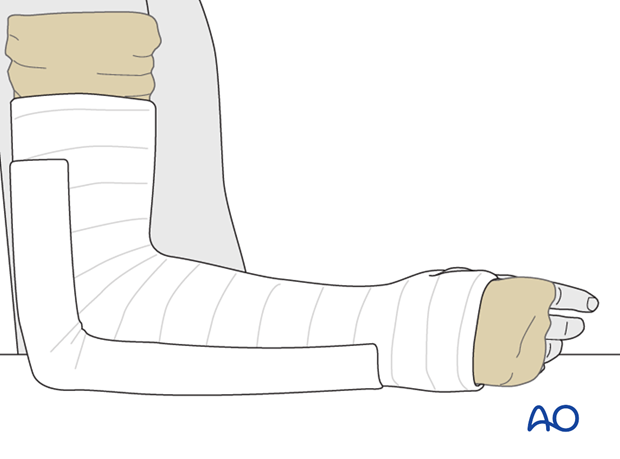
The tubular bandage is folded back over the cast at each end.
5. Aftercare
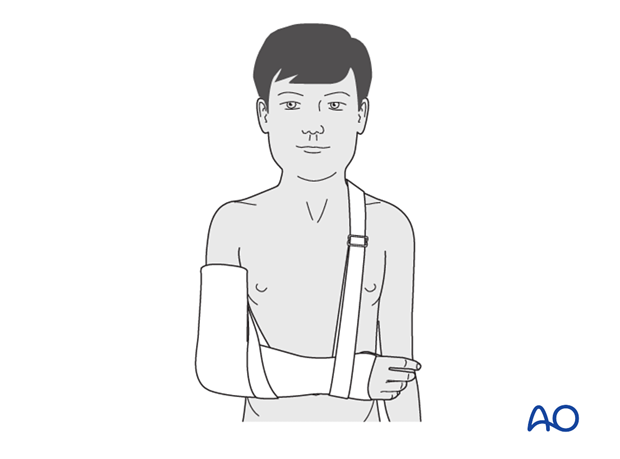
If the child remains for some hours/days in bed, the hand should be held in an elevated vertical position in a roller towel to reduce swelling and pain.

After discharge from hospital, the arm should be held in a sling for immobilization.
Note: In any case of elbow immobilization by plaster cast, careful observation of the neurovascular situation is essential both in the hospital and at home.
See also the additional material on postoperative infection.
It is important to provide parents with the following additional information:
- The warning signs of compartment syndrome, circulatory problems and neurological deterioration
- Hospital telephone number
- Information brochure
Cast removal
Radiological control should be scheduled according to the estimated healing time. The timing of this depends on the age of the child and the type of fracture. Any x-ray to assess healing must be performed out of the cast.
In case of delayed healing, a posterior plaster splint, or manufactured splint, might sometimes be required for an additional 1-2 weeks.













