Excision
1. General considerations
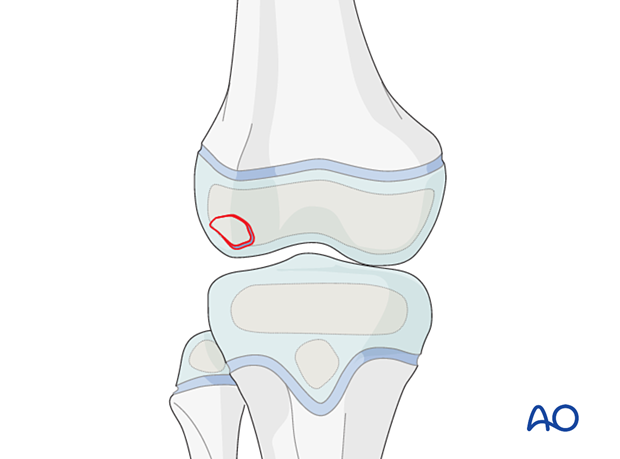
Reconstruction vs excision
A loose small osteochondral fragment in the knee may cause more symptoms than a small articular defect.
Reasonable attempts should be made to repair the articular surface but there may be small osteochondral defects that are not reconstructable.
Specialist techniques to reconstruct the articular surface are available and include osteochondral autograft and allograft transfer.
Associated patellar dislocation
Anterior and lateral osteochondral fractures may be associated with patellar dislocation/subluxation.
Check the retropatellar surface for osteochondral lesions.
2. Patient preparation and approaches
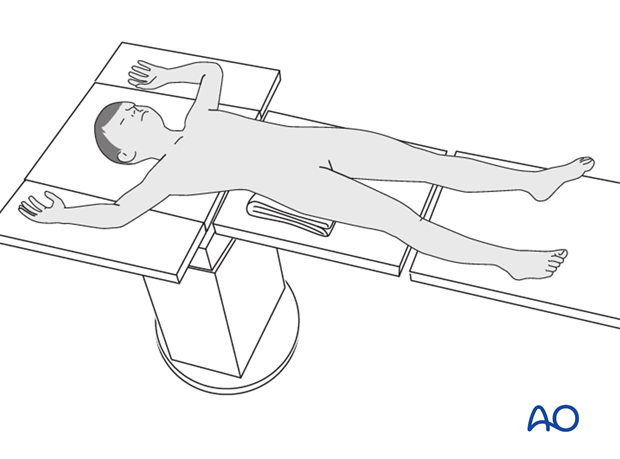
Patient positioning
Place the patient supine on a radiolucent table with a C-arm.
Approaches
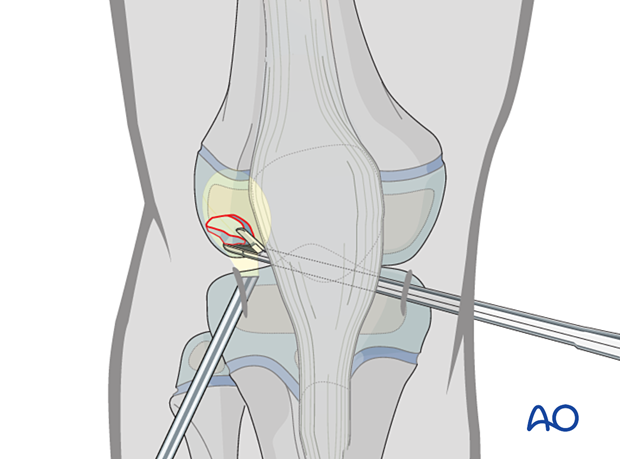
When appropriate resources are available, arthroscopically assisted excision is recommended.
If arthroscopy is not available, osteochondral fractures can be excised via a parapatellar approach.
3. Excision
Fragment removal assisted by arthroscopy
Identify and grasp the fragment under arthroscopic control.
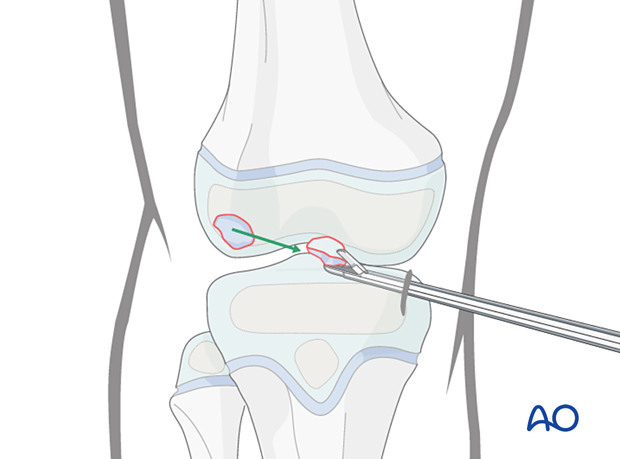
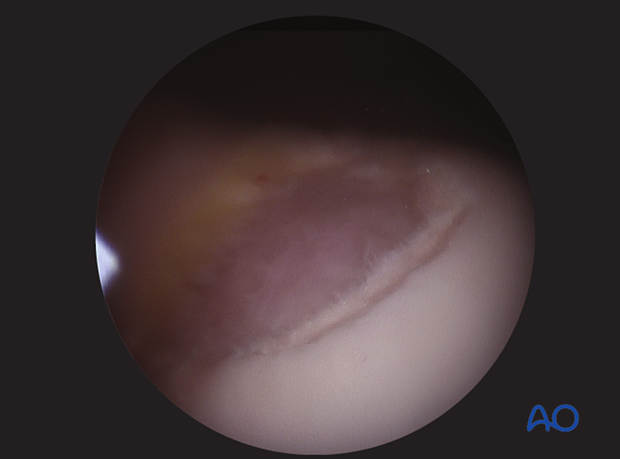
Intraoperative image of articular surface after excision
4. Final assessment
Carefully examine the range of motion and ligament stability.
5. Aftercare
Immediate postoperative care
The patient should get out of bed and begin ambulation with crutches on the day of surgery or the first postoperative day.
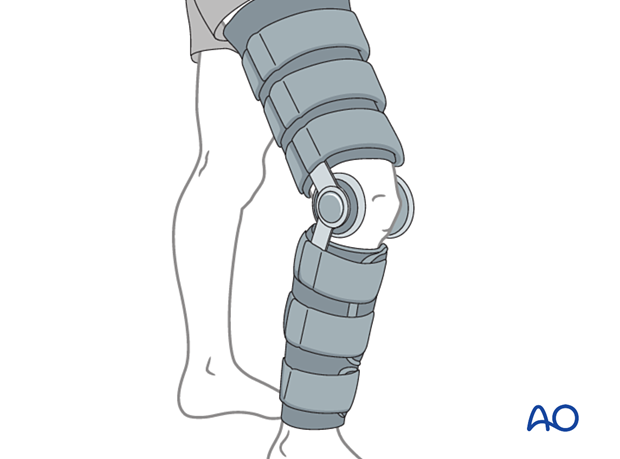
In most cases the postoperative protocol will be protected weight bearing in a hinged knee brace.
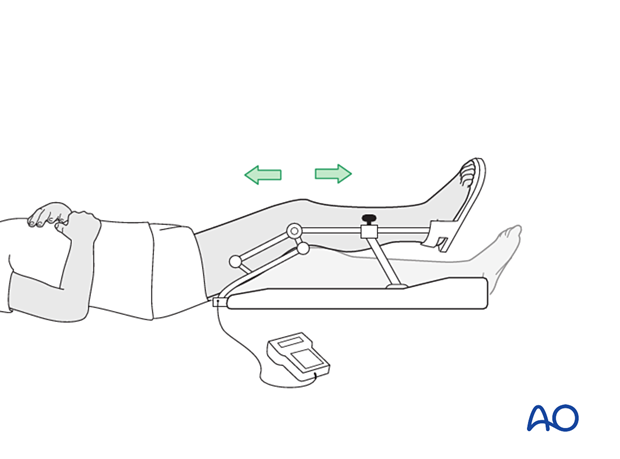
In some situations, the use of continuous passive motion may be useful.
Analgesia
Routine pain medication is prescribed for 3–5 days postoperatively.
Discharge care
Discharge from hospital follows local practice and is usually possible after 1–3 days.
Follow-up
Routine clinical follow-up is undertaken, and physiotherapy may be necessary to accelerate recovery.













