Open reduction; plate fixation
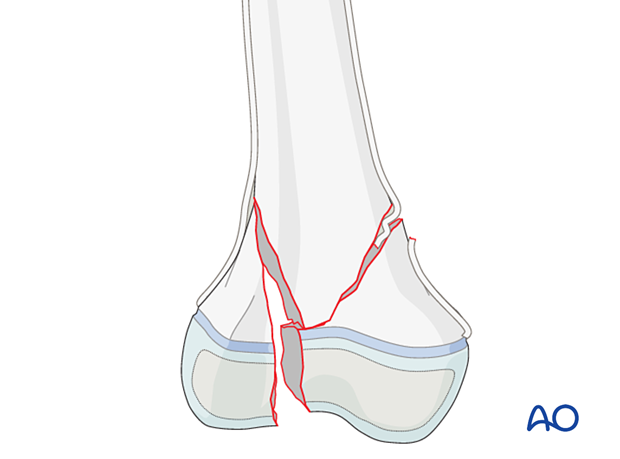
1. General considerations
Principles
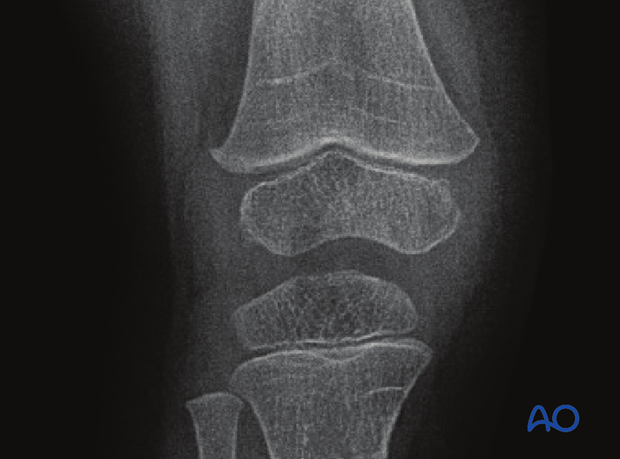
Intraarticular fractures that involve the physis require anatomical reduction and absolute stability.
The articular surface is reduced first and fixed with a screw or a K-wire through the epiphysis.
In some fracture patterns a large metaphyseal fragment is available for fixation and bridging the growth plate is not necessary.
A plate that bridges the growth plate will prevent further longitudinal growth.
In younger patients, this will necessitate early plate removal after fracture union.
In patients close to skeletal maturity, this may not cause a functionally important difference in leg lengths.
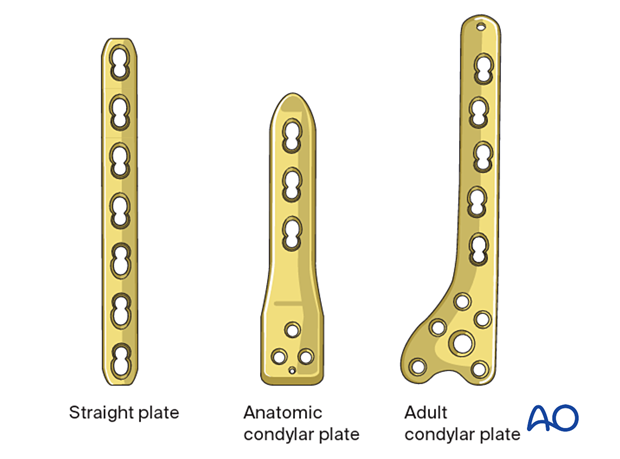
Size and type of implant
The size and type of implant are determined by the size and age of the patient as well as by the fracture pattern. The range of plate sizes in pediatric femur fractures is between 2.7 and 5.0 mm.
There are anatomic condylar plates specifically designed for pediatrics which are also an option.
Adult anatomic plates may be appropriate for patients with a closing growth plate or, in rare cases, where a stable fracture fixation requires sacrificing and bridging of the growth plate.
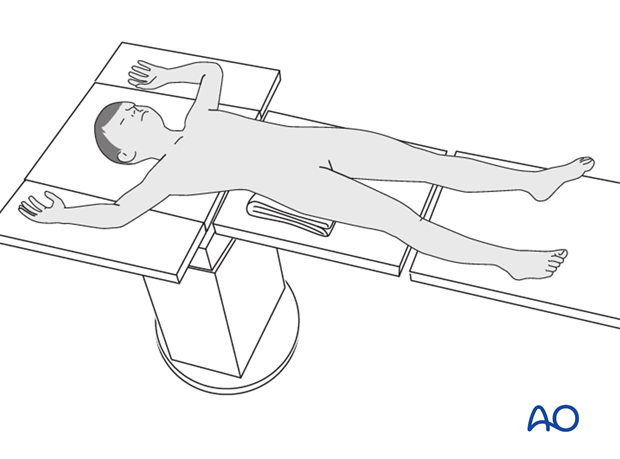
2. Patient preparation and approach
Patient positioning
Place the patient supine on a radiolucent table with a C-arm.
Approach
The majority of the fractures are approached using the distal component of a direct lateral incision.
Confirm the location of the growth plate with image intensification and protect it, taking care not to strip the adjacent periosteum.

3. Reduction and fixation of the articular fracture
Removal of impediments
It may be necessary to remove interposed soft-tissue and periosteum prior to reduction of the fracture under direct vision.
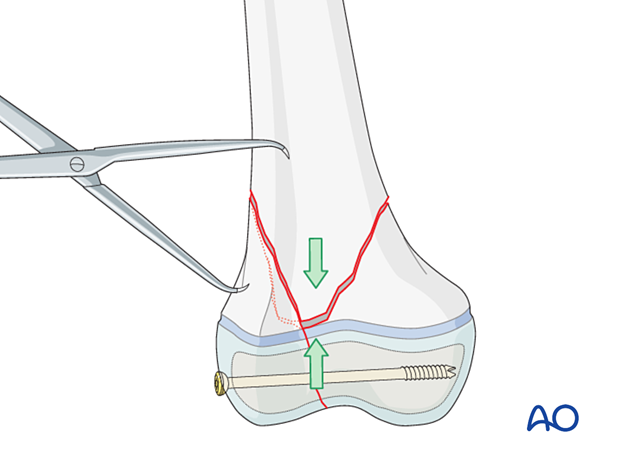
Reduction
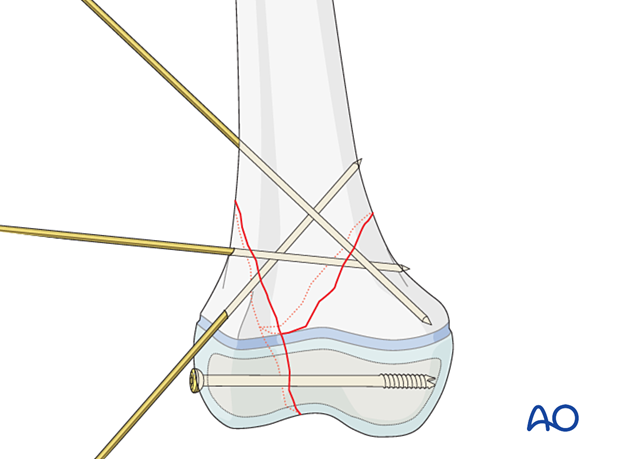
Reduce and hold the epiphyseal fracture with forceps.
Insert a K-wire in the epiphysis parallel to the growth plate to temporarily fix the fracture.
Confirm anatomical reduction with image intensification.
Planning for screw insertion
The epiphyseal fracture may be stabilized with a separate screw.
The position of this screw should not interfere with the planned plate placement.
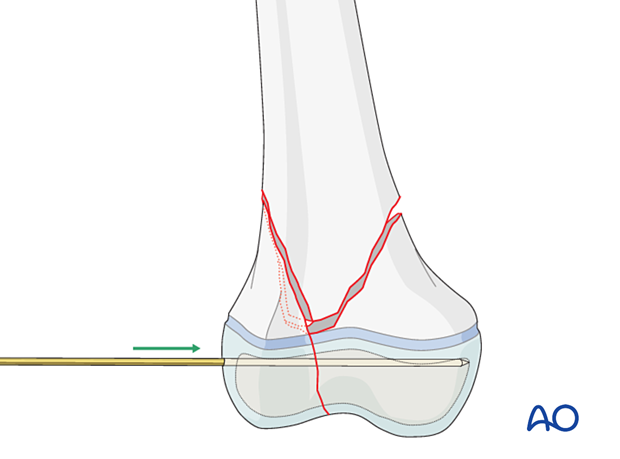
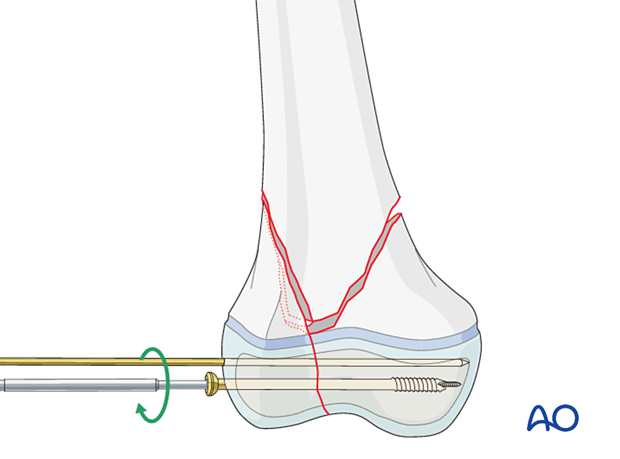
Insertion of guide wire
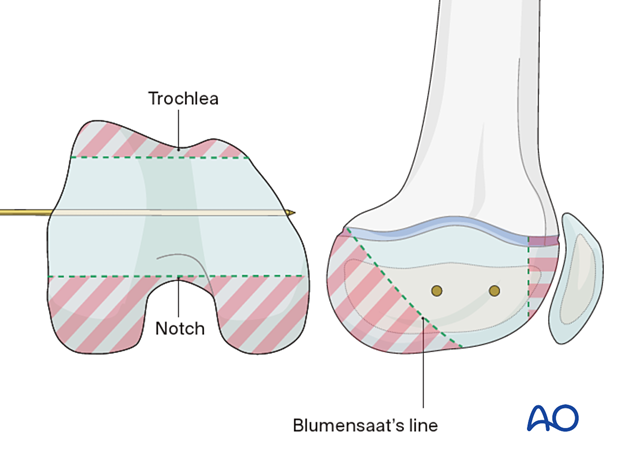
Insert a guide wire in the epiphysis parallel to and away from the growth plate.
If the K-wire for temporary fixation is in an ideal position, this can be used for screw insertion.
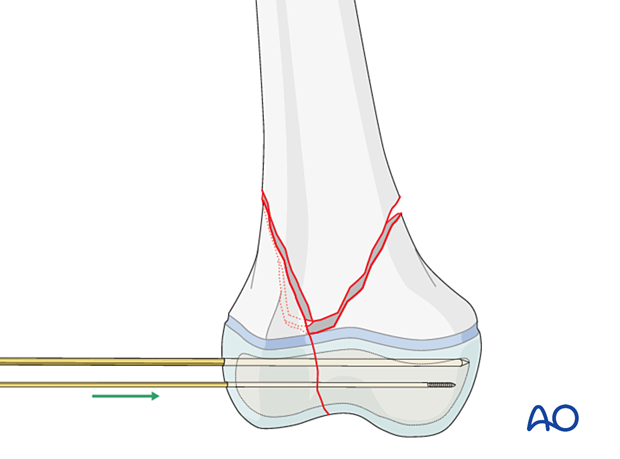
Epiphyseal screw insertion
Determine the appropriate screw length.
Choose a partially threaded screw ensuring that the thread will not cross the fracture.
Insert the screw and compress the fracture.
Confirm anatomical reduction and fixation of the articular surface with image intensification.
Remove the temporary K-wire.
4. Reduction of metaphysis
Reduction aids
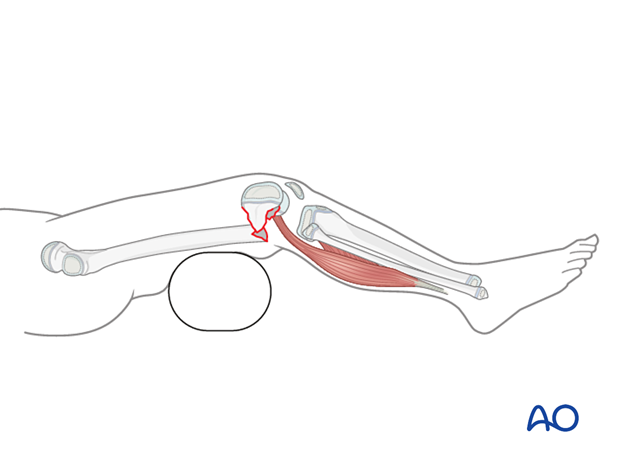
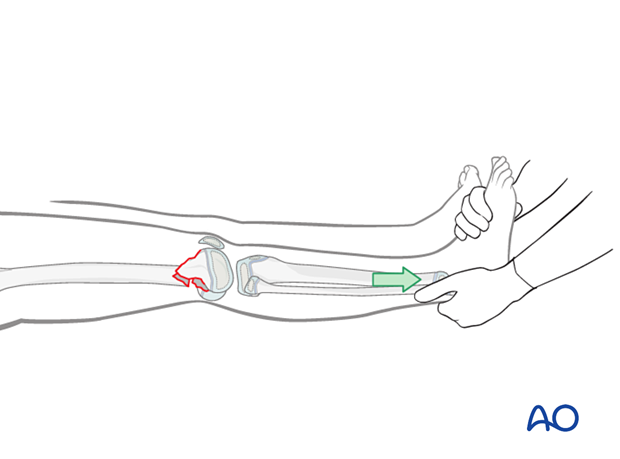
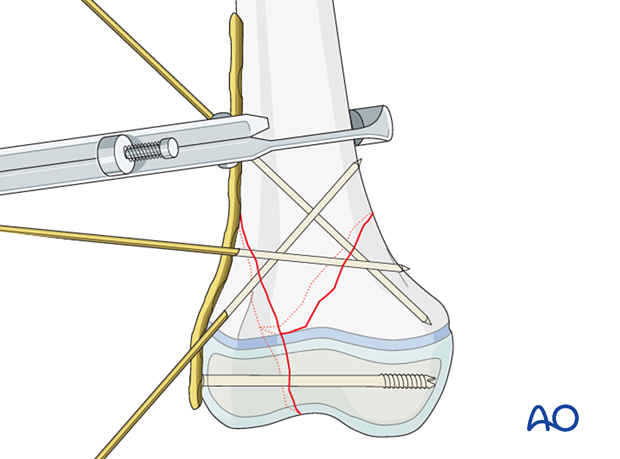
Open reduction is aided by:
- Bolsters placed posterior to the distal diaphyseal region to correct a hyperextension deformity of the distal femoral articular block
- Manual traction to restore length of the limb
- Direct pointed reduction forceps placement (particularly for spiral fractures of the metaphysis)
- A Hohmann retractor, which may be used as a lever to correct translational displacement
- K-wires, used as a joystick, to control the distal fragment
Temporary fixation with K-wires
Once the metaphyseal component of the fracture is reduced, insert multiple K-wires through the fracture for temporary fixation.
Ensure that these K-wires do not interfere with the planned plate placement.
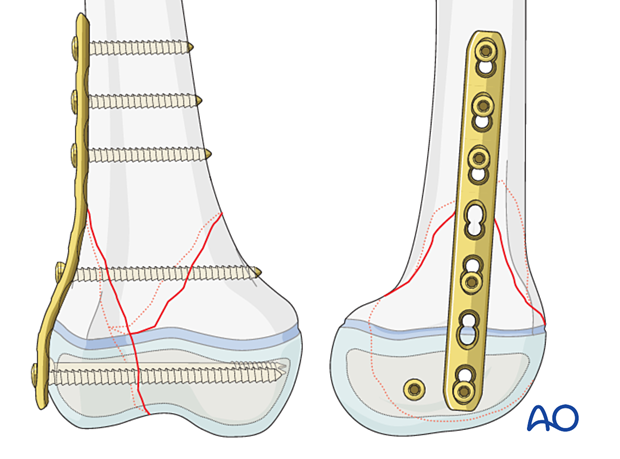
5. Plate fixation
Plate placement
Plate contouring is often required to match the anatomy of the femur.
Secure the plate with bone holding forceps.
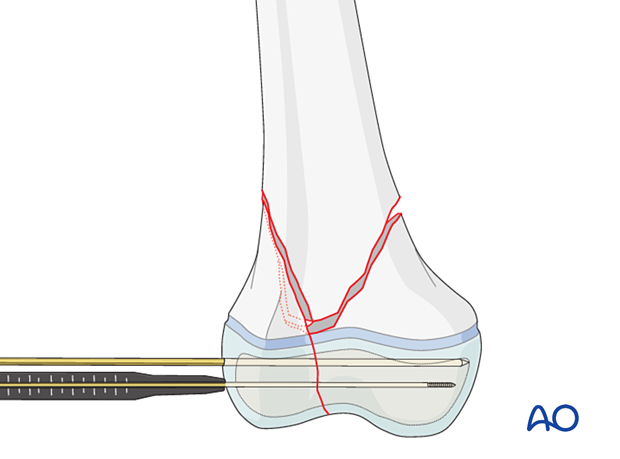
Insertion of screws
Prior to screw insertion make sure that both ends of the plate are well aligned and have good contact with the bone. Check the femoral alignment with image intensification before screw placement.
Start with insertion of a screw on both ends of the plate and then insert further screws.
Insert one or two screws through the plate distal to the growth plate.
Insert two or three screws through the plate proximal to the fracture zone.
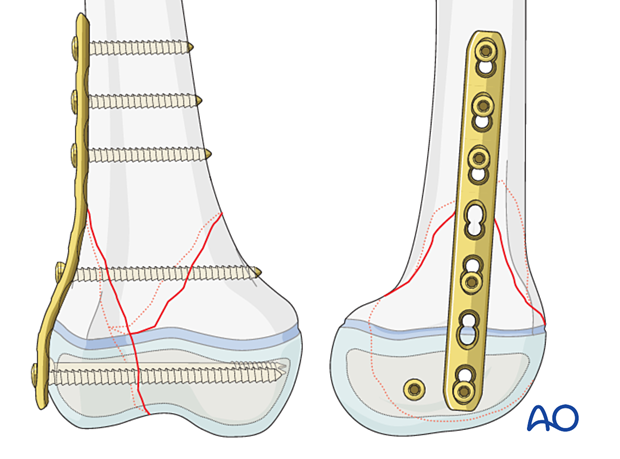
Alternative
Final construct with an adult condylar plate
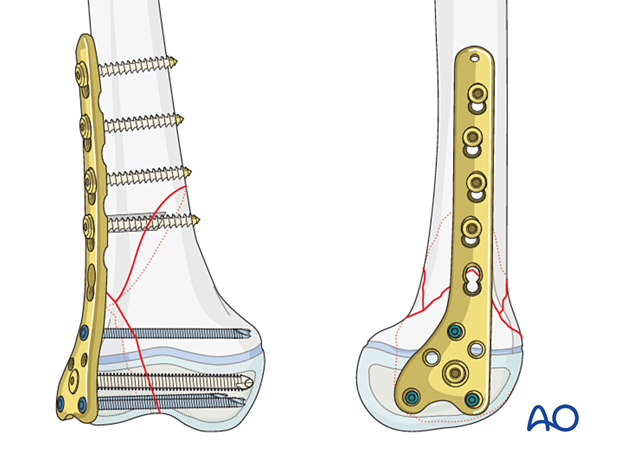
6. Final assessment
Check implant position and fracture reduction with image intensification.
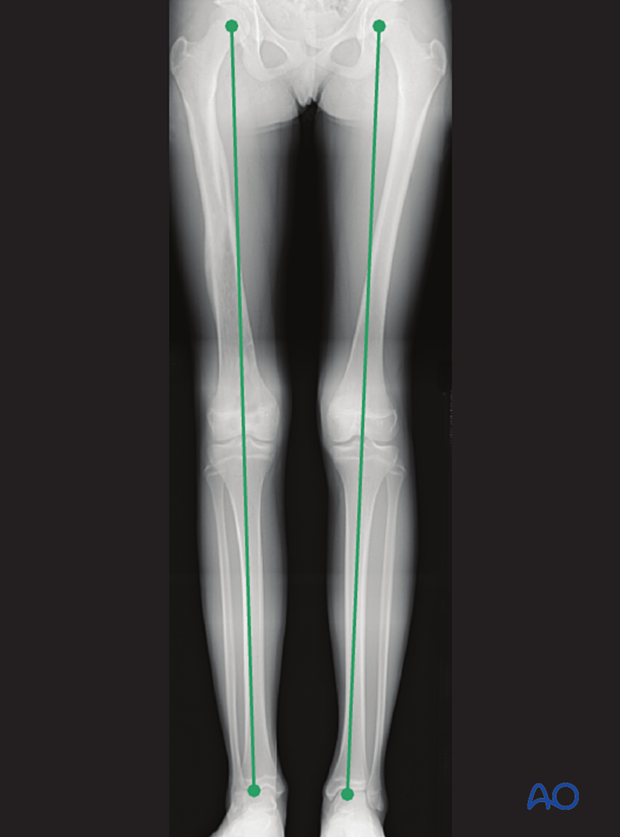
Use clinical examination to check lower extremity alignment.

7. Aftercare
Immediate postoperative care
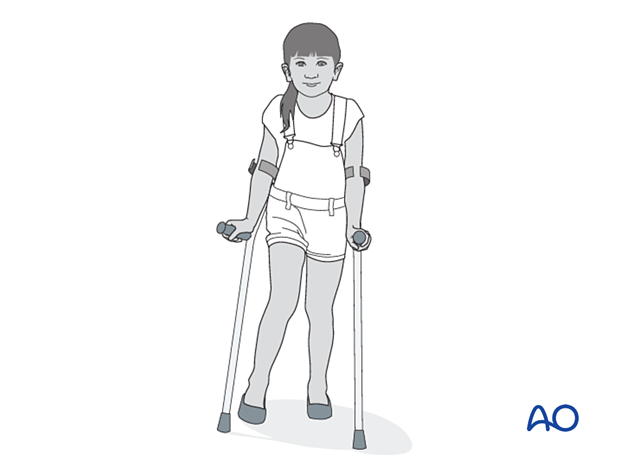
The patient should get out of bed and begin ambulation with crutches on the first postoperative day.
In most cases the postoperative protocol will be touch-weight bearing for the first 4 weeks.
Analgesia
Routine pain medication is prescribed for 3–5 days postoperatively.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise, particularly following displaced, high-energy fractures, when deterioration may be delayed.
Compartment syndrome, although rare, should be considered in the presence of severe swelling, increasing pain, and changes to neurovascular signs.
Discharge care
Discharge from hospital follows local practice and is usually possible after 1–3 days.
Mobilization
The patient should continue ambulation with crutches.
After ORIF, fractures are sufficiently stable for the knee to be immobilized in a removable brace and range-of-motion exercises can begin early in the postoperative phase.
For the more unstable or comminuted fractures, range-of-motion exercises will begin at a slower rate.
Follow-up
Clinical and radiological follow-up is usually undertaken 2 weeks postoperatively.
Follow-up for growth deformity
All patients with physeal fractures of the distal femur should have clinical and radiological examination 8–12 weeks postoperatively to assess for signs of physeal growth disturbance or resumption of growth.
Examination should be repeated at intervals until resumption of normal growth is documented. This can be seen as a horizontal growth line (Harris line) that is parallel to the entire physis on both AP and lateral views.
A growth line that converges towards the growth plate may be the earliest sign of growth arrest and should prompt investigation/treatment or referral as appropriate.
Clinical assessment of leg length and alignment is recommended at one-year.
Clinical assessment of leg length uses a tape measure from the ASIS to the medial malleolus.
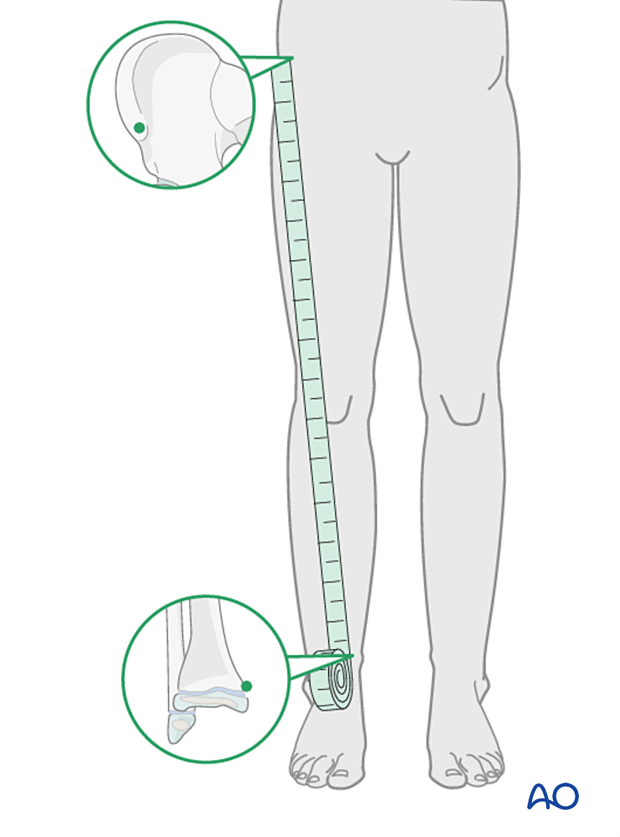
If there is any concern about leg length discrepancy or malalignment, long leg x-rays are recommended.
Leg length is measured from the femoral head to the ankle joint.
Implant removal
If symptoms develop, plate and screws can be removed once the fracture is completely healed, usually 6–12 months postoperatively.
If K-wires are used, they are typically removed after 4–6 weeks.













