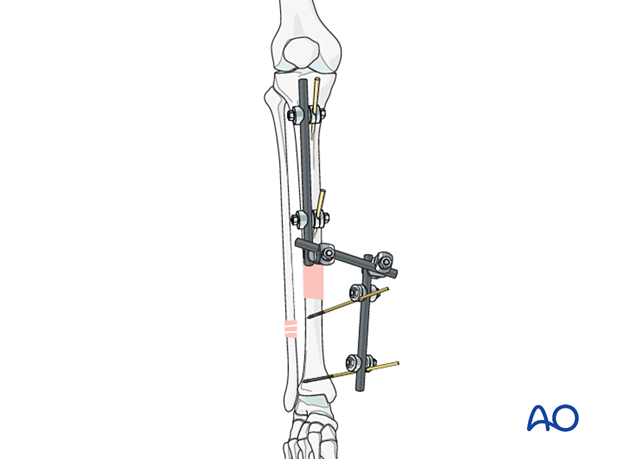
Modular external fixation
1. Principles of modular external fixation
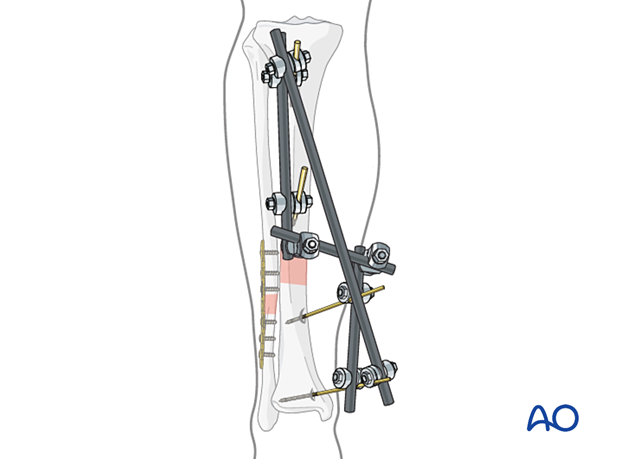
The modular external fixator is optimal for temporary use. It is rapidly applied without need for intraoperative x-rays and can be adjusted later.
Details of external fixation are described in the Modular external fixation basic technique.
Specific considerations for the tibial shaft are given below.
Teaching video
AO teaching video: Modular external fixator
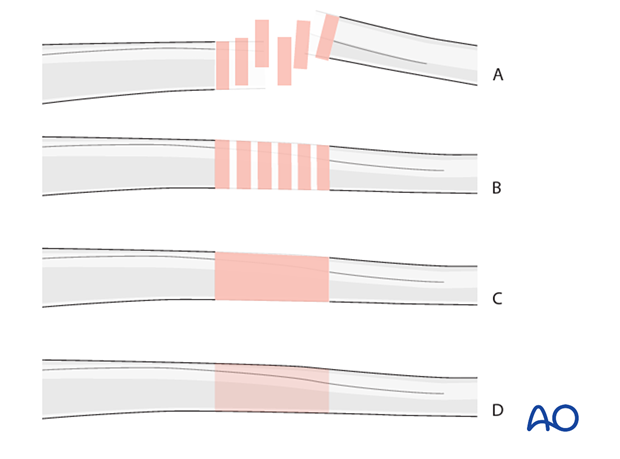
2. Note on illustrations
Throughout this treatment option illustrations of generic fracture patterns are shown as four different types:
- Unreduced fracture
- Reduced fracture
- Fracture reduced and fixed provisionally
- Fracture fixed definitively
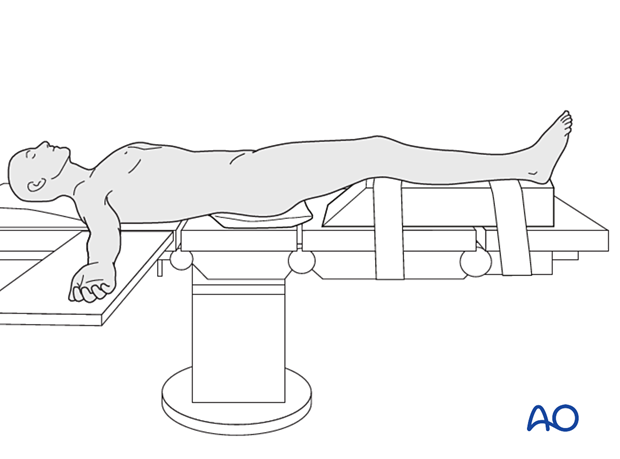
3. Patient preparation
This procedure is normally performed with the patient in a supine position.
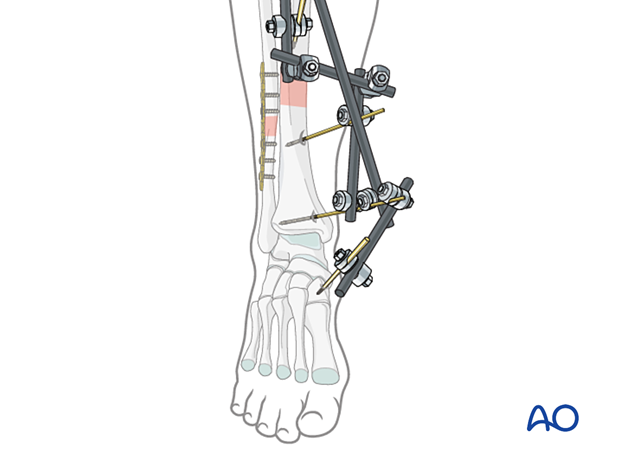
4. Safe zones for pin placement
For safe pin placement make use of the safe zones and be familiar with the anatomy of the lower leg.
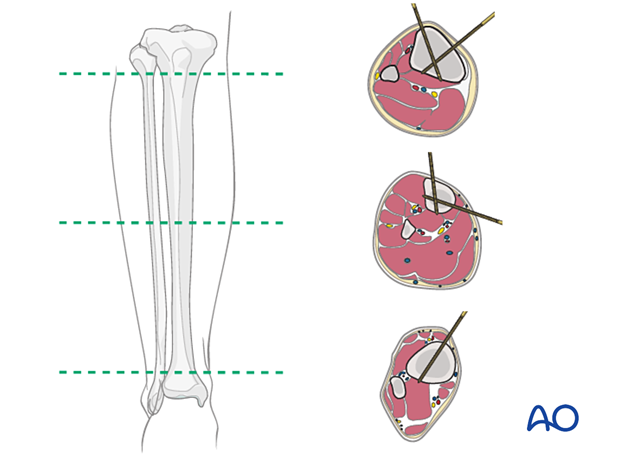
5. Pin insertion (tibial shaft)
Drilling a hole in the thick tibial crest may be associated with excessive heat generation and there is a risk the drill bit may slip medially or laterally, damaging the soft tissues. As the anteromedial tibial wall provides adequate thickness for the placement of pins, this trajectory is preferable. A trajectory angle (relative to the sagittal plane) of 20–60° for the proximal fragment and of 30–90° for the distal fragment is recommended.
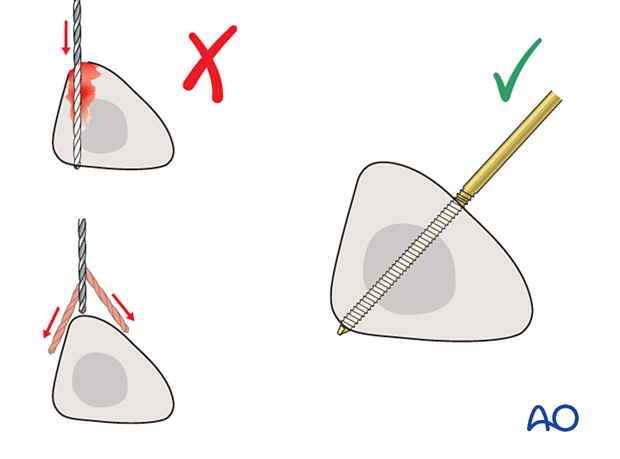
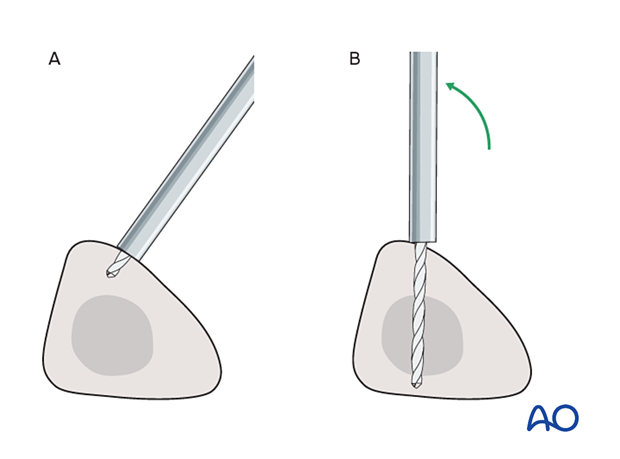
Alternatively, in order to avoid the frame catching on the opposite leg, the pins may be placed more anteriorly. The drill bit is started with the tip just medial to the anterior crest, and with the drill bit perpendicular to the anteromedial surface (A). As the drill bit starts to penetrate the surface, the drill is gradually moved more anteriorly until the drill bit is in the desired plane (B). This should prevent the tip from sliding down the medial or lateral surface.
6. Reduction and fixation
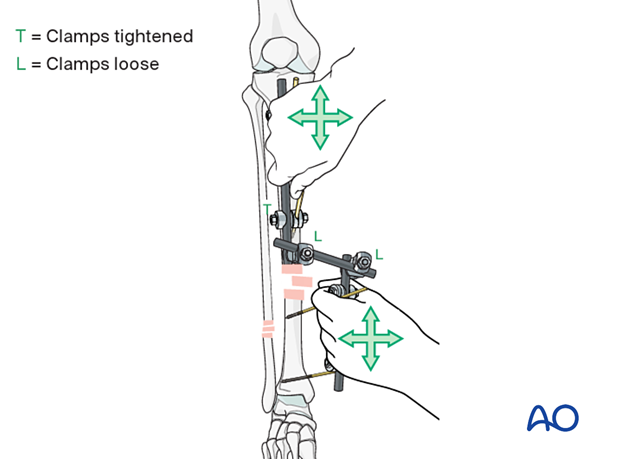
Reduction can be achieved by using the connected bars on each bone segment as handles.
7. Plating of the fibula (optional)
In order to add further stability to the reduction, a fractured fibula may be plated.
8. Aftercare
A damage-control frame is usually in place for a limited period of time prior to more definitive internal fixation. In this setting pin site care becomes less important. However, in situations in which the modular or unilateral external fixator is maintained through fracture healing refer to the following suggestions for pin site care.
Pin site care
Proper pin insertionTo prevent postoperative complications, pin insertion technique is more important than any pin care protocol:
- Correct placement of pins (see safe zones) avoiding ligaments and tendons, eg, anterior tibial tendon
- Correct insertion of pins (eg, trajectory, depth) avoiding heat necrosis
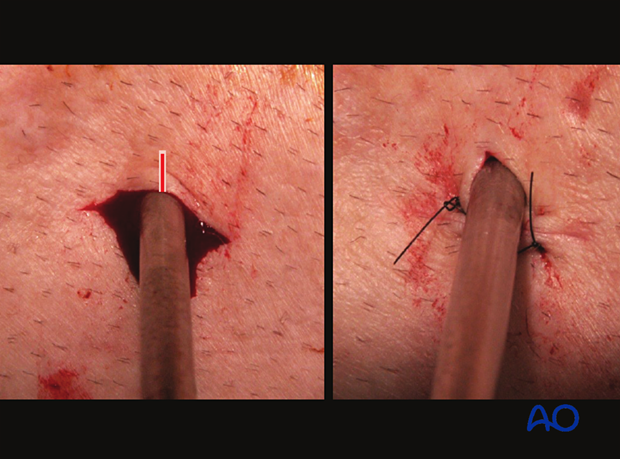
- Extending skin incisions to release soft-tissue tension around the pin insertion (see inspection and treatment of skin incisions)
- Creation of a mechanically stable frame will minimize stress and thus minimize pin-site motion
These images show the release of a pin to minimize skin tension. A releasing incision is made with a scalpel, as shown. After release, the left and right sides are sutured to create a tension-free closure.
Various aftercare protocols to prevent pin tract infection have been established by experts worldwide. Therefore, no standard protocol for pin site care can be stated here. Nevertheless, the following points are recommended:
- Relative motion between pin and skin should be minimized as a general rule. This is particularly important in areas of thick tissue or significant soft-tissue movement.
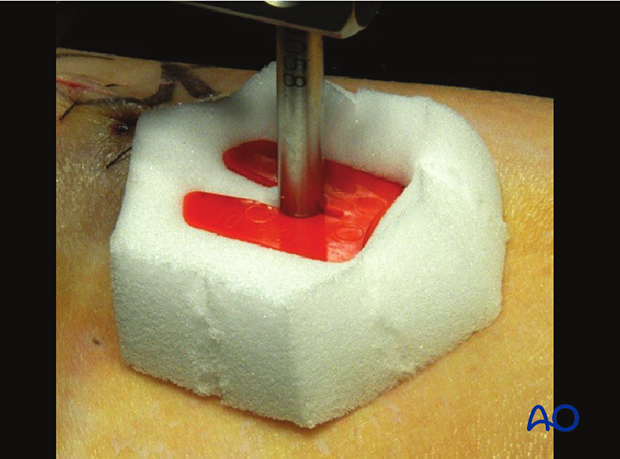
- A compressive dressing that limits skin motion is useful, initially after frame placement, and continued for any pin exhibiting ongoing drainage.
- A daily shower with antibacterial soap is very useful after surgical incisions have healed.
- Pin insertion sites should be kept clean. Any crusts or exudates should be removed. The pins may be cleaned with saline and/or disinfectant solution/alcohol. The frequency of cleaning depends on the circumstances and varies from daily to weekly but should be done in moderation.
- Dressings are not usually necessary once pin drainage has ceased.
- Pin insertion sites need not be protected for showering or bathing with clean water.
- The patient or the care-giver should learn and apply the cleaning routine.
- Oral antibiotics are reserved for pin site infections.
This image provides an example of a compressive dressing.
In case of pin/wire loosening or pin tract infection, the following steps need to be taken:
- Rest and elevate limb
- Moist saline compress
- Oral antibiotic
- Wrap pin to control skin/pin motion
- Release any skin tension
For recalcitrant pin-site problems consider:
- Culture drainage and switch to organism-specific antibiotics
- IV antibiotics
- Checking x-ray for lucency
- Removal or exchange of pin
Perioperative antibiotics may be discontinued before 24 hours.
Attention is given to:
- Pain control
- Mobilization without early weight bearing
- Leg elevation in the presence of swelling
- Thromboembolic prophylaxis
- Early recognition of complications













