ORIF - Lag screws through protection plate
1. Principles
Indications
Nonoperative treatment
Spiral fractures of the tibial diaphysis can be treated nonoperatively. However, some shortening must be expected. The initial x-ray usually shows the expected final shortening. Displacement of more than 30%, particularly for distal fractures, suggests an increased risk of secondary displacement with nonoperative treatment.
Malrotation is a risk which must be looked for and corrected, particularly during the first weeks of nonoperative treatment.
Operative treatment with a nail
Nailing is usually a good option in tibial fractures. However, in long spiral fractures, malrotation can be a problem and must be addressed by the surgeon.
Operative treatment with lag screws and protection plate
For the treatment of simple spiral fractures in the diaphyseal area, absolute stability is recommended. For this, anatomical reduction and interfragmentary compression are necessary. Interfragmentary compression is achieved with at least two lag screws, but the strength of this fixation is often insufficient for clinical use.
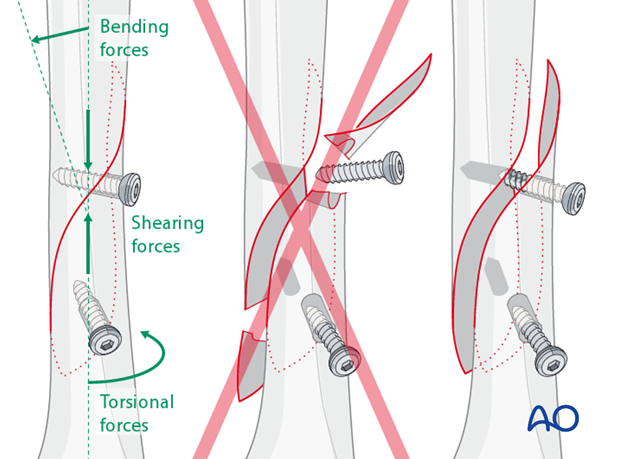
Protection plate
Bending, shearing and torsional forces acting on an unprotected lag screw may cause screw loosening, loss of compression, or fracture of the bone. In order to protect the lag screw from these forces, a protection plate should be applied.
2. Preoperative planning
Screw position
Lag screws should always be inserted as perpendicular as possible to the fracture plane where they cross it.
Lag screws inserted through a plate give better stability than screws outside of a plate. Whenever possible, plan the plate position so that one or two screws can be inserted through the plate and still perpendicular to the fracture.
However, in some situations, one, or both, lag screws have to be inserted outside of the plate, depending on fracture geometry and surgical access.
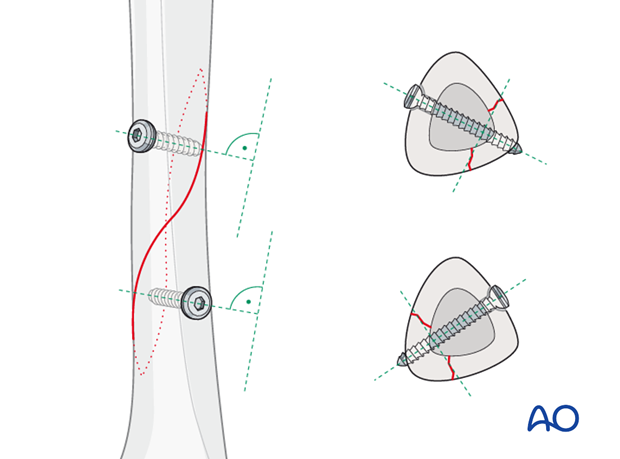
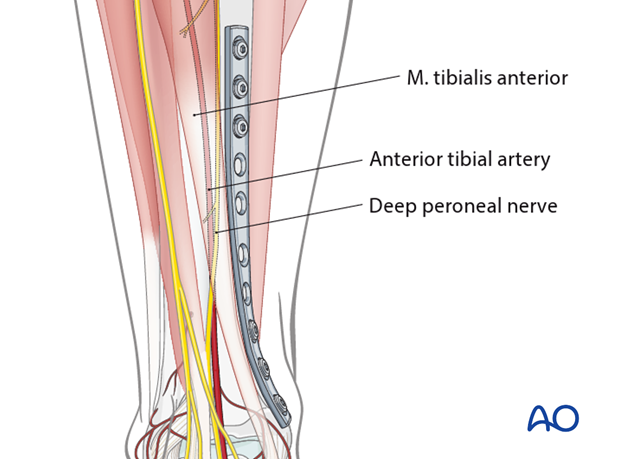
Plate location
If the anteromedial skin is completely free of injury, a plate can be positioned on this tibial surface. When in doubt about the soft tissues, an anterolateral plate may have less risk of wound breakdown.
An anteromedial, subcutaneous plate does not require muscle elevation, as would be necessary anterolaterally, but with some loss of periosteal blood supply. Furthermore, this location also allows a more distal position of the plate.
The plate should be long enough to span the fracture zone, usually with at least 3 screws proximal and distal.
A narrow, large-fragment (4.5 mm screws) plate is usually chosen. It will need to be bent and twisted to fit the selected tibial surface.
3. Patient preparation and approaches
Patient preparation
This procedure is normally performed with the patient in a supine position.
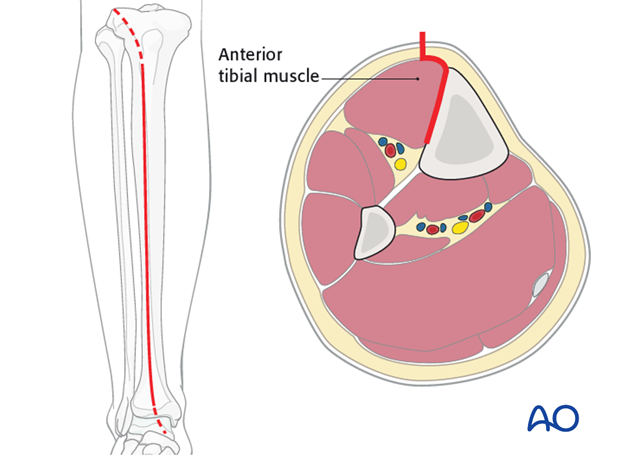
Anteromedial approach
The anteromedial approach is used most commonly for fractures of the distal third tibial shaft. However, it can be used to expose the entire anteromedial surface.
It is also useful for debridement and irrigation of open fractures when an incision on the injured subcutaneous surface is to be avoided.
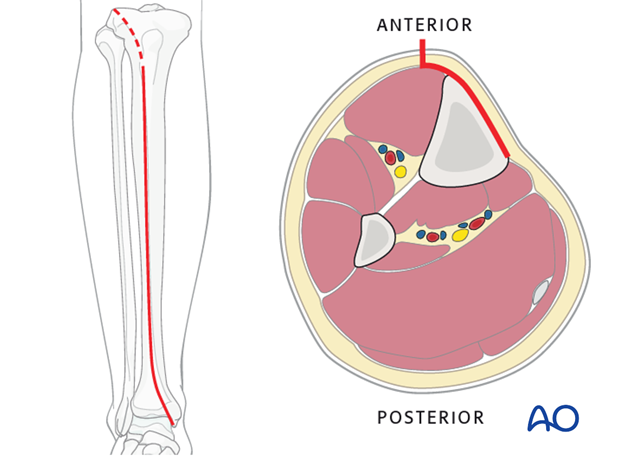
Anterolateral approach
The anterolateral approach is used uncommonly, but may be necessary when the medial soft tissues are compromised.
4. Open reduction
Introduction
Open, or direct, reduction is necessary to achieve the required anatomical reduction.
Leave the periosteum on the bone, except elevate just enough around the fracture edges to confirm the reduction.
Pointed reduction forceps are preferred because they do less damage to the soft tissues.
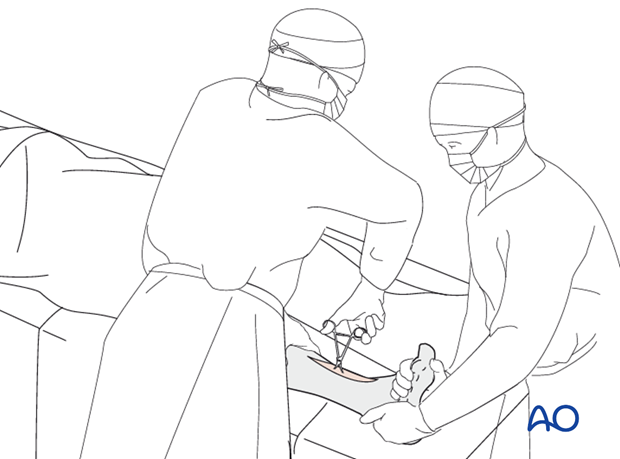
Reduction
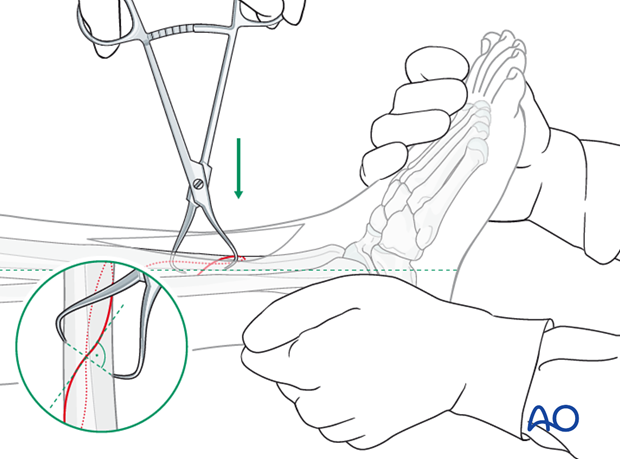
In a first step, length and rotation must be restored. This may be possible with manual traction. Otherwise, mechanical aids such as a large distractor, or bone spreader, should be considered.

In a second step, once length and rotation are restored, pointed reduction forceps are used to compress and anatomically reduce the fracture. The forceps tips should be applied perpendicular to the plane of the fracture, just like a lag screw.
5. Preparation
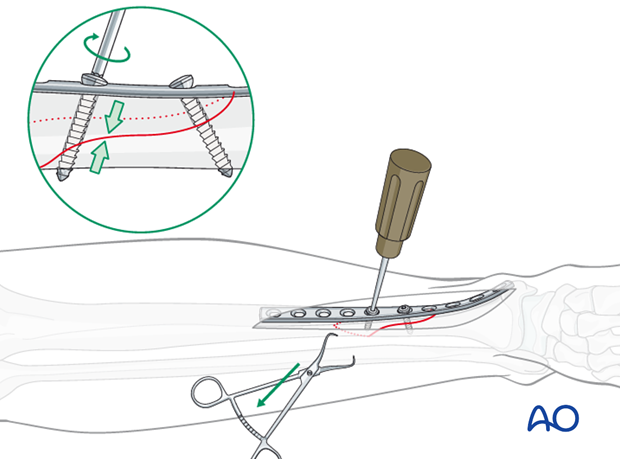
Provisional fixation with the pointed reduction forceps
Use the pointed reduction forceps to provisionally stabilize the fracture. The forceps should not interfere with plate positioning. They can be placed across the plate location as shown, or go through a screw hole.
Remember that the forceps can be positioned either medially or laterally. Choose the position that provides the most stability with the least additional soft-tissue damage.
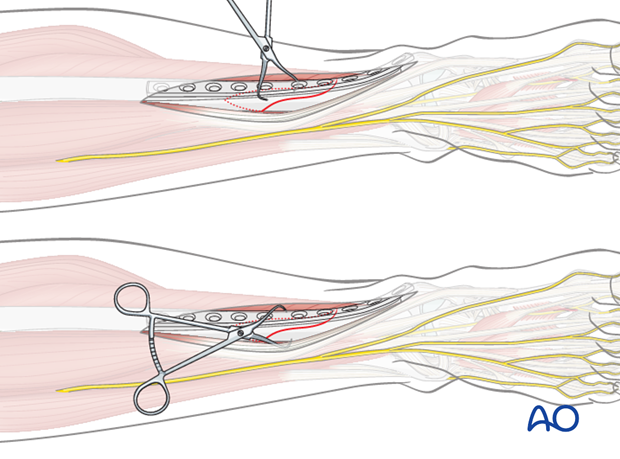
Plate selection and preparation
The chosen plate (usually a narrow, 4.5 mm DCP) should allow
1. A hole near the middle of the fracture, for the first lag screw to be inserted as perpendicularly as possible to the fracture plane.
2. Sufficient length for at least 3 screws proximal and distal to the fracture zone.
Usually a 10-12 hole straight 4.5 mm DCP is used. The plate has to be twisted and bent to fit perfectly on the surface of the tibia where it will lie.
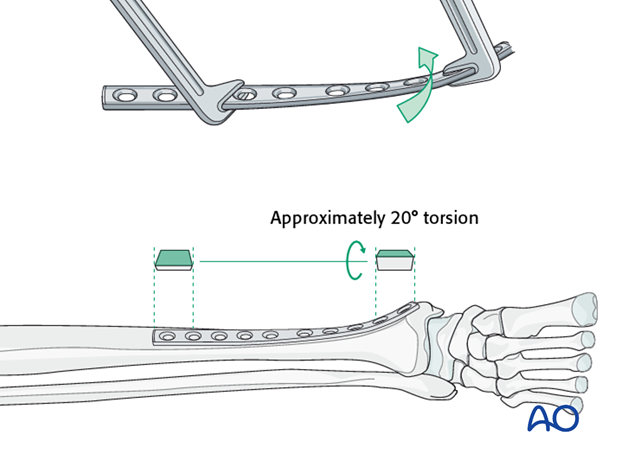
The bend of the plate is usually a 20 cm radius, and the twist is approximately 20 degrees.
6. Drilling and tapping
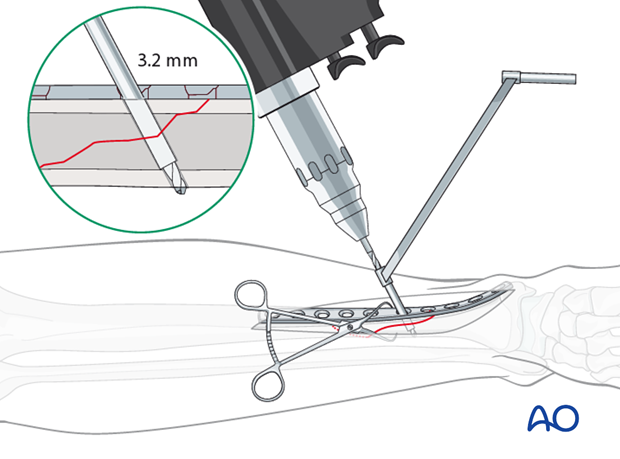
Gliding hole drilled through plate
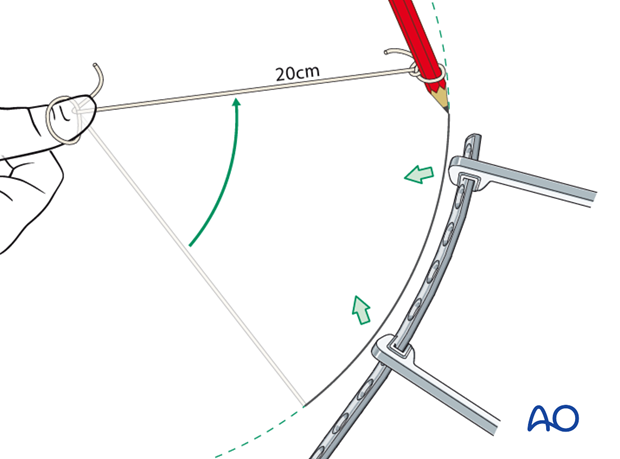
Place the contoured plate onto the bone.
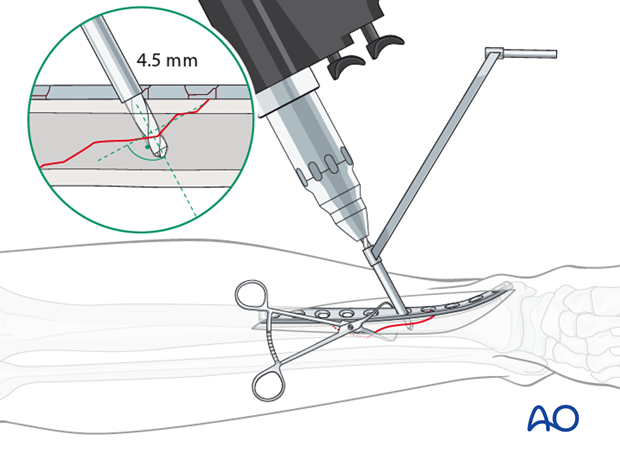
Using a 4.5 mm drill sleeve and a 4.5 mm drill bit, drill a gliding hole in the near cortex.
Ensure that the direction of the drill is as perpendicular to the fracture plane as possible, and the plate is properly positioned on the bone.
Thread hole: guide in gliding hole
Insert the 4.5 mm / 3.2 mm drill guide through the plate into the gliding hole. Use a 3.2 mm drill bit to drill a pilot hole just through the far cortex.
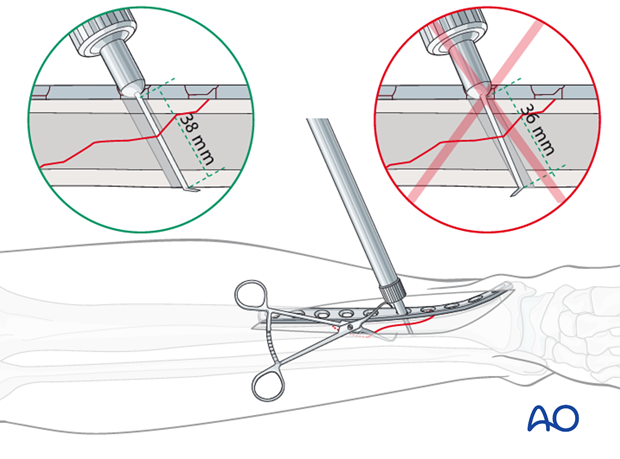
Measure for screw length
Use a depth gauge through the plate to measure for screw length.
Measure the longer side of an oblique drill hole, as shown, to ensure sufficient screw length.
A screw should protrude 1-2 mm through the opposite cortex to ensure thread purchase. However, too long a screw may be tender, or injure soft tissues.
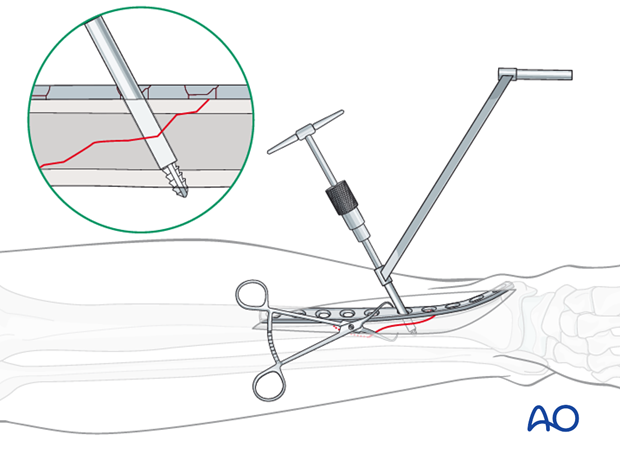
Tap the thread hole
Use a 4.5 mm cortical tap with the corresponding drill sleeve to protect adjacent soft tissues.
7. Screw insertion
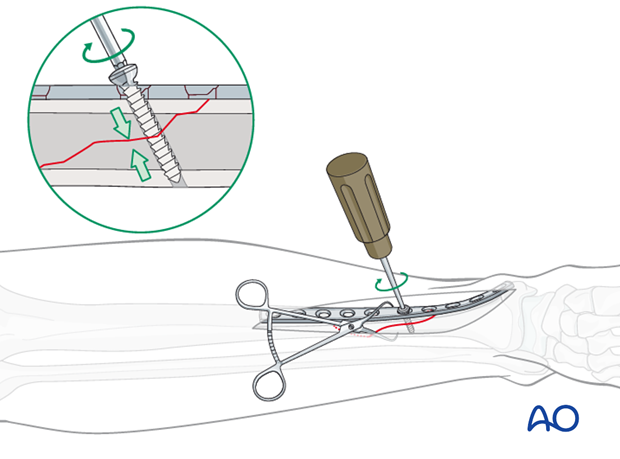
Lag screw insertion
Insert the first lag screw through the plate and carefully tighten it, making sure that the fracture stays reduced, is compressed, and the plate is approximated to the tibial surface.
Insertion of the second lag screw
Insert the second lag screw following the same steps as for the first lag screw:
- Drill the gliding hole with a 4.5 mm drill bit and drill guide. The hole should be as perpendicular to the fracture plane as possible.
- Insert the 4.5 mm / 3.2 mm drill guide into the gliding hole.
- Drill the thread hole with a 3.2 mm drill bit.
- Measure for length.
- Tap the thread hole with a 4.5 mm cortical tap.
- Insert the screw.
Due to the fracture geometry of spiral fractures, the second lag screw may not be perfectly perpendicular. However, the stability gained by inserting the screw through he plate outweighs this slight disadvantage.
8. Plate placement
Insertion of diaphyseal fixation screws
Insert the screws alternating between the proximal and distal fragments. Start with the screws closest to the fracture and work your way outwards.
Drill for the fixation screws. At least 3 screws should be used on the proximal fragment, and at least 3 screws on the distal fragment. Every hole need not be filled, but the screws closest to and furthest from the fracture are the most important.
In the diaphyseal bone, use cortical screws. Cancellous screws will be used in the metaphysis.
Observe the following steps:
- Drill both cortices using the appropriate DCP drill guide to ensure a central drill hole with the 3.2 mm drill bit.
- Measure for screw length.
- Tap both cortices using the 4.5 mm tap and appropriate drill sleeve.
- Insert the screw.
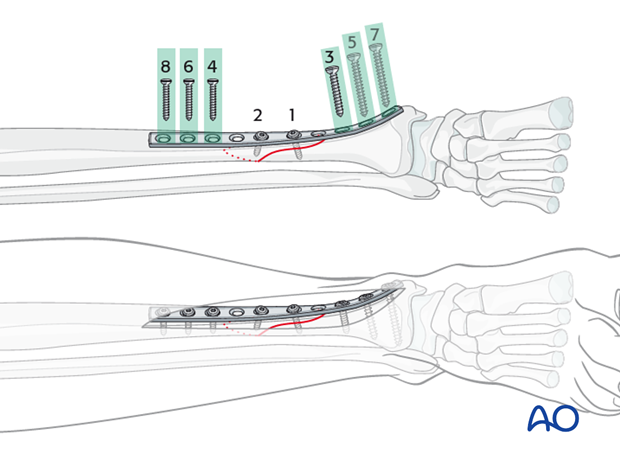
Insertion of metaphyseal plate screws
In the metaphysis, use screws with cancellous threads.
Observe the following steps:
- Drill using the appropriate DCP drill guide to ensure a central drill hole with the 3.2 mm drill bit. Do not penetrate the far cortex (or the joint).
- Measure for screw length.
- Tap just the near cortex using the 6.5 mm tap and appropriate drill sleeve.
- Insert cancellous screws and carefully tighten them.
Metaphyseal screws should be as long as possible but must not penetrate the far cortex, or the joint.
9. Postoperative care
Perioperative antibiotics may be discontinued before 24-48 hours.
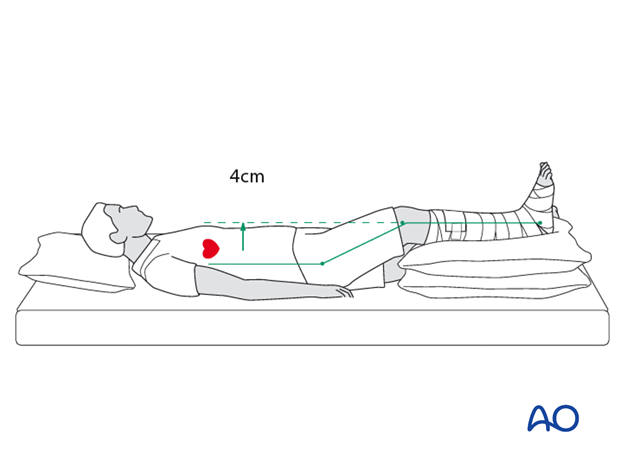
After surgery, the patient’s leg should be slightly elevated, with the leg placed on a pillow, 4 cm above the level of the heart.
Attention is given to:
- Pain control
- Mobilization without early weight bearing
- Leg elevation when not walking
- Thromboembolic prophylaxis
- Early recognition of complications
Soft-tissue protection
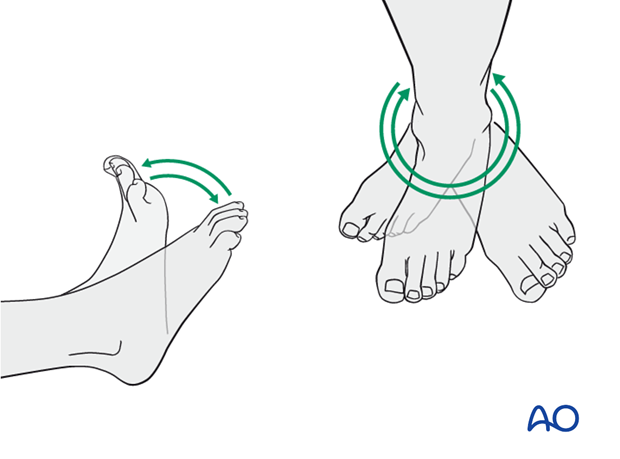
A brief period of splintage may be beneficial for protection of the soft tissues, but should last no longer than 1–2 weeks. Thereafter, mobilization of the ankle and subtalar joints should be encouraged.
Mobilization
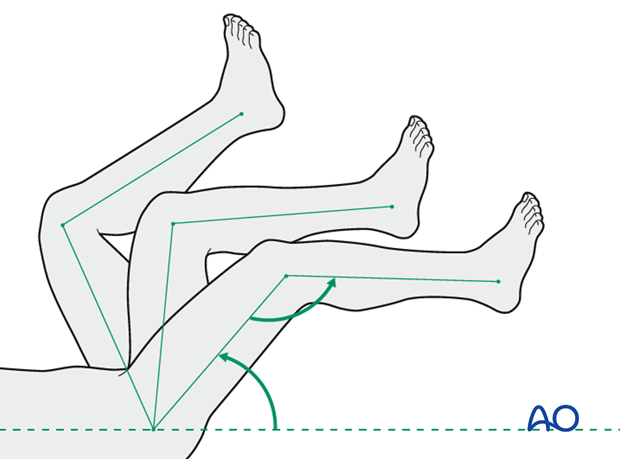
Active and assisted motion of all joints (hip, knee, ankle, toes) may begin as soon as the patient is comfortable. Attempt to preserve passive dorsiflexion range of motion.
Weight bearing
Limited weight-bearing (15 kg maximum), with crutches, may begin as tolerated, but full weight bearing should be avoided until fracture healing is more advanced (10-12 weeks).
Follow up
Follow-up is recommended after 2, 6 and 12 weeks, and every 6-12 weeks thereafter until radiographic healing and function are established. Depending on the consolidation, weight bearing can be increased after 6-8 weeks with full weight bearing when the fracture has healed by x-ray.
Implant removal
Implant removal may be necessary in cases of soft-tissue irritation by the implants. The best time for implant removal is after complete bone remodeling, usually at least 24 months after surgery. This is to reduce the risk of refracture.













