ORIF - Lag screws outside protection plate
1. Principles
Indications
Nonoperative treatment
Oblique fractures of the tibial diaphysis can be treated nonoperatively if the initial displacement is small and there is <1 cm shortening.
Operative treatment with a nail
Nailing is usually a good option for tibial fractures, but is technically more difficult for proximal and distal locations.
Operative treatment with plate and screws
For the treatment of simple oblique fractures in the diaphyseal area, absolute stability is recommended.
For this, anatomical reduction and interfragmentary compression are necessary.
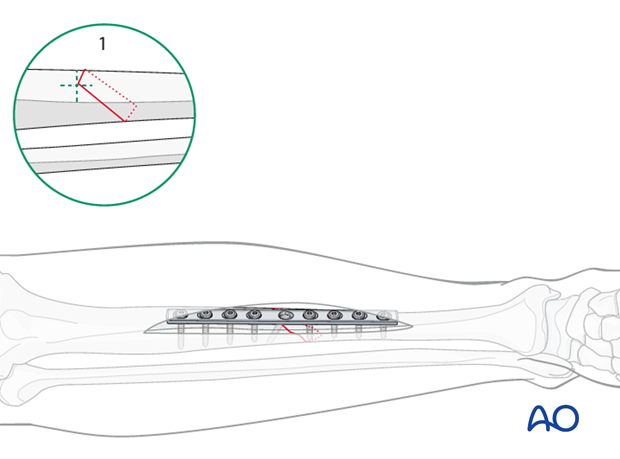
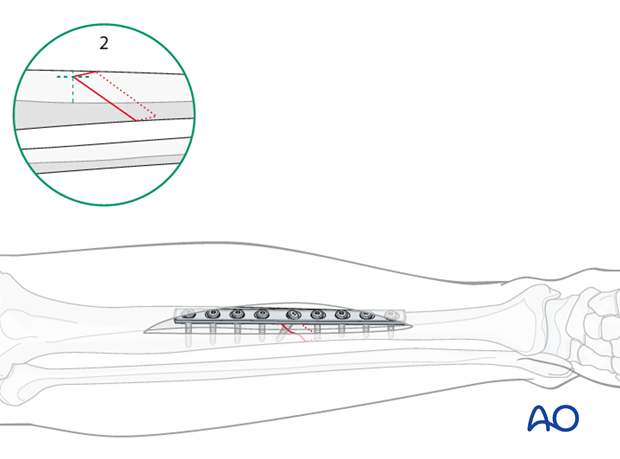
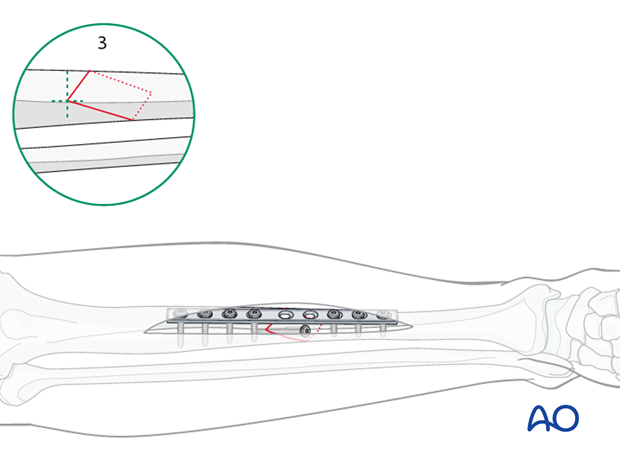
Choosing the method of interfragmentary compression
The method of interfragmentary compression is determined by the fracture geometry and the plane of the obliquity.
1. The tip of the fracture is in the center of the anteromedial or anterolateral surface of the tibia
In this case, the fracture can be compressed with an axial compression plate, with a supplementary lag screw through the plate.
The apex of the fracture should be underneath the plate.
2. The tip of the fracture is not in the center of the anteromedial or anterolateral surface, but either posterior or anterior
In this case, compression must be done with a lag screw, usually inserted through the plate. In this case, the plate is used in protection rather than compression mode. The apex of the fracture is not underneath the plate, but either anterior or posterior of it.
3. The tip of the fracture lies on the tibial crest
In this case, a lag screw outside of the plate (protection mode) is usually required.
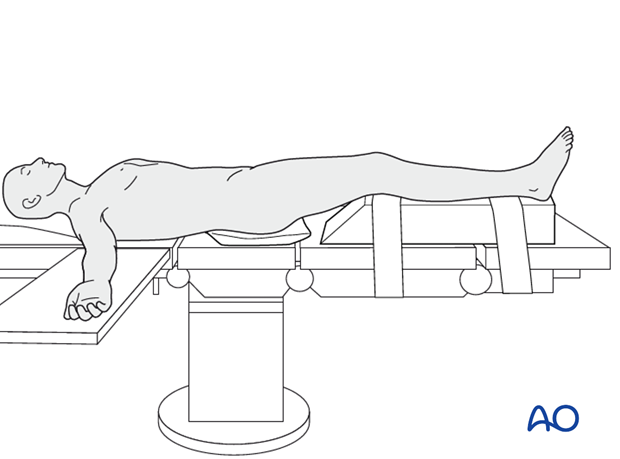
2. Patient preparation and approaches
Patient preparation
This procedure is normally performed with the patient in a supine position.
Anteromedial approach
The anteromedial approach is used most commonly for fractures of the distal third tibial shaft. However, it can be used to expose the entire anteromedial surface.
It is also useful for debridement and irrigation of open fractures when an incision on the injured subcutaneous surface is to be avoided.
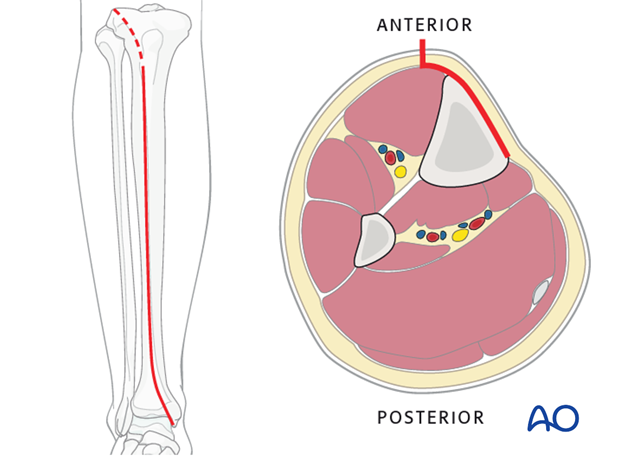
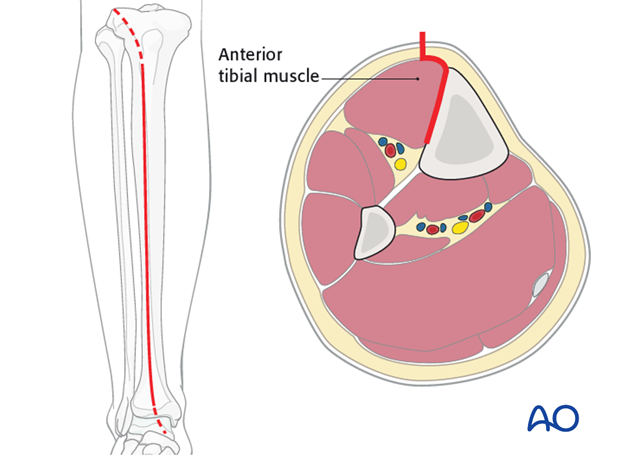
Anterolateral approach
The anterolateral approach is used uncommonly, but may be necessary when the medial soft tissues are compromised.
3. Open reduction
Introduction
As anatomical reduction is necessary, open, or direct, reduction is needed.
Mobilize just enough of the periosteum around the fracture edges to control the reduction. Take care to protect the periosteum wherever possible.
Because they do less damage to the soft tissues, pointed reduction forceps are best used.
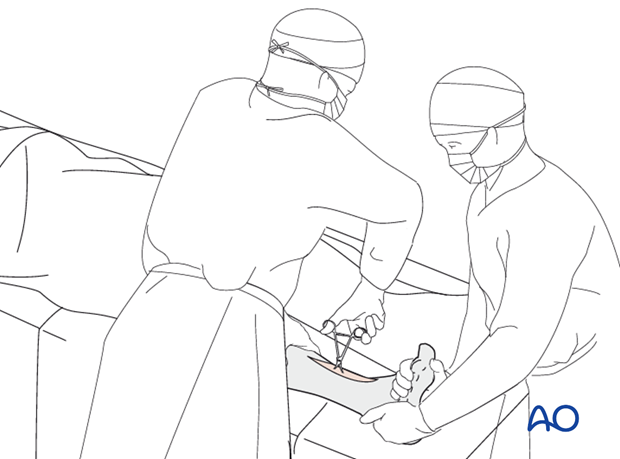
Manual traction
In a first step, length and rotation must be restored. This may be possible with manual traction. Otherwise, mechanical aids such as a large distractor, or bone spreader, should be considered.

Reduction of the fracture
In a second step, once length and rotation are restored, pointed reduction forceps are used to compress and anatomically reduce the fracture. The forceps tips should be applied perpendicular to the plane of the fracture, just like a lag screw. Place the forceps outside the intended path of the lag screw.
Provisional fixation with the pointed reduction forceps
Use the pointed reduction forceps to provisionally stabilize the fracture. Select a position for the forceps so that it will not interfere with the planned position of the screw and the plate.
Also, consider that the forceps can be positioned either medially or laterally. Choose the position that allows the most stability with the least soft-tissue damage.

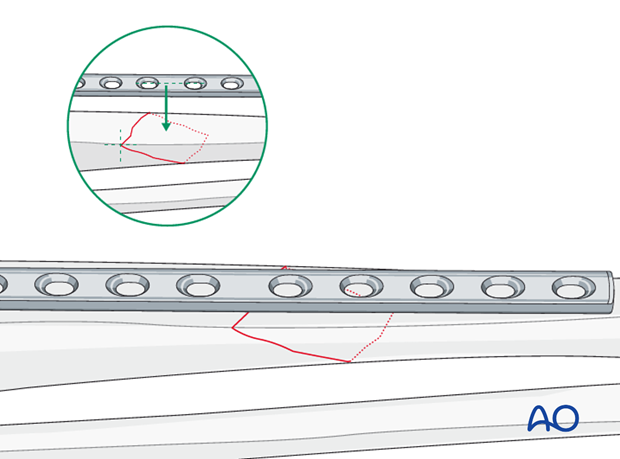
4. Confirm fracture plane
Confirm that the fracture apex lies on the tibial crest. This indicates that the lag screw must lie outside the plate.
If the fracture apex is on the anteromedial or anterolateral surface and the plate can be applied over it, an axial compression plate with a lag screw should be applied instead.
On the other hand, if the plate can not be applied over the fracture apex, a lag screw through a protection plate should be employed.
5. Lag screw insertion
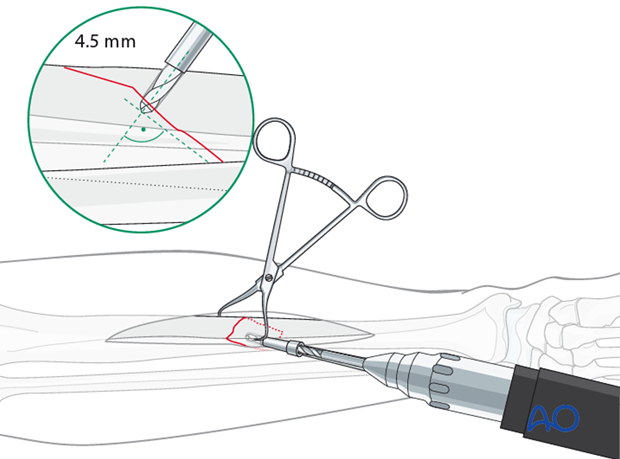
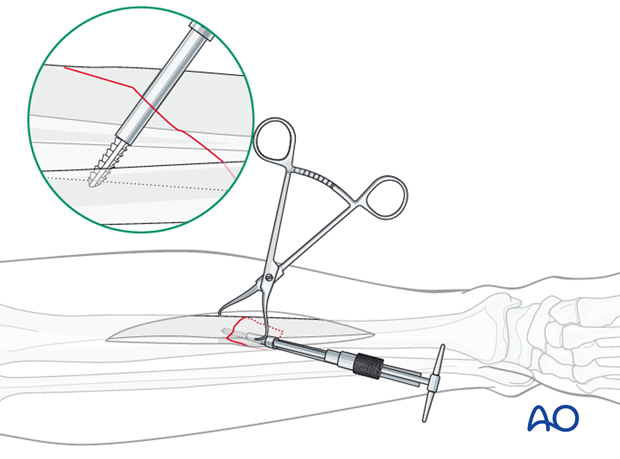
Drilling the gliding hole for the lag screw
Using a 4.5 mm drill guide and a 4.5 mm drill bit, drill a gliding hole in the near cortex. This screw must not interfere with planned plate placement.
Ensure that the direction of the drill is as perpendicular to the fracture plane as possible.
Drilling the thread hole
Insert the 4.5 mm / 3.2 mm drill guide through the plate and the gliding hole. Use a 3.2 mm drill bit to drill a thread hole just through the far cortex.

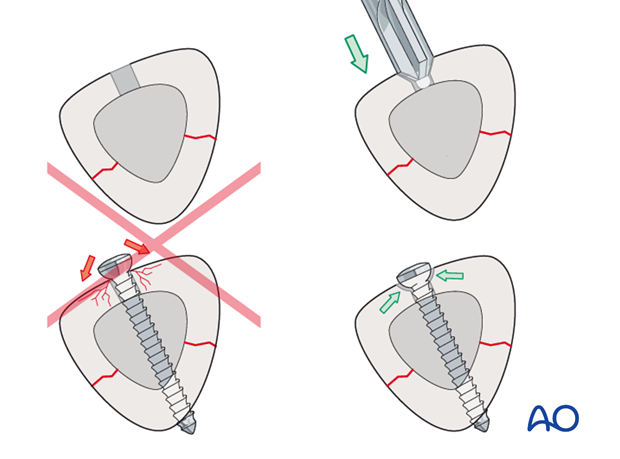
Countersinking in diaphyseal bone
There are two important reasons for countersinking:
1. Countersinking ensures that the screw head has a maximal contact area with the bone, so that its compressive forces are widely distributed.
2. A countersunk screw head is less prominent and tender.
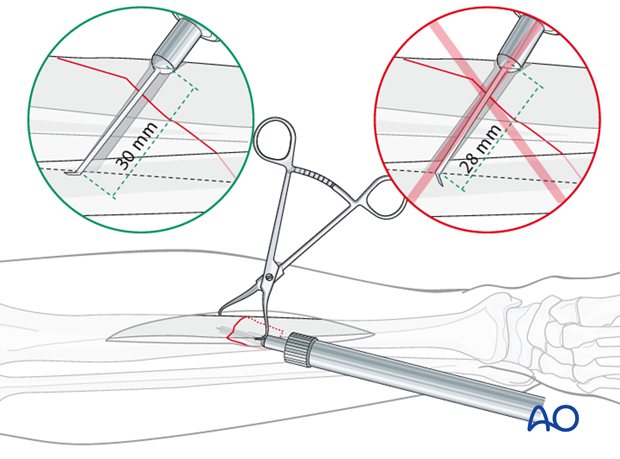
Measure for screw length
Use a depth gauge to measure for screw length.
Measure the longer side of an oblique drill hole, as shown, to ensure sufficient screw length.
A screw should protrude 1-2 mm through the opposite cortex to ensure thread purchase. However, too long a screw may be tender, or injure soft tissues.
Tap the thread hole
Use a 4.5 mm tap and the corresponding drill sleeve to tap the thread hole.
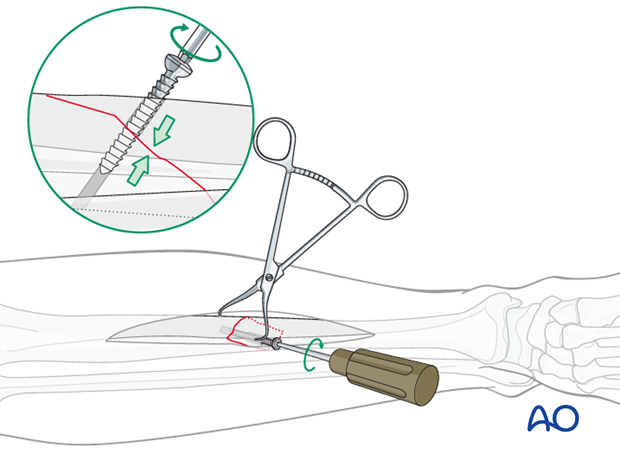
Insertion of the lag screw
Insert the lag screw and carefully tighten it. Confirm that the fracture is reduced anatomically and compressed.
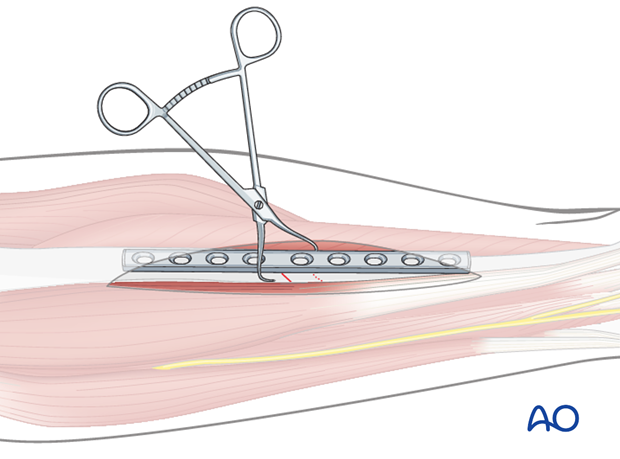
6. Plate fixation
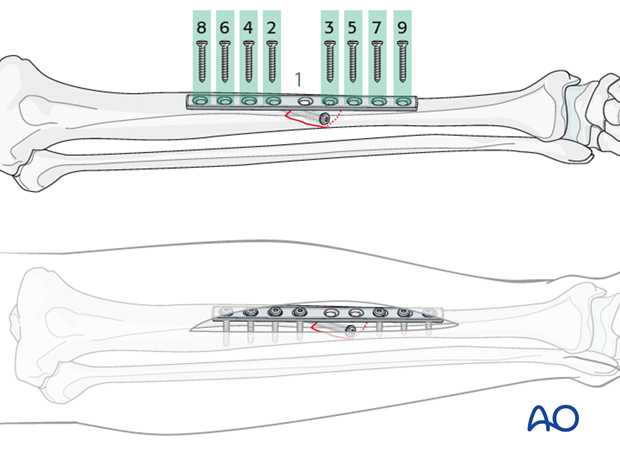
Plate selection and preparation
The chosen plate (usually a narrow, 4.5 mm DCP) should allow
1. A hole near the middle of the fracture, for the first lag screw to be inserted as perpendicularly as possible to the fracture plane.
2. Sufficient length for at least 4 screws proximal and distal to the fracture zone.
Usually a 8-9 hole straight 4.5 mm DCP is used.
Remember that whenever the plate is placed distally, the plate must be twisted and bent to match the shape of the tibia in that region.
Insertion of screws
Insert the screws alternating between the proximal and distal fragments. Start with the screws closest to the fracture plane and work your way outwards.
Drill for the fixation screws. At least 4 screws should be used on the proximal fragment, and at least 4 screws on the distal fragment.
Use cortical screws for the diaphysis, observing the following steps:
- Drill both cortices using the appropriate drill guide to ensure a central drill hole with the 3.2 mm drill bit.
- Measure for screw length.
- Tap both cortices using the 4.5 mm tap and appropriate drill sleeve.
- Insert the screw.
7. Postoperative care
Perioperative antibiotics may be discontinued before 24-48 hours.
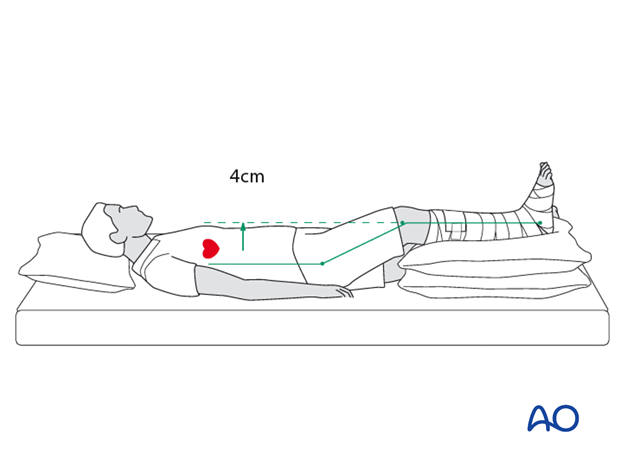
After surgery, the patient’s leg should be slightly elevated, with the leg placed on a pillow, 4 cm above the level of the heart.
Attention is given to:
- Pain control
- Mobilization without early weight bearing
- Leg elevation when not walking
- Thromboembolic prophylaxis
- Early recognition of complications
Soft-tissue protection
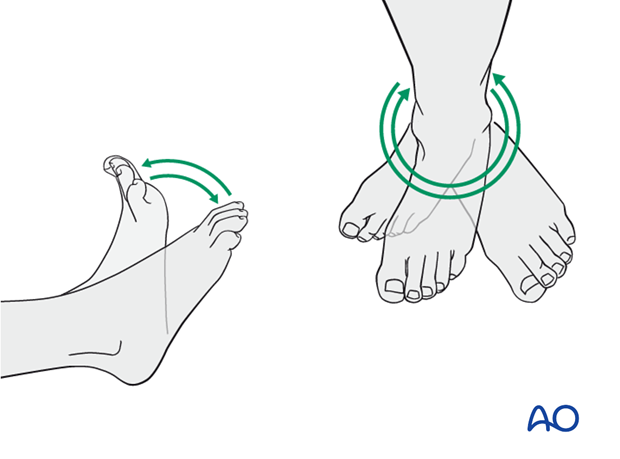
A brief period of splintage may be beneficial for protection of the soft tissues, but should last no longer than 1–2 weeks. Thereafter, mobilization of the ankle and subtalar joints should be encouraged.
Mobilization
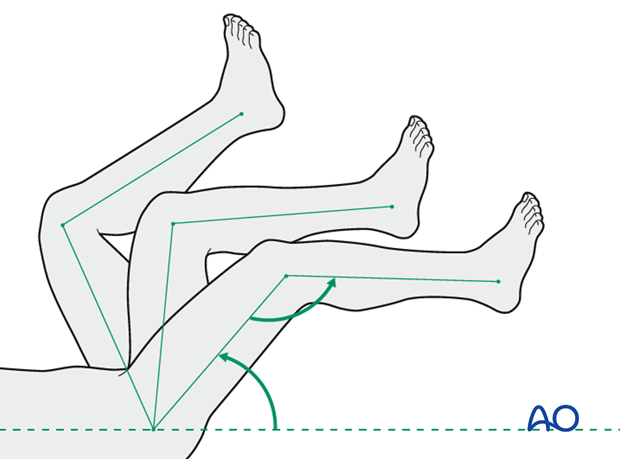
Active and assisted motion of all joints (hip, knee, ankle, toes) may begin as soon as the patient is comfortable. Attempt to preserve passive dorsiflexion range of motion.
Weight bearing
Limited weight-bearing (15 kg maximum), with crutches, may begin as tolerated, but full weight bearing should be avoided until fracture healing is more advanced (10-12 weeks).
Follow up
Follow-up is recommended after 2, 6 and 12 weeks, and every 6-12 weeks thereafter until radiographic healing and function are established. Depending on the consolidation, weight bearing can be increased after 6-8 weeks with full weight bearing when the fracture has healed by x-ray.
Implant removal
Implant removal may be necessary in cases of soft-tissue irritation by the implants. The best time for implant removal is after complete bone remodeling, usually at least 24 months after surgery. This is to reduce the risk of refracture.
8. Case
This is a simple spiral fracture of the tibial shaft with a proximal fibular neck fracture.
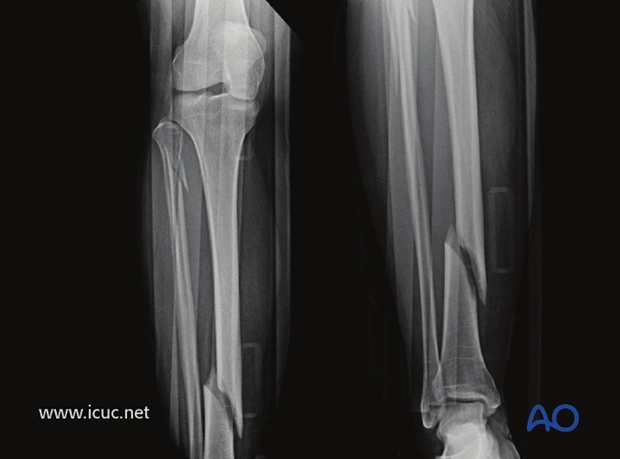
Lateral image of the same fracture.
Because of the spiral nature of this fracture, many of these twisting injuries have a component of fracture that goes into the joint. A CT scan was used to assess this.
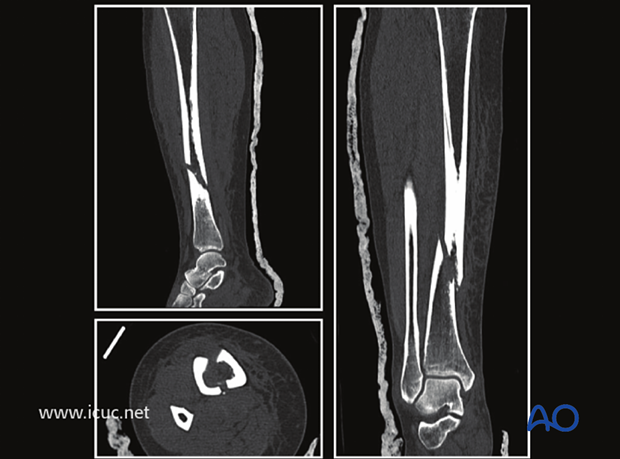
A CT scan at the malleolar level showed that the fracture did continue into the ankle joint but with minimal displacement.
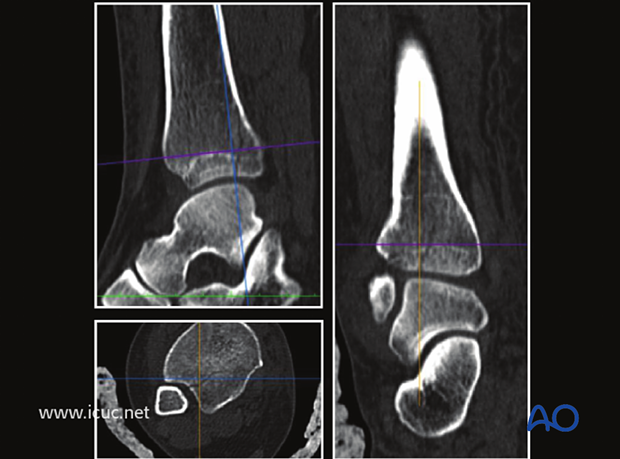
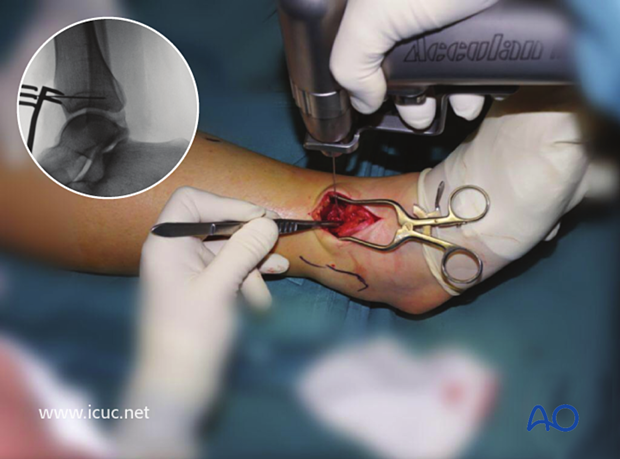
Before plating the tibia, a lag screw was placed across the fracture site just above the ankle to prevent the intraarticular component from displacing.

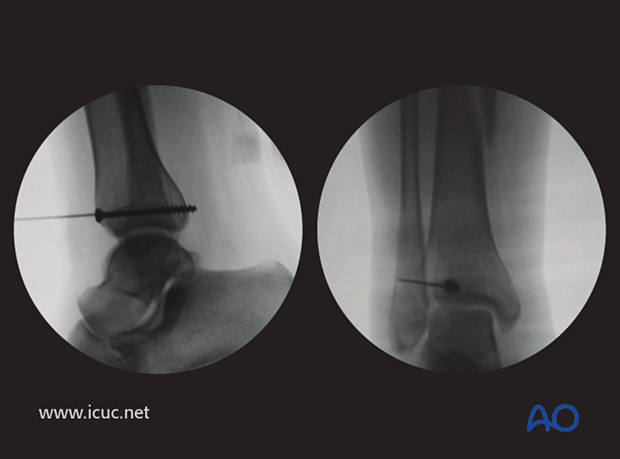
A K-wire was inserted to ensure the fracture did not displace during lag screw insertion.
The lag screw was placed just above the joint line in the AP plane. This lag screw is probably 2 mm too long.
The fracture was reduced with the help of a distractor with pins in the calcaneus and proximal tibia. Note the small incision directly anterior, perpendicular to the fracture plane so that the fracture can be reduced under direct vision.

The fracture has been exposed but not yet reduced.
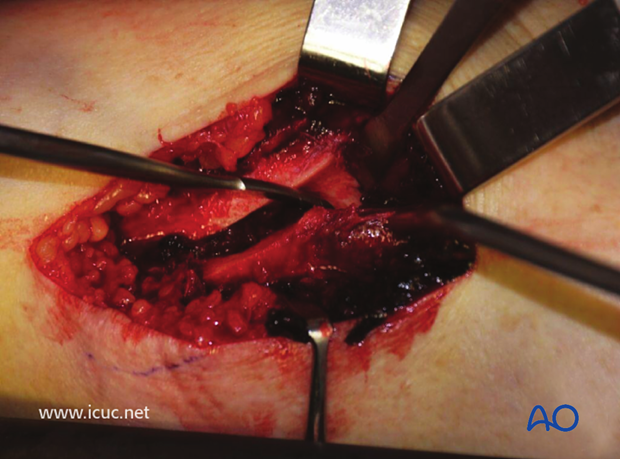
The fracture has now been reduced and held with a sharp Weber clamp.

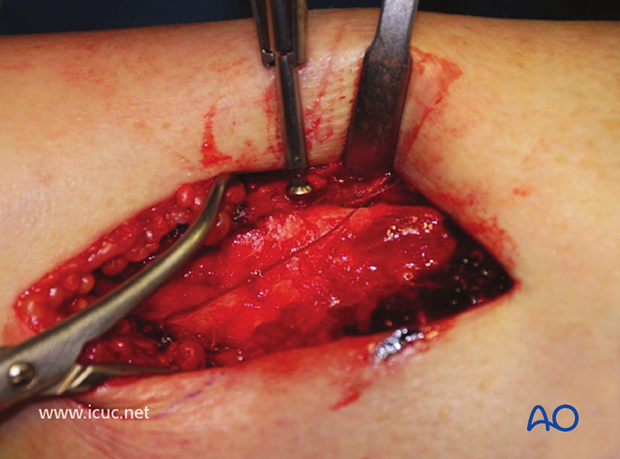
The pilot hole for a cortical lag screw is being drilled from anterior to posterior.

After tapping and countersinking, the cortical lag screw is inserted. Care must be taken not to overtighten it as this might create a new fracture.
The distal incision for the MIPO plate insertion is made on the medial side, taking care not to damage the saphenous vein and nerve.

The appropriate length LCP is selected and contoured.
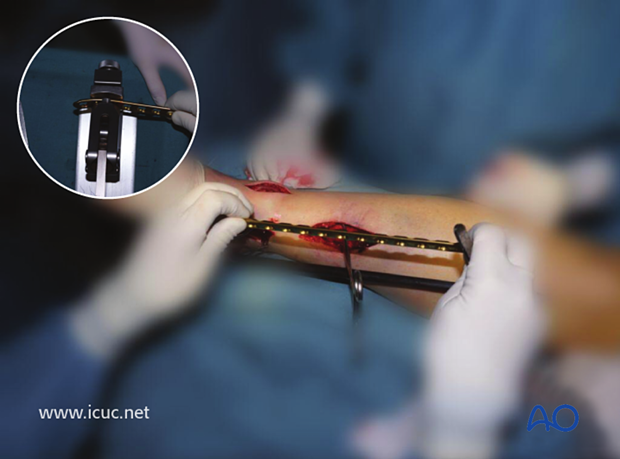
A small amount of distal contour allows for the medial malleolar flare.

The proximal incision is made.

The plate is slid under the soft tissues along the surface of the bone. In this case the plate required further contouring so it was removed, adjusted and reinserted.

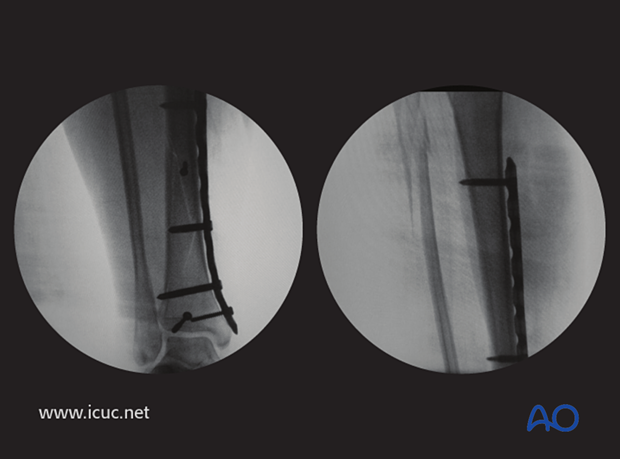
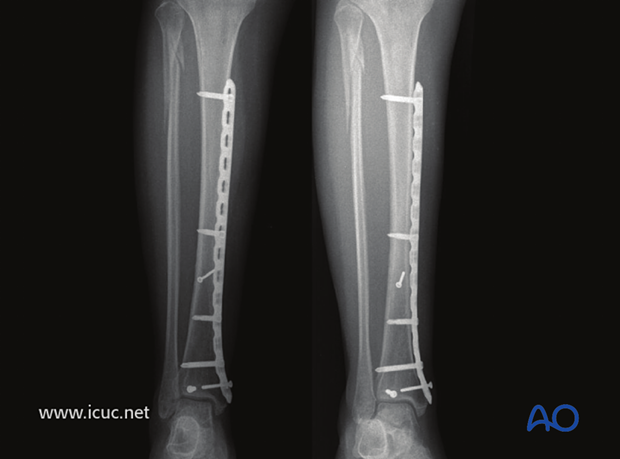
Final AP X-rays of MIO plating using the near far principle for screw placement. It is important to remember that any screw that crosses a fracture line should be used with lag technique.
As the fracture was well reduced, and held with two lag screws, the surgeon felt that only two distal screws and two proximal screws were required to achieve sufficient stability.
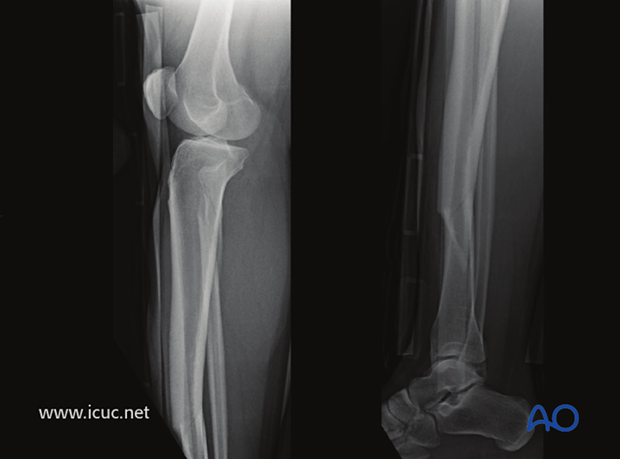
AP lateral X-rays at 6 weeks, showing the reduction has been maintained and the fracture is healing.

Healed tibial fracture at 6 months.
Clinical image of good outcome at 30 weeks.














