Principles of management of open fractures
1. Classification of open fractures
Introduction
In 1895, Stanley Boyd said, “The most important divisions of fractures - simple, compound and complicated - are based upon the condition of the soft parts.”
There is no doubt that the status of soft-tissue wounding in open fractures is a crucial determinant of patient outcomes.
Most research shows that infection rates increase with the severity of soft-tissue injuries. Bony injury is less important, provided that the injured bone retains a blood supply.
Common classifications
Soft-tissue wounds associated with fractures are classified according to two systems, namely that of Gustilo, Mendoza, and Williams and also that of the AO.
An additional influence is the ability of the host to combat infection, based on both systemic and local factors. For details see the Cierny classification.

Wound-severity classification
The Gustilo–Anderson classification divides open fractures into three grades – I, II, and III.
This work largely addresses lower leg injuries but has some value in other anatomical sites.
Gustilo RB, Anderson JT Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses J Bone Joint Surg Am. 1976 Jun;58(4):453-8.
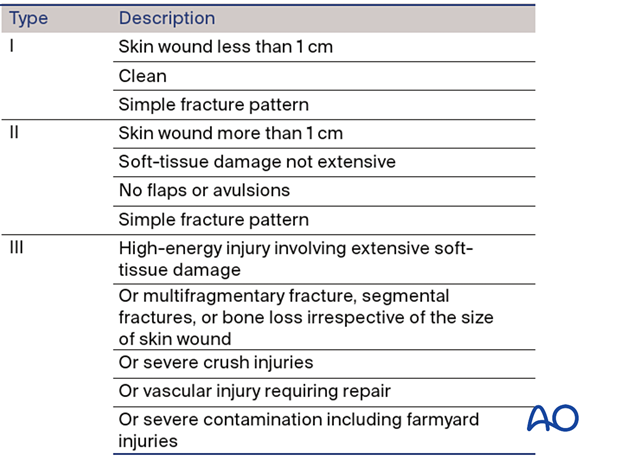
This illustration summarizes the three basic grades – I, II, and III.
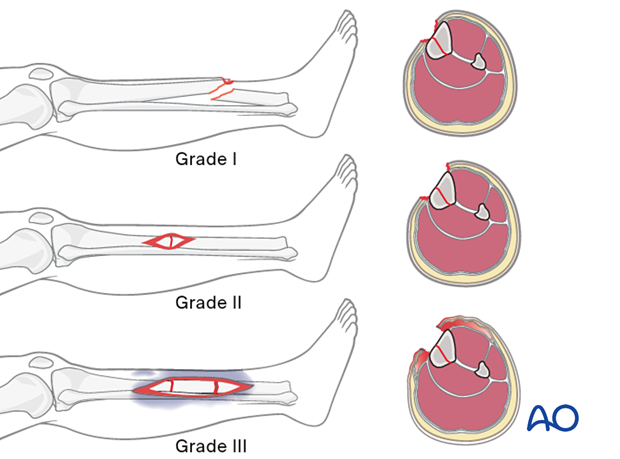
Grade III was later further subdivided into types IIIA, IIIB, and IIIC by Gustilo, Mendoza and Williams.
Gustilo RB, Mendoza RM, Williams DN Problems in the management of type III (severe) open fractures. A new classification of type III open fractures. J. Trauma 1984 Aug;24(8):742–6.
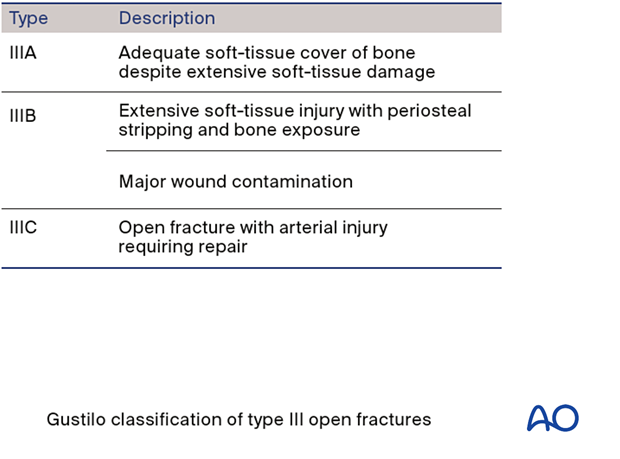
These examples illustrate the three types – IIIA, IIIB, and IIIC.

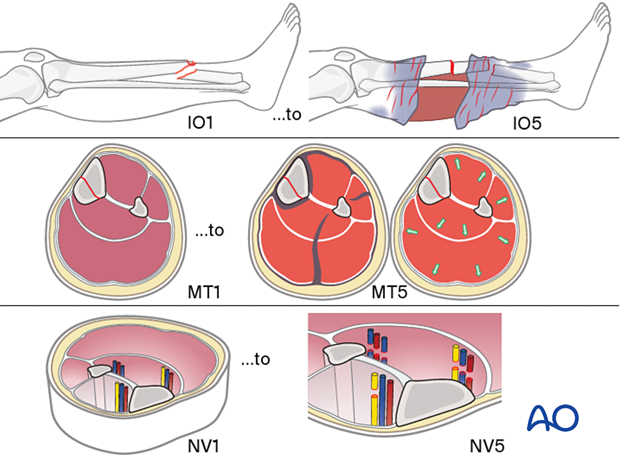
The AO classification of fracture wound severity provides a grading system for injuries of each of the following: skin (I), muscles and tendons (MT), and neurovascular (NV). Each of these classifications is divided into five degrees of severity.
This classification system is designed to provide a unique, unequivocal definition of any injury and, thereby, allows accurate comparison of cases.
A full understanding of the severity of an open fracture requires consideration of each of these soft-tissue elements.
This very detailed classification is designed to be used in conjunction with the AO/OTA Fracture and Dislocation Classification.
The detailed categorization of open fractures by the AO system is most reliably done in the operating room at the completion of primary wound care and surgical excision.
When used in a large database, this multifaceted, alphanumeric classification permits very precise comparison of injury types and is useful as a research tool. Nevertheless, its complexity renders it impractical for everyday use in clinical practice.
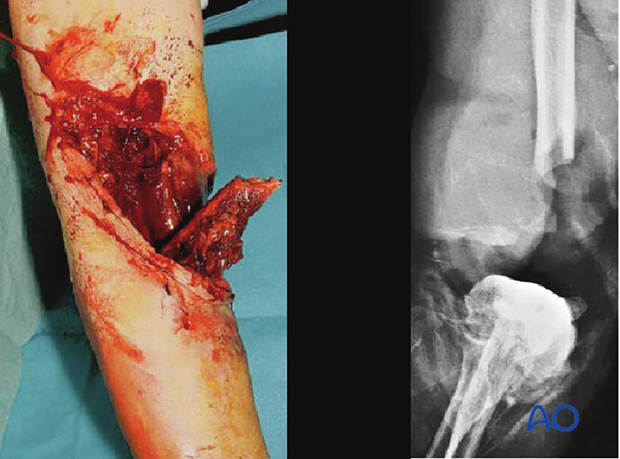
The Gustilo-Mendoza-Williams open-fracture classification separately identifies, as type IIIC, those grade III open fractures with arterial injuries that require vascular repair to restore limb viability. Gustilo et al. demonstrated a 50% risk of osteomyelitis after such injuries, with amputation (early or late) a frequent outcome (Gustilo et al. The management of open fractures. J Bone Joint Surg 1990 72(2):299–304).
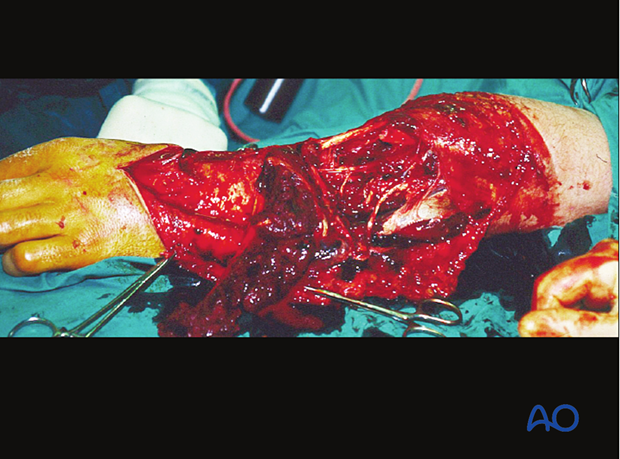
This illustration shows a severe open injury of the shaft of the lower humerus, after a high-energy motor vehicle collision. There was disruption of the brachial artery and vein and neurapraxia of the median, radial, and ulnar nerves. It would be classified as a Gustilo IIIC injury, whereas on the more comprehensive AO/OTA Fracture and Dislocation Classification it would be a 12-C3, IO4-MT4-NV4.
2. Principles of surgical care for open fractures
Introduction
Open fractures need:
- Prompt diagnosis
- Appropriate, immediate intravenous antibiotics
- Meticulous injury zone excision (debridement)*
- Fracture stabilization
- Second look surgery
- Early soft-tissue coverage after soft-tissue recovery
* Such a surgical procedure is frequently referred to as debridement. This term is open to interpretation and denotes different procedures in different surgical contexts.
Debridement, as used in this discussion, means the surgical exposure of the whole pathological injury zone and the removal of all necrotic, contaminated, and/or damaged tissue, whether bony or soft tissue.
Intravenous antibiotics for open fractures
Antibiotics for open fractures are an adjunct to meticulous wound debridement.
Bacterial contamination is always present with open fractures. Bacterial count and infection rate can be significantly reduced by prompt administration of intravenous antibiotics, in combination with surgical debridement.
Most infecting bacteria, except in very dirty wounds, are typical skin flora. A first-generation cephalosporin is often used, except for patients with a penicillin allergy.
For more severe open-fracture wounds, add an aminoglycoside.
If “agricultural” contamination is present, high-dose intravenous penicillin is usually added, and metronidazole can be considered.
Antibiotics should be started as soon as the open fracture is diagnosed but continued for only 2–3 days.
The following should be noted: “It is irrational to hope that a short course of antibiotic prophylaxis can cure fundamental surgical errors.” (Hell K. In: Geroulanos S, ed. Antimicrobial Prophylaxis in Surgery. Roche; 1989).
Intraoperative wound contamination
A key principle of safe surgical treatment is to minimize the number of bacteria that might enter the surgical wound. Appropriate preoperative skin decontamination with washing, using antibacterial agents, is a mainstay of this.
Similarly, the use of sterile drapes, instruments, and implants, and the maintenance of strict aseptic discipline throughout the procedure are also important.

In the absence of optimal sterility, or with overwhelming surgical load, only the most limited emergency surgery should be carried out (eg, emergency wound irrigation and debridement).

3. Debridement
Debridement of the injury zone in open fractures
The injury zone excision must be meticulous and complete. Early wound debridement is the most important component of the care of any open fracture.
The surgical site should be thoroughly irrigated (several liters of fluid – optimally, a balanced salt solution, such as normal saline or Ringer’s lactate – should be used to reduce the bacterial population). The saying, “dilution is the solution to pollution” has merit in this context.
In cases with significant amounts of contaminated, dead, or possibly ischemic tissue, additional surgical wound debridement 24–48 hours later (sometimes called a “second look”) is often necessary. If there is any doubt, take the patient back to the operating room to debride again.

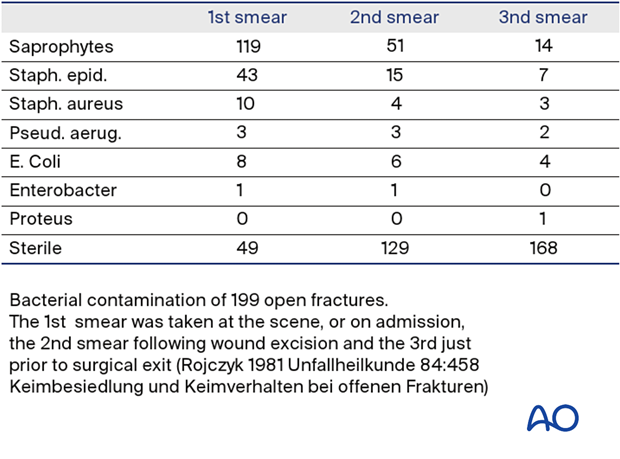
Tscherne and Gotzen refer to the work of Rojczyk (1981) as follows: “During the operation the wound is irrigated repeatedly with Betadine or Ringer’s solution. Following the debridement, all surgical instruments and attire are changed, and the wound is redraped as for a new operation. The benefits of this routine are demonstrated in a continuous series of 199 open fractures (see table). The number of positive microbiological smears decreases markedly from the initial contamination by the trauma to the end of the operation.”
Deciding which tissue to remove and which to retain is the essential challenge of wound debridement. This is best learned in the operating room from senior surgeons, and through supervised practice. Typical errors are failure to remove enough compromised tissue or doing so in a way that causes additional injury to retained healthy tissue.
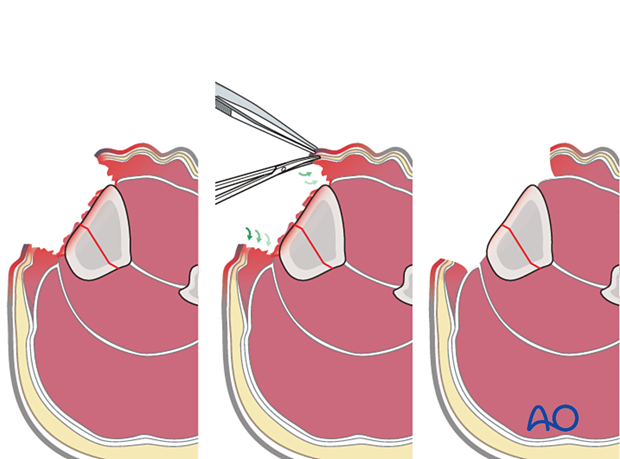
Take an organized approach that proceeds in orderly steps through each tissue layer. First, enlarge the traumatic wound for adequate exposure of the whole injury zone. Only non-viable wound margins need to be excised. Explore the depths of the injury zone and examine it thoroughly. Protect and preserve major blood vessels and nerves, tendon sheaths, healthy periosteum and soft tissue attached to bone.
Next, systematically excise all dead, or questionably viable tissue, from each layer:
- Subcutaneous tissues
- Deep fascia
- Muscle
- Bone
At each level, leave only obviously viable tissue.
Any bony fragments devoid of soft-tissue attachment should be removed. Contaminated, or non-viable, bone surfaces will also need excision.
Copious irrigation with a balanced salt solution (such as normal saline or Ringer’s lactate) helps to remove bacteria, fragments of dead tissue and blood clot, and improves the surgeon’s ability to examine the wound.
The use of pulsed pressure lavage systems risks driving contamination into hidden depths of the wound and is of questionable value.
See also:
- Bhandari M, Schemitsch EH, Adili A, et al. High and low pressure pulsatile lavage of contaminated tibial fractures: an in vitro study of bacterial adherence and bone damage. J Orthop Trauma. 1999 Nov;13(8):526–533.
- Hassinger SM, Harding G, Wongworawat MD. High-pressure pulsatile lavage propagates bacteria into soft tissue. Clin Orthop Relat Res. 2005 Oct:439; 27–31.
- Crowley DJ, Kanakaris NK, Giannoudis PV. Irrigation of the wounds in open fractures. J Bone Joint Surg Br. 2007 May;89(5):580–585.
Fractures with open joint injuries
When an open fracture communicates with a joint, special surgical tactics are required. As always, all devitalized tissue must be removed. Joint surfaces should not be allowed to become dry. If possible, the soft-tissue envelope over the joint should be closed to minimize subsequent contamination. If this is not possible, the joint must be kept clean and moist (using a moisture-retaining dressing). Early definitive closure should be planned.
4. Fixation of open fractures
Open fractures need the following:
- Surgical stabilization, either internal or external
- Delayed definitive open reduction and internal fixation (ORIF) if an appropriate debridement and primary wound closure is not possible
Bony stability in open fractures helps associated soft-tissue wounds to recover, by providing the best possible setting for soft-tissue healing and resistance to infection.
See:
- Worlock P, Slack R, Harvey L, et al. The prevention of infection in open fractures: an experimental study of the effect of fracture stability. Injury. 1994 Jan; 25(1):31–8
- Rittmann WW, Perren SM, Allgöwer M, et al. Cortical Bone Healing after Internal Fixation and Infection: Biomechanics and Biology. Berlin: Springer Verlag; 1975.

Surgical fixation, external or internal, is the best way to stabilize an open fracture. This is only done after thorough injury zone debridement.
For lower-grade open fractures, use fixation that would be appropriate for similar closed injuries. For more severe open fractures, or wounds that need repeated excisions, temporary fixation (external or internal) is usually preferable as it allows temporary stabilization and easier access to the bony and soft-tissue envelope during the subsequent surgical procedure.
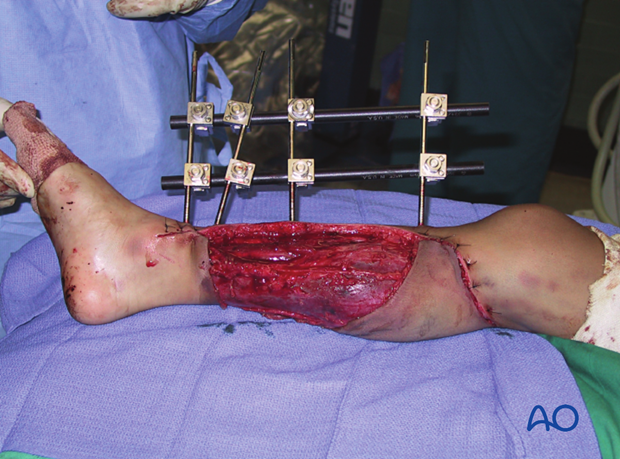
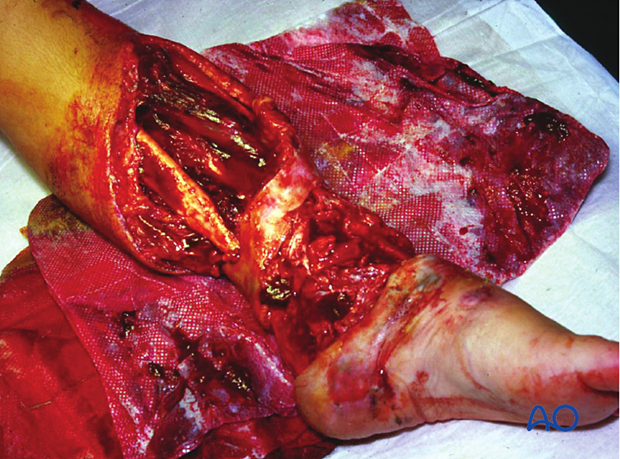
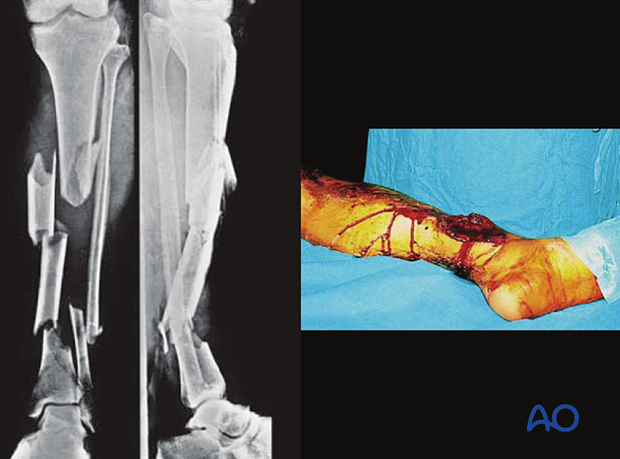
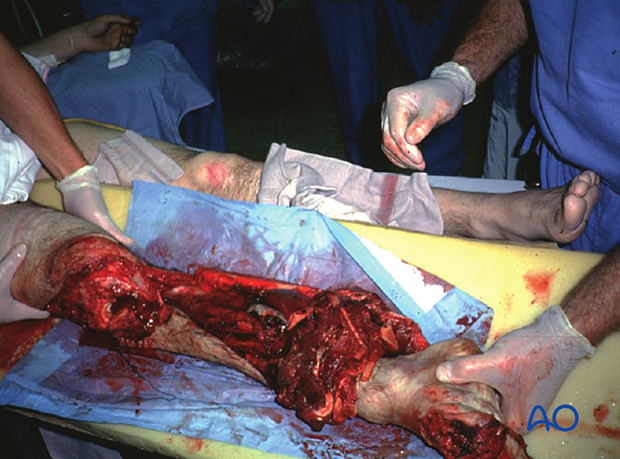
Intramedullary (IM) nailing can be chosen to manage open, complex fractures of the tibia. These images show a severe open segmental tibial fracture, in which IM nailing was performed.
If IM nailing must be delayed (due to significant wound contamination, etc.), temporary external fixation can be used for preliminary stabilization.
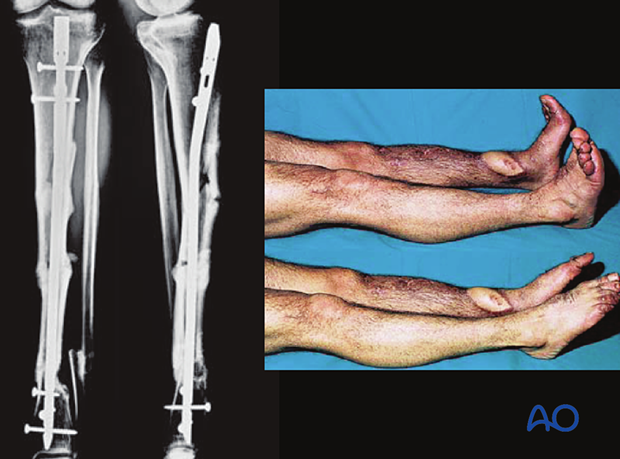
These images show the healed tibial fracture.
5. Soft-tissue care
Open wound care
When caring for open wounds:
- Avoid contamination
- Avoid desiccation
- Consider special dressings
- Cover promptly
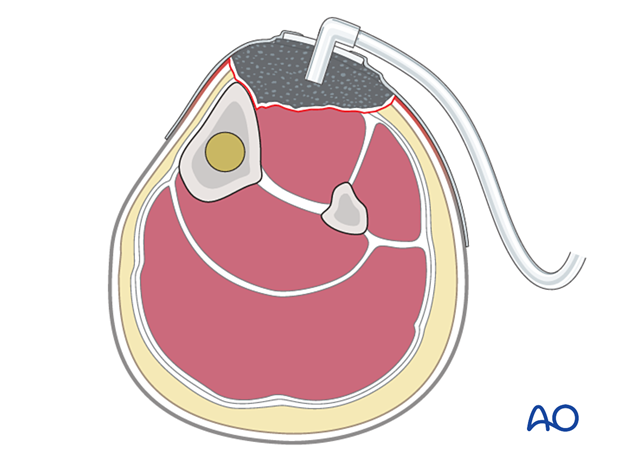
All open wounds need to be protected from secondary contamination. A sealed dressing (eg, an antibiotic bead pouch, or vacuum-assisted closure device (VAC)) can be used. VACs help to reduce the size of an open wound and promote the formation of granulation tissue. This device may permit early split-thickness skin graft closure.
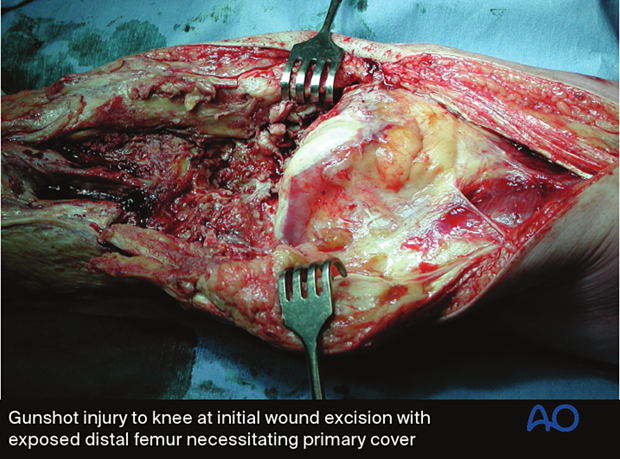
Closure with local or free flaps is appropriate for larger and more complicated wounds and for open joints, as soon as staged wound excision is complete.
It is important to close a complex wound, especially one that involves a joint, as soon as the wound appears healthy (preferably at 5–7 days), rather than leaving it open and risking further infection.
Soft-tissue coverage in open fractures
After wound debridement has been satisfactorily completed, in either one or more procedures, consideration must be given to the best means of wound coverage.
The following should be considered:
- Wound coverage should only take place after wound debridements are complete
- Delayed closure of the wound is safer in all open fractures
- Excessive skin tension will prevent wound healing
- A contaminated wound is almost certain to become infected with primary closure
Temporary open wound management with delayed primary closure, or preferably split skin grafting, is the safest approach for most open fractures.
Immediate wound closure can be considered with low-energy fractures and benign wounds. If primary closure is chosen, the surgeon must watch carefully for signs of wound infection.
If closure is delayed, it should be completed as soon as it is safe to do so, to minimize the risk of further contamination.

Caveat - Prof. Harald Tscherne 1984
- Incomplete excision of poorly vascularized tissue, especially muscle, skin, and bone
- Inadequate hemostasis and hematoma evacuation, and insufficient drainage of wound discharges and wound hematoma
- Devascularization of primarily viable tissue
- Large metallic fixation devices implanted under poorly vascularized tissue
- Wound closure under tension
- A failure to recognize compartment syndrome
Second look
Twenty-four to forty-eight hours after the original debridement, it is generally advisable to reinspect the injury zone under anesthesia. This is the so-called “second look.”
This affords an opportunity to do the following:
- Thoroughly inspect the injured bone and soft-tissue envelope
- Debride any remaining avascular tissue
- Wash out the remaining bone and soft tissue

6. Primary amputation
Primary amputation for open fractures
A mangled extremity is a life-threatening injury. Some extremity injuries are so severe that amputation is a safer option than attempted limb preservation. Injudicious efforts at limb salvage may lead to failure, with the risk of life-threatening complications, particularly infection.
Deciding whether to amputate, or to try to save, a severely injured limb is one of the most controversial choices in trauma surgery. The patient’s physical and emotional ability to tolerate injury and prolonged, extensive treatment must be taken into account.
The level of surgical resources at the disposal of the treating surgeon will also influence the choice.
Limb salvage usually requires multiple operations, prolonged hospitalizations, and frequently results in serious complications, ending with a painful and dysfunctional extremity.
Whenever possible, options and outcomes must be discussed with the patient and/or family at an early stage, either before amputation, or before starting out on a long and complex journey of reconstruction.
Because prostheses are generally more functional replacements for the lower than the upper limbs, additional risks may be worth considering to save a severely injured upper extremity, particularly in well-resourced health care systems.
Appropriate primary amputation usually results in a wound which heals satisfactorily, effectively prevents infection, and permits the possibility of an earlier return to function.

7. Modifiable risk factors
Poor nutrition
In the malnourished, dietary supplements, vitamins, and other forms of nutritional support should be instituted as soon as possible after emergency surgery.
Malnourished patients have difficulty healing wounds and resisting infection. Simple screening tests, such as total lymphocyte count, or serum albumen level, together with a careful dietary history and physical examination, help to identify patients with inadequate nourishment. Severe malnutrition should be corrected as soon as possible after the emergency surgery.
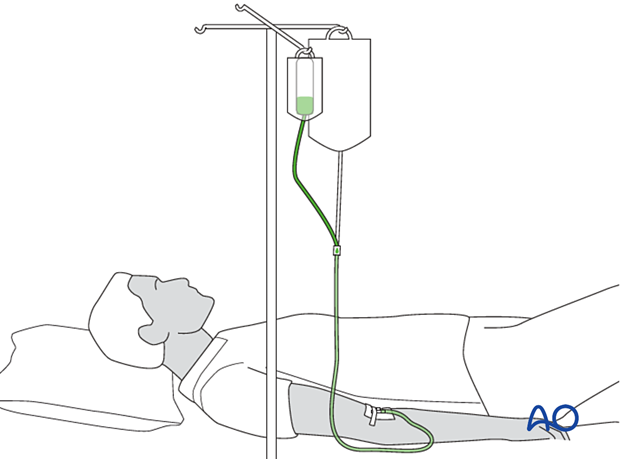
Temperature control
Should a patient’s core temperature fall during surgery, the risk of delayed soft-tissue healing, and the risk of infection becomes greater. For this reason, every effort must be made to minimize intraoperative heat loss, using appropriate covers and external warming devices.













