Classification of fracture wound infection
1. Classification of fracture wound infection
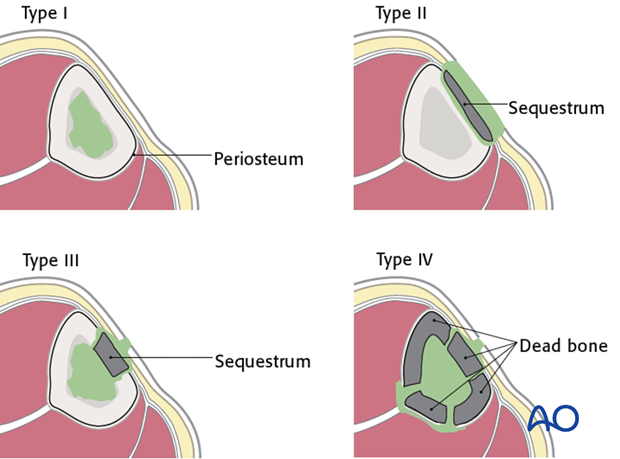
Cierny’s anatomical classification
The anatomical classification of osteomyelitis is important for understanding and localizing the infection.
- Type I (medullary osteomyelitis) diffusely involves the intramedullary cavity, usually after medullary nailing. The entire medullary canal is involved, and will require surgical clearance (nail removal and reaming).
- Type II osteomyelitis is superficial, may be present under a plate, but is rarely, if ever, seen with fracture-site infection.
- Type III osteomyelitis (localized full-thickness cortical involvement), will require excision of all necrotic bone. During the excision, the full extent of the necrotic area becomes evident. This may weaken the bone, or produce significant dead space. Soft-tissue cover may be inadequate and therefore require reconstruction. Fracture healing may be a problem requiring additional treatment.
- Type IV osteomyelitis diffusely involves the entire circumference of a segment of the bone. The entire bone segment must be removed to eliminate necrotic tissue and persistent bacteria.
Cierny’s classification of host resistance to infection
Patients vary in their ability to resist infection. In some cases, a patient’s response to infection is so impaired that all efforts at treatment fail. To understand the problem of posttraumatic infection, it is important to assess each patient’s immunocompetence.
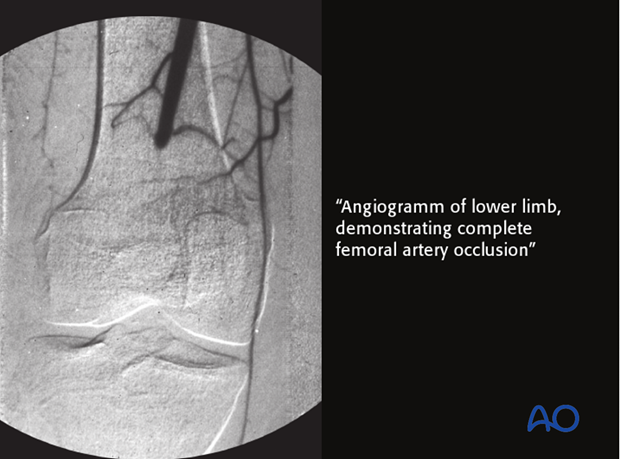
Local factors are limited to the site of infection and include focal arterial insuffiency, venous stasis, previous radiation therapy, etc.
Systemic factors that impair host resistance include smoking, malnutrition, diabetes mellitus, renal failure, chronic steroid use, HIV/Aids, etc.

Cierny has also suggested a classification scheme according to host resistance. Both local and systemic factors may be involved. This classification identifies the uncompromised patient as Class A. If significant compromise is identified, the patient is class B, either based on local factors (BL), systemic factors (BS), or both (BL,S).
Class C patients are either so compromised that the risks of treatment outweigh the benefits, or the symptoms of their infection are sufficiently limited that surgical treatment is not indicated.
See also Cierny G 3rd, Mader JT, Penninck JJ (2003) A clinical staging system for adult osteomyelitis. Clin Orthop Relat Res.(414):7-24.
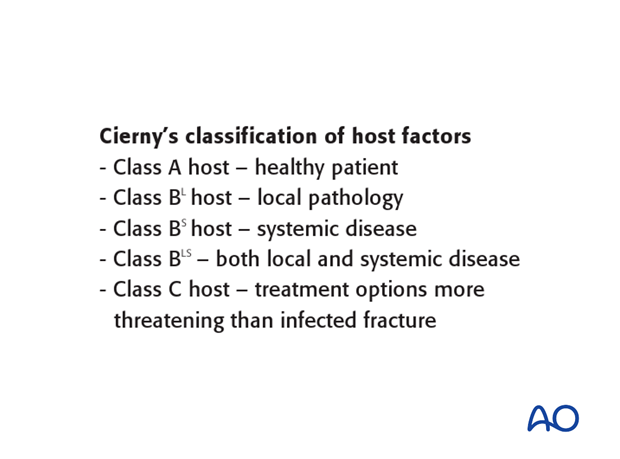
Class A host
Class A hosts are healthy patients. Their infection was not the result of impaired systemic host resistance. It must be remembered that a very severe injury can result in a focal defect of host resistance, because of locally impaired vascularity and tissue damage. An otherwise healthy patient with this degree of persisting local damage belongs in class BL.
Class A hosts are usually able to tolerate any appropriate surgical procedure. Tissue response to infection is strong, soft-tissue viability is excellent, and healthy tissue is available for transfer.

Class BL host – local disease
A class BL host has locally compromised soft tissue, or bone. The patient’s injury, or previous surgery, or both, may compromise tissue healing. For example, the patient may have had radiation, or previous injury to this region. Other potential local impairments are vascular disease or lymphedema, which impair wound healing and response to infection.
Localized ischemia may be correctable with arterial reconstruction, with improvement of host resistance classification.
BS host – systemic disease
Many systemic diseases can reduce a host’s ability to fight infection. Extremes of age, malnutrition and obesity are three common examples. Systemic diseases such as diabetes, renal or liver failure also impair tissue response to infection. Smoking, alcohol, steroids, etc. also compromise host resistance.
With such patients, every effort must be made to identify and treat the systemic problems, but it is not always possible to restore normal host resistance. In practice, when dealing with an active infection, it is appropriate to begin treatment by drainage, surgical clearance, minimally invasive fracture stabilization (external fixation), and appropriate antibiotics. Preferably, impaired host resistance should be improved before definitive surgical reconstruction. If this is not possible, treatment failure and/or amputation become likely.
Class C host – poor surgical candidate
Class C patients are either so compromised that the risks of treatment outweigh the benefits, or their symptoms of infection are sufficiently limited that surgical treatment is not justifiable.

Classification according to microbiology
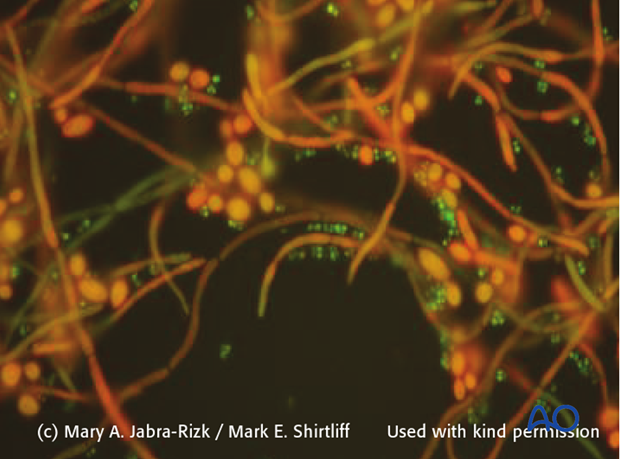
See also the General introduction – planktonic and biofilm micro-organisms.
Like all infections, those involving fracture wounds can be classified according to the infecting organisms. Adequate specimens, taken at surgery from several representative locations, and properly processed by a microbiology laboratory, are necessary to identify the causative organism(s), and antibiotic sensitivities. Special sensitivity testing may be necessary, particularly with potentially resistant organisms.
The most common microorganism causing posttraumatic infection is the gram-positive staphylococcus. Worldwide, methicillin-sensitive S. aureus (MSSA) is most common. In some areas, methicillin-resistant S. aureus (MRSA) is a major problem, particularly in postoperative infections and institutionalized patients.
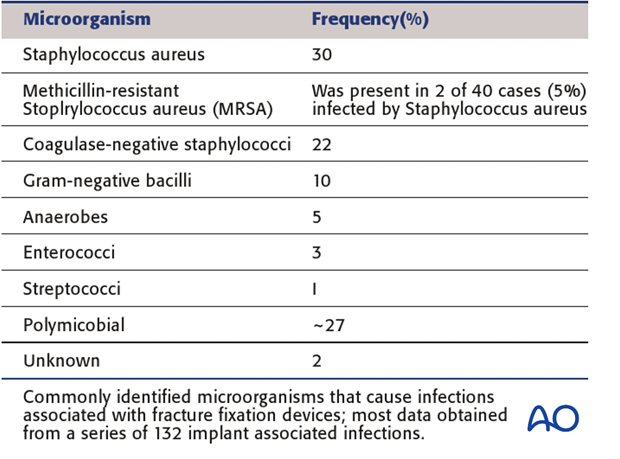
Gram-negative bacilli occur in 10% of such infections, usually with open fractures and hospital-acquired infection. Polymicrobial, or mixed, infections (25%-30%) are actually more common, and may require prolonged, complex treatment.
Remember that an organism initially present may be replaced, or joined, by other bacteria during treatment, adding to the challenge of correct antibiotic selection.
Antibiotics are a valuable adjunct to the surgical treatment of post-traumatic infections. However, the overriding principle is that adequate clearance of all infected and nonviable tissue is the most important factor. Macroscopic quantities of planktonic and biofilm bacteria are reduced by surgical removal– so-called bioburden reduction. Antibiotic administration suppresses bacterial growth and helps to eliminate any residual bacteria at the cellular level.
Unless a patient is septic, with a life-threatening infection, it is desirable to obtain culture specimens before beginning antibiotics, in order to maximize the likelihood of correct identification and sensitivity-testing of bacterial pathogens.
Classification according to status of fixation
Fracture wound infections are influenced by factors involving the fracture and its prior treatment. Infections interfere with fracture healing. Infections are more difficult to eradicate in the presence of nonunion. Treatment plans must take into account any nonunion, with decisions about bone resection, stabilization, bone grafting, etc.
Fracture fixation devices impair host resistance. If they provide absolute stability, this benefit may outweigh their detrimental effects, and in carefully selected cases (low-virulent organisms and healthy tissues), the internal fixation implants may be retained. Titanium implants are generally more resistant to bacterial adhesion.
If there is instability, or if the infection fails to resolve promptly, plates and screws, or intramedullary nails, should be removed, and the fracture restabilized, using external fixation.













