Approach to the posteromedial surface of the tibial shaft
1. Indications
The posteromedial approach can be used for open plate fixation of the tibia on its posterior surface. Typically, this approach would be chosen when direct exposure for open reduction and internal fixation (ORIF) is desired, but only the posteromedial soft tissues are safe to incise.
Note that this incision can also be used for a medial fasciotomy for compartment decompression. Further information on compartment syndrome can be found here.
The posterior surface of the tibia is relatively flat and therefore little contouring of the plate is necessary.
This approach allows access only to the tibia, not the fibula.
2. Positioning
The patient may be positioned either supine or prone. When positioned supine, the patient’s leg must be flexed at the knee and externally rotated at the hip to provide good exposure. In the prone position, the leg requires less manipulation.
3. Anatomy
The lateral and posterior surfaces of the tibia are covered by muscle. The anteromedial surface has only a thin layer of subcutaneous tissue and skin. This surface provides less blood supply to the underlying bone.
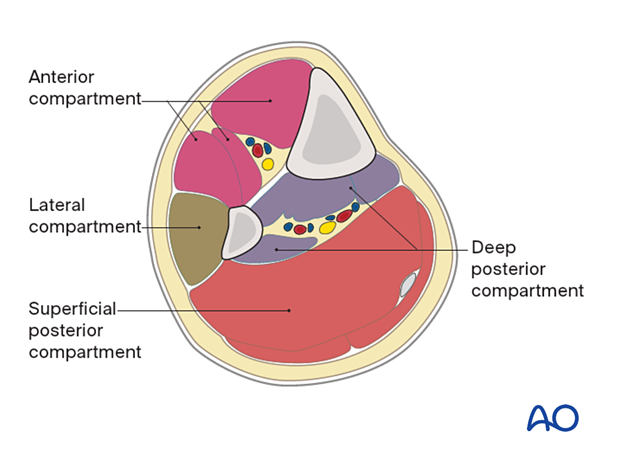
The lower leg has four compartments:
- Anterior
- Lateral
- Deep posterior
- Superficial posterior
The anterior compartment has three muscles, one main artery, and one nerve: the tibialis anterior, extensor hallucis longus, extensor digitorum longus, the anterior tibial artery, and the deep peroneal nerve.
The lateral compartment has two muscles and one nerve: the peroneus longus and brevis, and the superficial peroneal nerve.
The deep posterior compartment has three muscles, two arteries, and one nerve: the tibialis posterior, flexor hallucis longus and flexor digitorum longus, and the peroneal and posterior tibial arteries, as well as the tibial nerve.
The superficial posterior compartment has two muscles and one nerve: the gastrocnemius, the soleus, and the sural nerve.
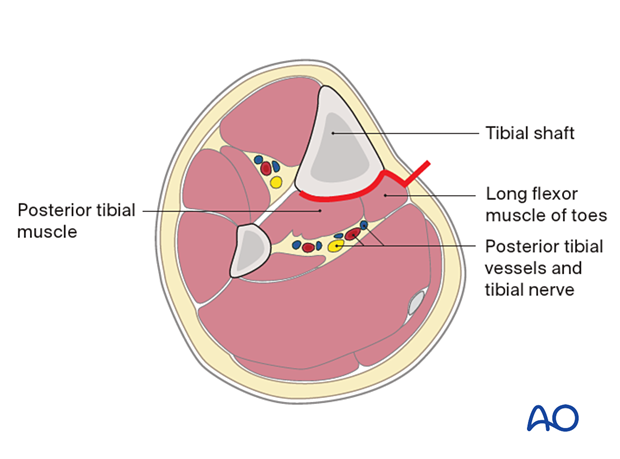
4. Skin incision
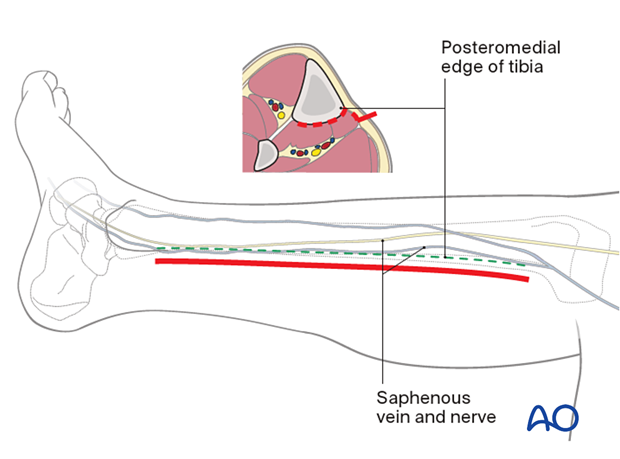
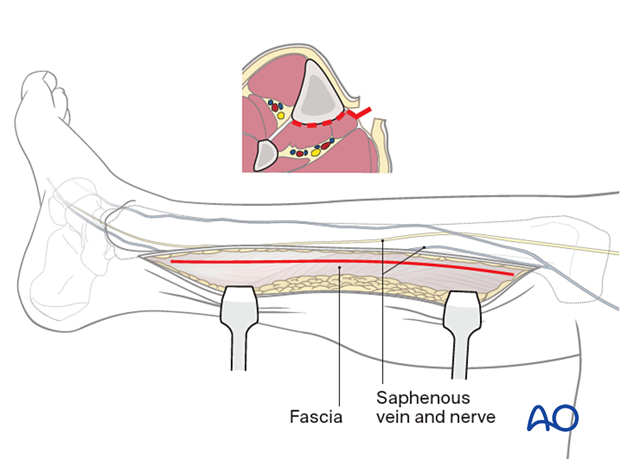
The length of the incision varies according to the fracture location and the plate selected. Minimally invasive incisions are safe in this region and should be considered. The posteromedial border of the tibia is first palpated throughout its length. The incision is then made in parallel 1–2 cm posterior to the posterior tibial border.
5. Dissection
Subcutaneous dissection is carried out carefully so as to identify and/or protect the saphenous vein and nerve. These are typically mobilized anteriorly.
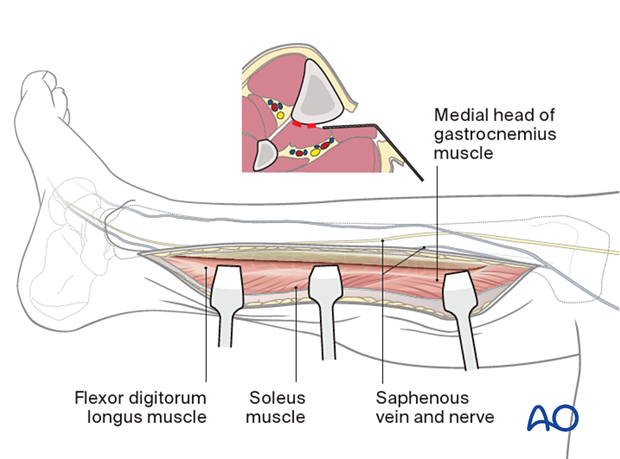
The fascia is then incised in line with the skin incision and the superficial and deep posterior compartments are mobilized. The gastrocnemius, soleus, and flexor digitorum will be identified and mobilized with a soft-tissue elevator, depending on the level of the fracture.
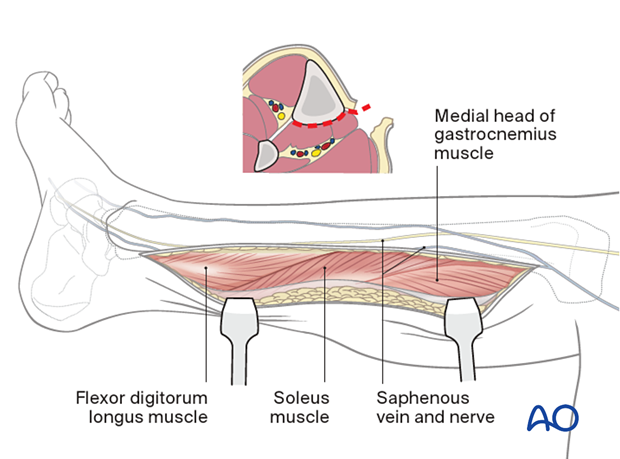
The dissection should be done in an extra-periosteal plane.
Dissection is not necessary beyond the posterolateral aspect of the tibia.
In this way, the middle 3/5 of the posterior tibia can be effectively exposed.
6. Wound closure
The deep fascia should almost always be left open to minimize the risk of a compartment syndrome affecting the deep posterior space. Only the skin and subcutaneous layers are closed.













