Bridge plate fixation
1. Principles
Comminuted fractures
Comminuted fractures are most often the result of a crushing type injury.
The associated soft-tissue lesions carry the potential risk of edema, fibrotic reactions and eventual stiffness.
For these reasons, these injuries are usually treated by ORIF, in order to provide sufficient stability for immediate mobilization, reducing the risk of joint stiffness and tendon adhesions.
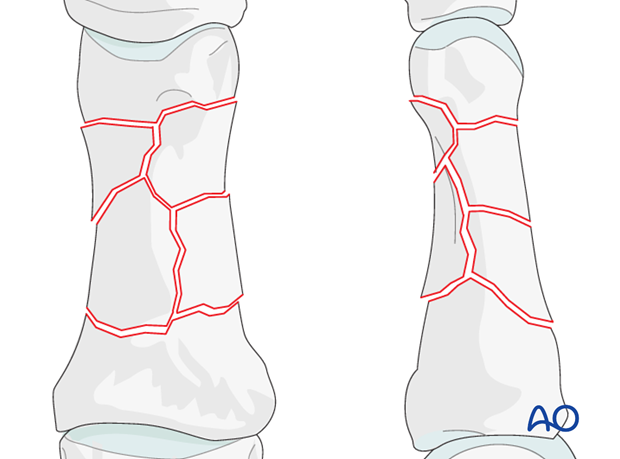
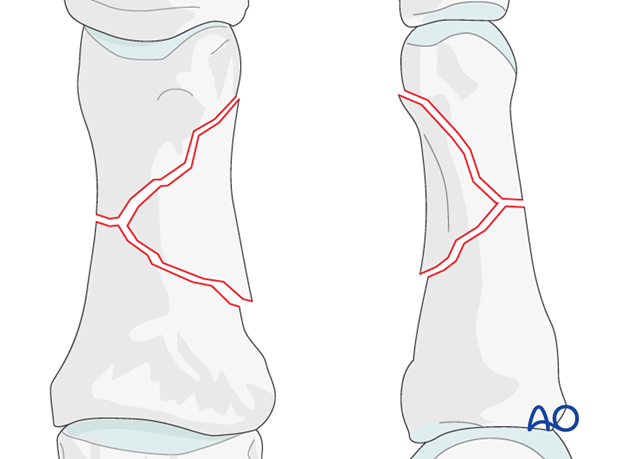
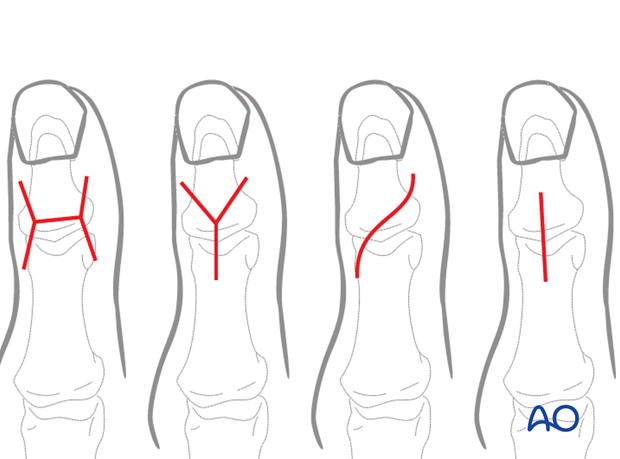
Depending on the forces acting on the bone, two kinds of comminuted fractures are common: small fragment comminution, or wedge fractures.
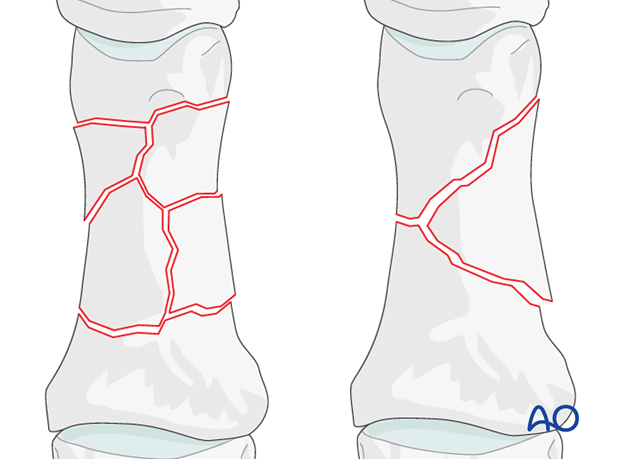
Small fragment comminution
Even in the hand, which has a good blood supply, small fragment comminution is associated with poor soft-tissue attachments to the fragments and, thereby, compromised vascularity.
Wedge fracture
The degree and type of comminution depends on the forces and energy acting on the finger. In cases where a large wedge fragment has resulted from the injury, vascularity is less likely to have been compromised.
2. Approach
For this procedure a dorsal approach to the IP joint of the thumb is normally used.
3. Reduction
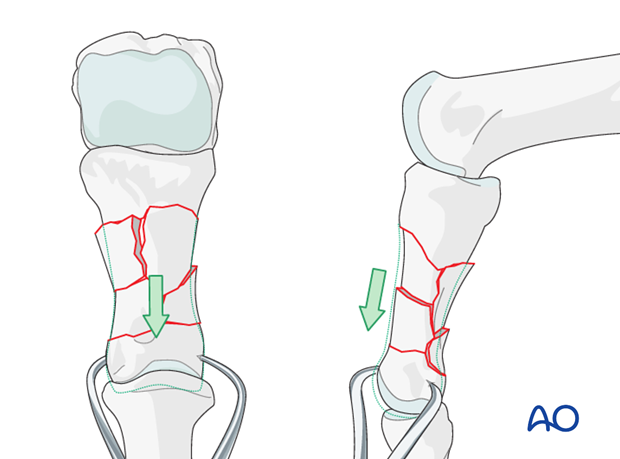
Restoring length by traction
Length can be restored by traction applied either manually by the surgeon, using a finger trap, or with pointed reduction forceps.
Provisional K-wire fixation
Provisional fixation can be provided by an intramedullary K-wire, inserted through the head of the metacarpal, with the metacarpo-phalangeal joint in 90 degrees of flexion, through the base of the phalanx and into the head of the proximal phalanx.
Great care must be taken to control rotational alignment.
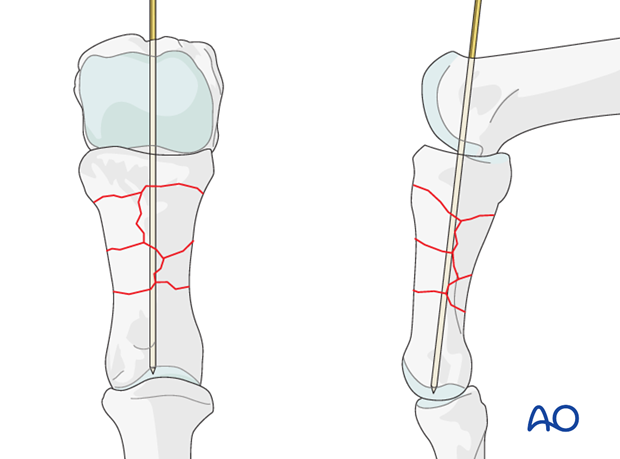
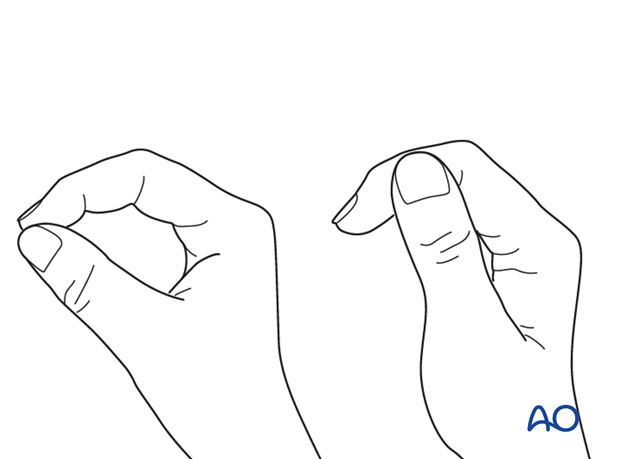
Correct rotation of the thumb can be difficult to judge. Make sure that the tip of the thumb correctly reaches the tip of the index finger for tip pinch and the lateral side of the second phalanx of the index finger in key pinch.
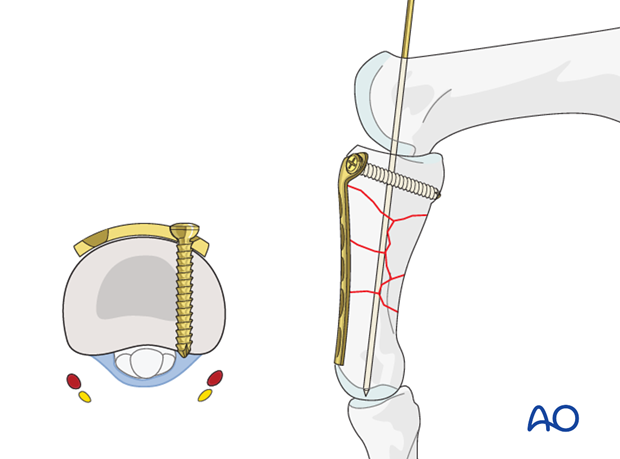
4. Fixation: Proximal
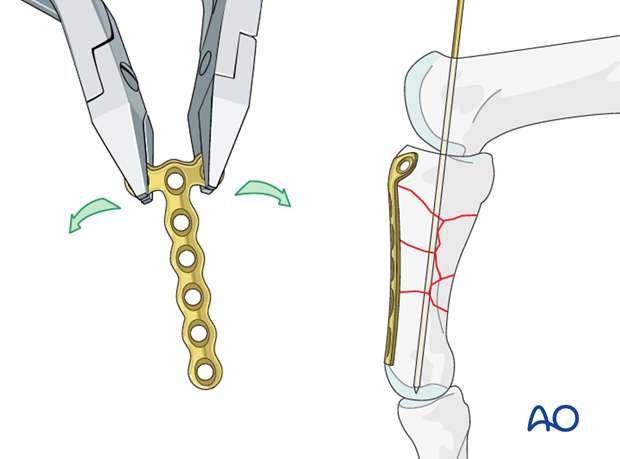
Bending and contouring the plate
The plate is contoured exactly to replicate the shape of the normal dorsal surface of the phalanx.
The T-end of the plate must be bent to follow the convexity of the dorsal surface of the base of the phalanx.
Drilling
Using a drill guide, carefully drill a first hole for a screw through the transverse part of the plate using a 1.0 mm drill bit.
Pitfall
Be sure not to injure the flexor tendons, the digital artery and nerve by overpenetration of the drill. The screw must not protrude into the joint.
Measuring
Use a depth gauge to determine screw length.
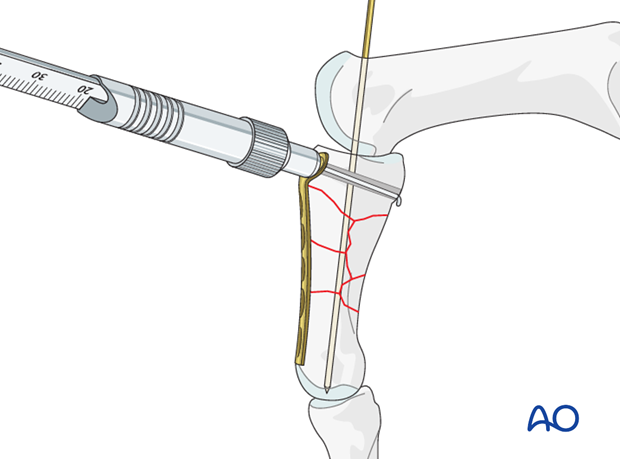
Plate application
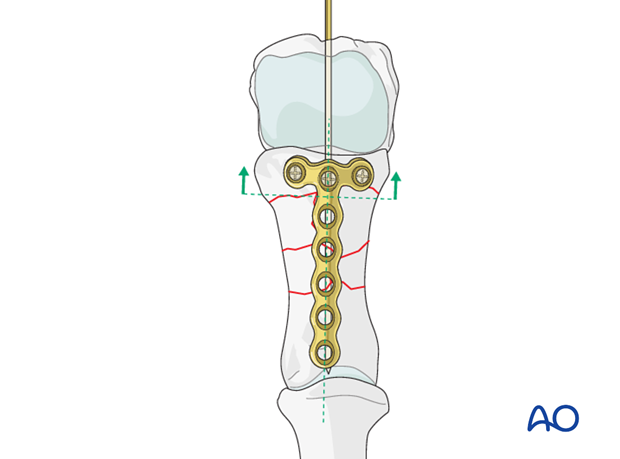
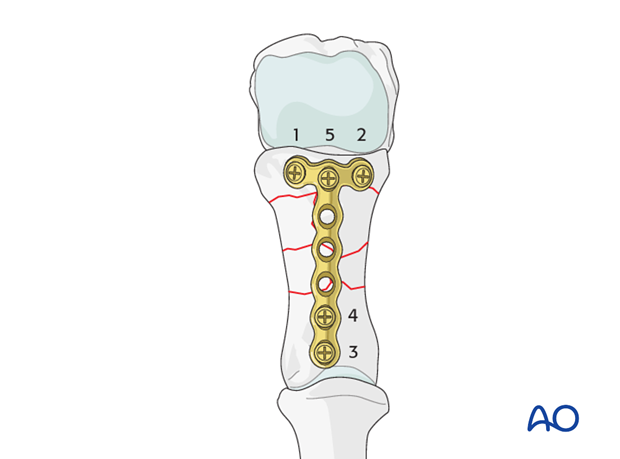
The plate is placed dorsally on the phalanx, proximally enough from the comminuted area to allow for at least 2 screws to be inserted into the metaphysis.
Ensure that the plate is centered on the long axis of the diaphysis.
Screw insertion (proximal)
Insert the first screw but do not tighten it fully. Ensure that it engages the far cortex, but does not protrude into the fibro-osseous flexor digital tunnel, through which the flexor tendons run. The digital nerve and artery are also at risk of injury.
Check the position of the transverse part of the plate in relation to the metaphysis and to the long axis of the bone. Then drill the hole for the second screw in the opposite lug of the transverse part of the plate.
Insert the second screw, alternately tightening both screws.
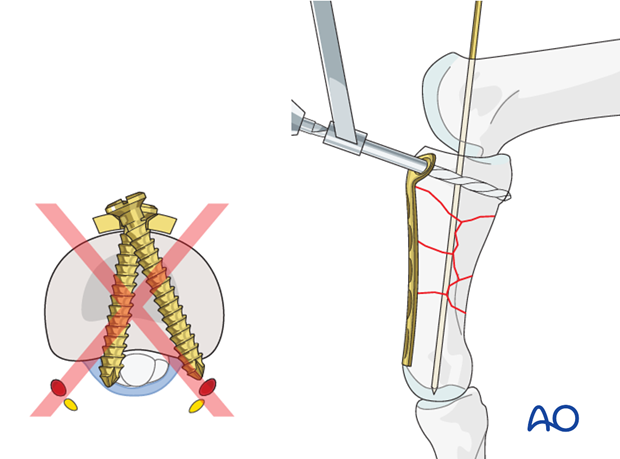
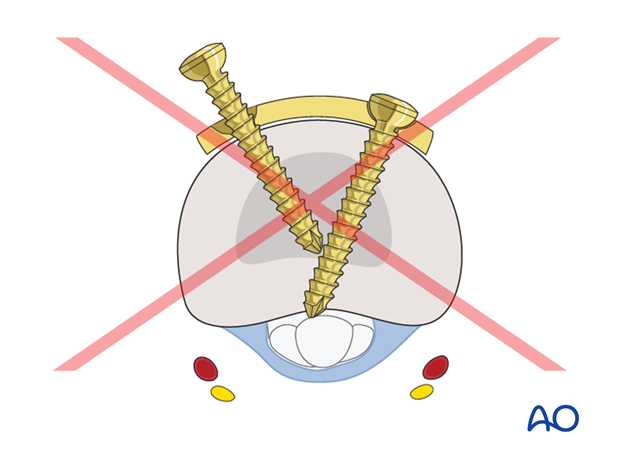
Pitfall: Interfering screws
Conflict of the tips of the screws in the transverse part of the plate, and joint penetration must be avoided.
Correct malrotation
With the plate securely fastened to the base of the phalanx, now is the time to manipulate the distal part of the phalanx to correct any malrotation of the distal part.
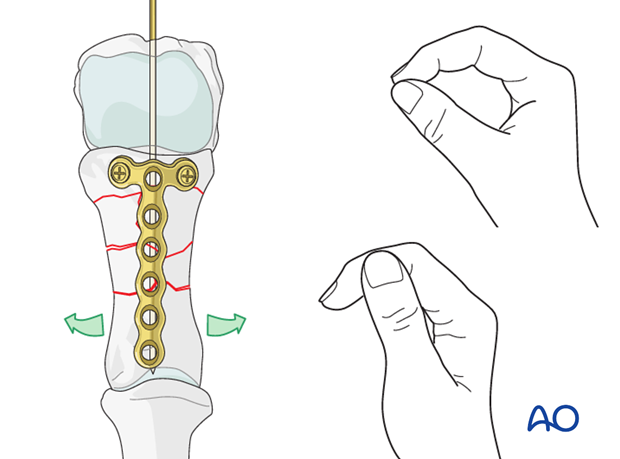
5. Fixation: Distal
Drill for distal screws
Partially withdraw the provisional K-wire, sufficiently to prevent interference with drilling the most distal hole.
Use a drill guide and 1.0 mm drill bit to prepare neutral holes for the distal plate screws.
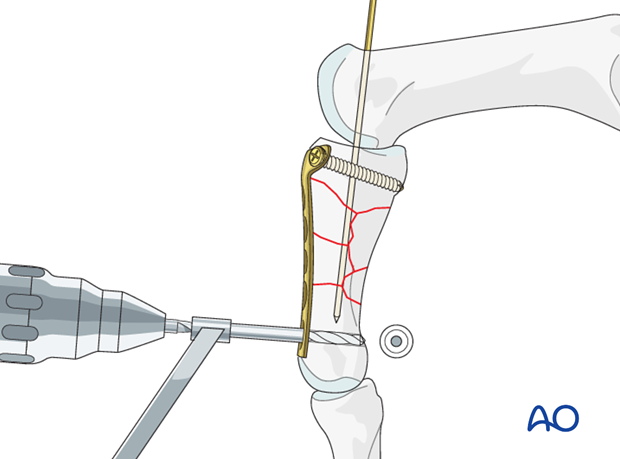
Measure screw length
Use a depth gauge to determine screw length.
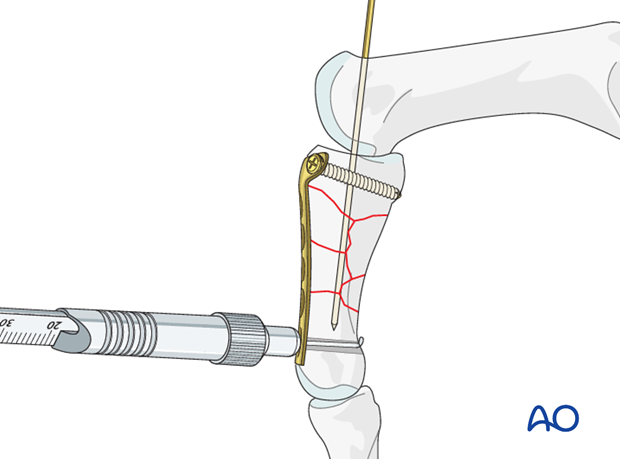
Screw insertion
Insert the most distal screw, and tighten it.
Retract the K-wire a little further to allow drilling for and insertion of the second distal screw.
At this stage, length, alignment and rotation have been controlled.
Remove the K-wire.
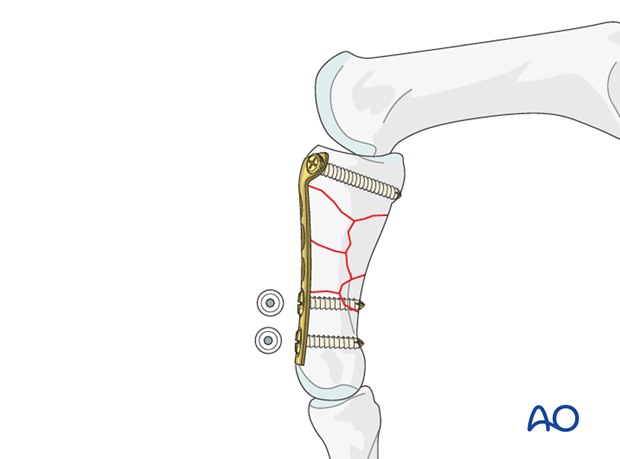
Additional proximal screws
Now insert the middle screw in the transverse part of the plate after the same fashion.
If the fracture configuration allows, insert a further screw through the next plate hole, but be sure not to enter the comminuted zone.
6. Aftertreatment
Orthoplast splint
In compliant patients, a well-padded orthoplast splint is sufficient for immobilization. This has the advantage of leaving the wrist free.
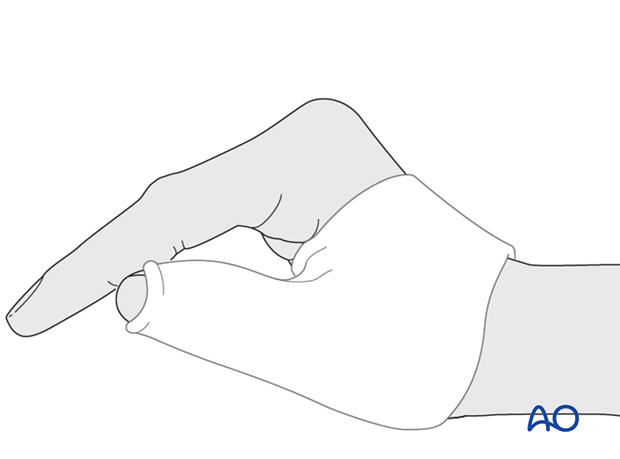
Thumb spica
In noncompliant patients, a more restrictive well-padded thumb spica cast may be a wiser choice.
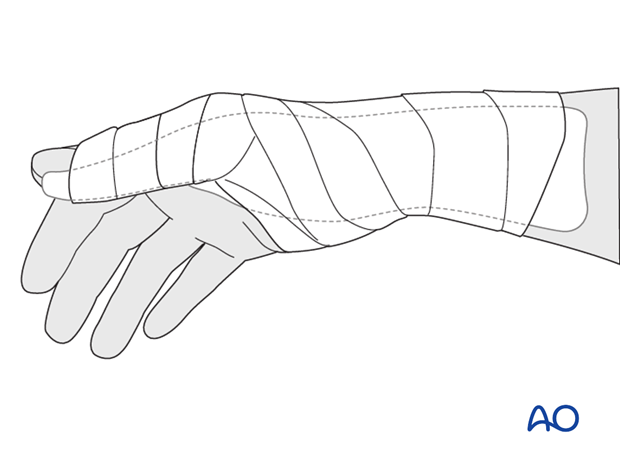
Splintage
Immediately postoperatively, a temporary plaster splint is applied which immobilizes the first MCP joint as well as the wrist. When the pain and swelling have reduced, a custom thermoplastic splint is applied for a period of time, depending on patient comfort and fracture stability.
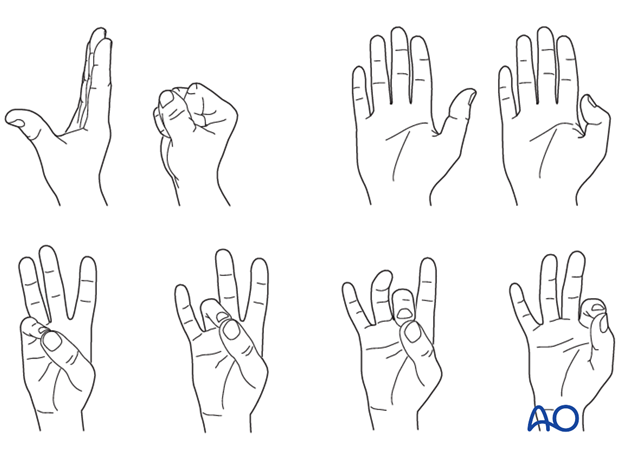
Functional exercises
In compliant patients with stable fixation, the splint can be removed under the supervision of a physical therapist, and early active motion exercises of the thumb and the fingers started after a few days.