ORIF - Screw fixation
1. Anatomy
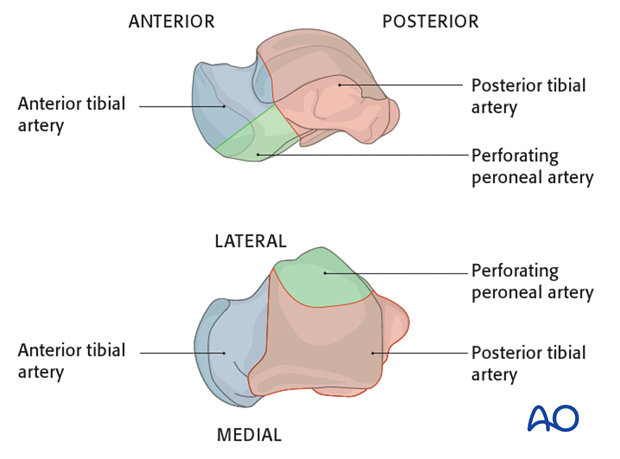
The blood supply to the talus is very compromised with a fracture dislocation scenario. The posterior tibial artery has branches medially. The dorsalis pedis has branches anteriorly. The peroneal artery has branches laterally. They are all connected through a sling of vessels that lie within the sinus tarsi.
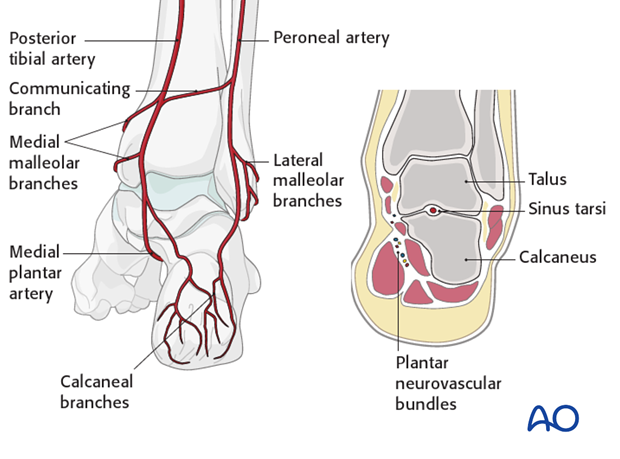
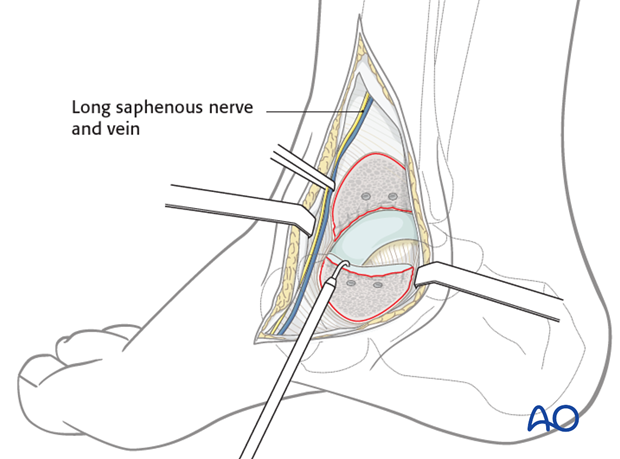
The deltoid branch of the posterior tibial artery must be protected. It is an important point for blood supply entry into the medial talus. This is the reason why a medial malleolar osteotomy is successful as it protects the talar blood supply.
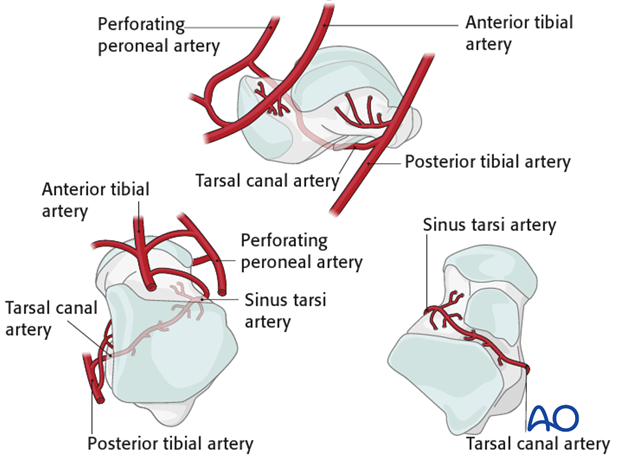
The deltoid branches are important to supply blood to the medial talar neck and talar body. Branches from the dorsalis pedis supply the talar head and most of the dorsal talar neck. The artery of the tarsal canal coming from branches off of the posterior tibial artery supply most of the talar body.
The peroneal artery has the least contribution laterally.
2. Decision making
If the talar neck fracture is undisplaced and all joint surfaces are in perfect alignment, then nonoperative treatment is a rational choice.

If the fracture is displaced, then it is often associated with other hindfoot injuries. This will lead to more decisions about further investigation and other forms of treatment.
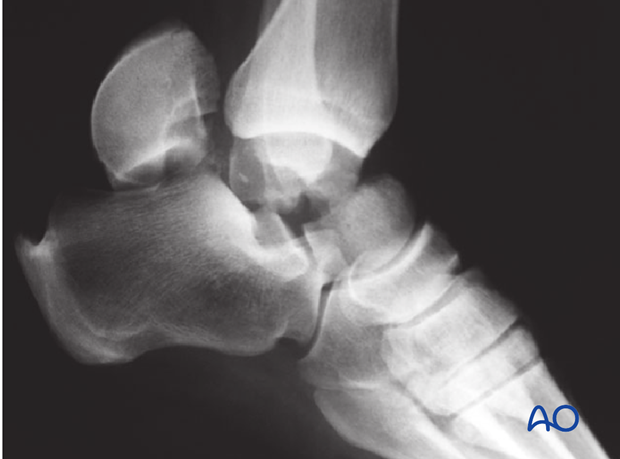
Plain x-rays may be all that is required if the fracture is undisplaced. This, however, is unusual as most talar neck fractures present with at least some displacement.
CT examination is very helpful whenever there is any question about displacement, or requirement for debridement of the subtalar joint. Along the spectrum of injury, increasing displacement presupposes that there is more subtalar and tibiotalar osteochondral injury. This often requires surgical approaches for debridement and fixation of these fracture types.

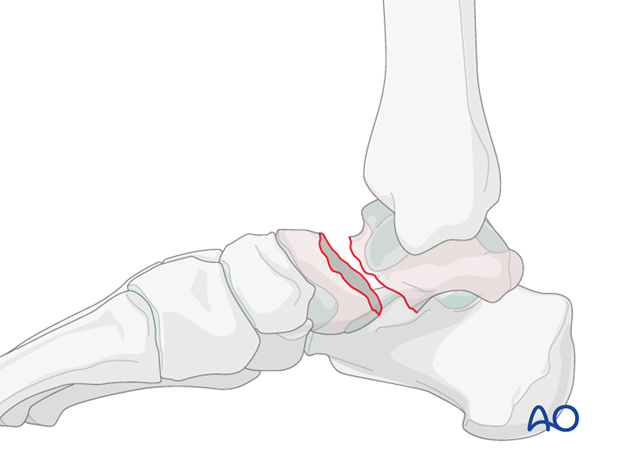
3. Closed reduction
Introduction
Where possible, after the diagnosis of a displaced talar neck fracture, where soft tissue is compromised, a closed reduction must be attempted. This is mandated because soft-tissue and skin compromise may occur if deformity is not reduced. If there is no soft-tissue compromise and the joints are not dislocated, then surgical intervention can be delayed.
A second reason for early closed reduction of talar neck fractures is the importance of the blood supply to the talar neck and body. The complex blood supply is further compromised the longer the displacement, or dislocation, of the fragments is maintained.
However, closed reductions become increasingly difficult with increasing severity of a talar neck fracture. Type 2 talar neck fractures will only have successful closed reduction 30-60% of the time.
The closed reduction does not have to be anatomic. Soft tissues will be protected while further investigation is performed.
Closed reduction technique
Which side is injured is obvious by looking at the foot that it is swollen and deformed. It is useful to look at the patient’s other normal foot to determine individual anatomy.
The talar body will stay with the tibia, yet the talar head and calcaneous will sublux medially or laterally.
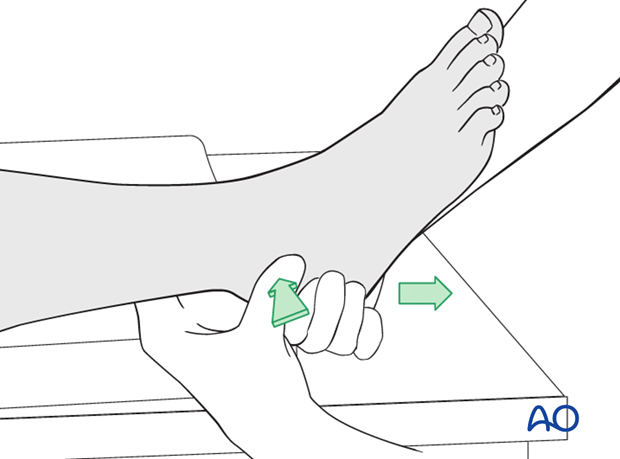
Traction
The reduction maneuver is facilitated by longitudinal traction and reversal of the force and its direction.
If successful, normal anatomy will be restored. The deforming force may have been a medially directed force, or laterally directed force, depending upon whether this is a medially or laterally displaced injury.
Usually, with type 2 talar neck fractures, a successful reduction is accompanied by reestablishment of normal foot anatomy.
Splintage with follow-up radiology will now determine whether the closed reduction is successful.
Multiple attempts of closed reduction are not advised as they can further injure the soft tissue.
4. Open reduction
Introduction
Type 3 talar neck fractures are usually non-reducible in a closed fashion, but efforts should still be made as occasionally (< 25%) the procedure is successful.
Type 4 talar neck fractures are similar to type 3 neck fractures.
Rarely, type 2 talar neck fractures are open fractures, but 50% of type 3 talar neck fractures present as open injuries.

Teaching video
AO teaching video: Talar fractures: reduction and screw fixation
Exposure
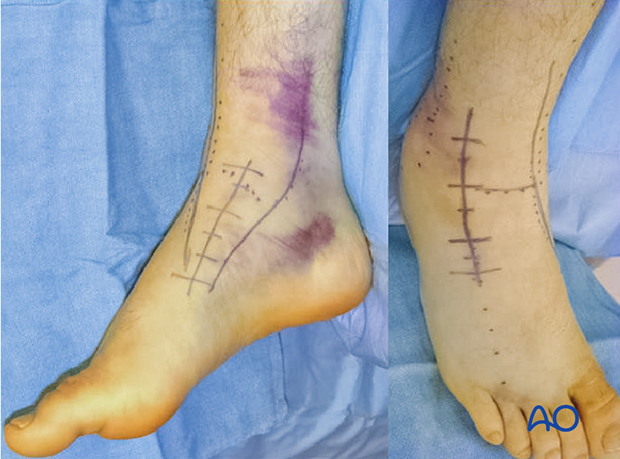
The combined anteromedial and anterolateral incisions are optimal for all talar neck fractures that are treated operatively. These two exposures ensure adequate visualization for reduction and fixation.
Helpful adjuncts in surgery when doing an open reduction include joysticks, external fixator, small distractor, or lamina spreader. A headlamp helps with visualization, and an image intensifier will guide the reduction of this difficult fracture.
If a reduction can not be achieved with the standard two anteromedial and anterolateral approaches, then a medial malleolar osteotomy is the most common tactic that is used.
An alternative oblique lateral approach is another option.
The medial malleolar osteotomy is performed by extending the anteromedial approach to provide access for the osteotomy. Remember that the deltoid ligament and the osteotomy fragment must be kept as one to preserve blood supply to the talar body.
Open manipulation
Care should be taken to preserve all soft-tissue attachments (blood supply) to the talar body.
Two approaches should be used.
When the combined approaches are used and the reduction can not be obtained, then there is a series of steps for successfully obtaining the reduction.
Firstly, elevators and joysticks are advised, followed by the use of external fixators and distractors.
Lastly, the medial malleolar osteotomy would be performed as the most invasive, yet most definitive tool.
Image intensification would be used at every step.
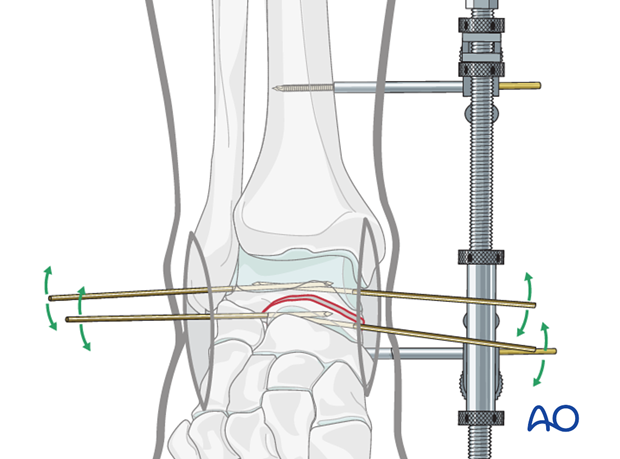
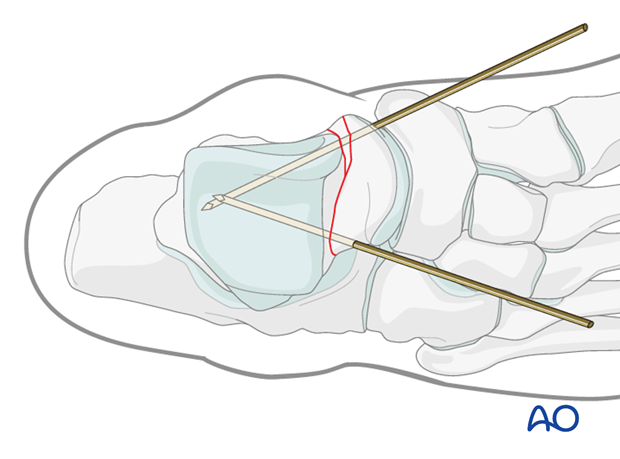
The images demonstrate a medial distractor with a patient under general anaesthetic with maximum muscle relaxation. The talar neck fracture has been reduced by distraction using the distractor which allowed derotation and reduction of the body into its anatomical position.
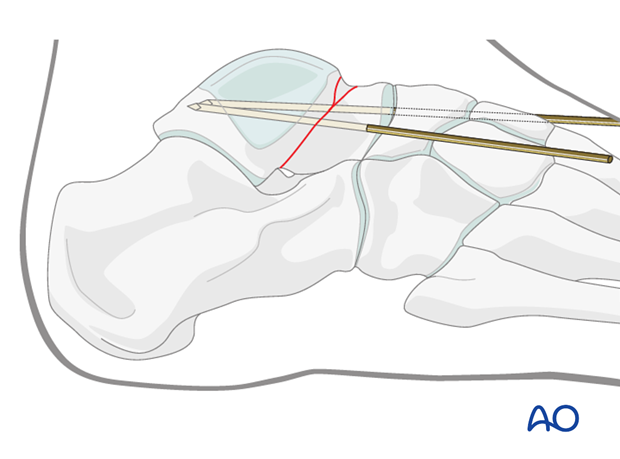
The second image demonstrates the talar neck reduction with tibiotalar distraction still maintained.
5. Fixation
Preliminary fixation
Lateral side
K-wires are helpful to achieve preliminary fixation. K-wire placement is very important when using cannulated screws, as the position of the wires can help with definitive screw fixation.
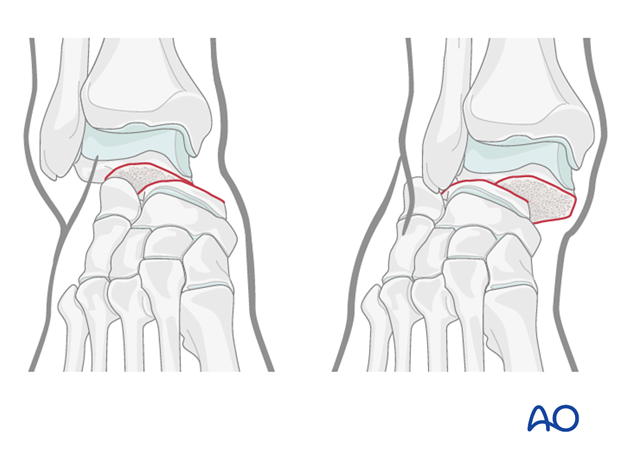
The lateral talar neck is usually not comminuted and can be reduced using fracture interdigitations. Screw fixation is appropriate in compression mode on the lateral side.
Medial side
The medial talar neck is often somewhat comminuted and can be reduced by using image intensification as a guide. For fixation, one should use a fully-threaded cortex screw in a position fashion. A lag screw would displace and shorten the medial side of the talar neck upon tightening.
This medial K-wire is often best placed through the medial portion of the talar head articular cartilage allowing for countersinking of a future screw.
Screw fixation
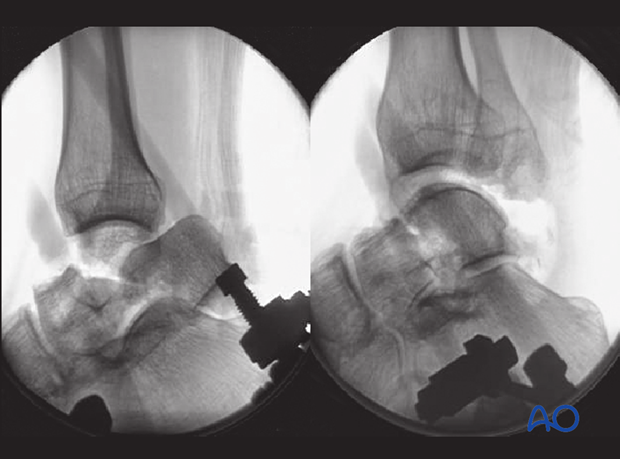
With the K-wires placed appropriately and with image intensification verifying accurate reduction, cannulated screws can be placed over the K-wires.
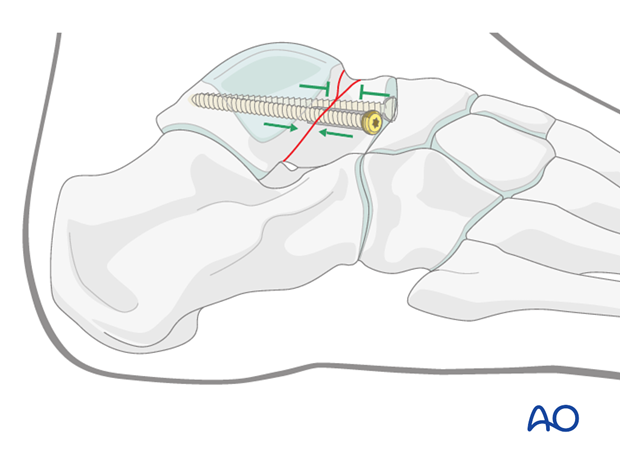
Medially, where comminution is common, one should avoid lag effect and the screw is placed without compression (position screw). The screw head on the medial side is often countersunk through the medial edge of the talonavicular articular surface.
The lateral side, with no bone loss and interdigitation of the bone, which can withstand compression, is best treated with a cannulated lag screw. The screw on the lateral side is not inserted through articular cartilage but through bone on the lateral side of the talar neck.
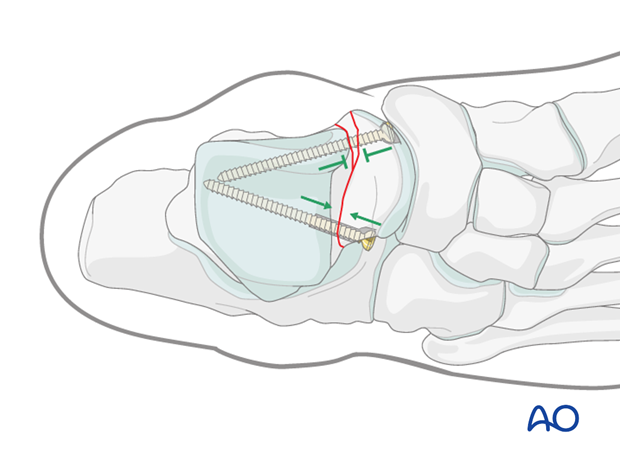
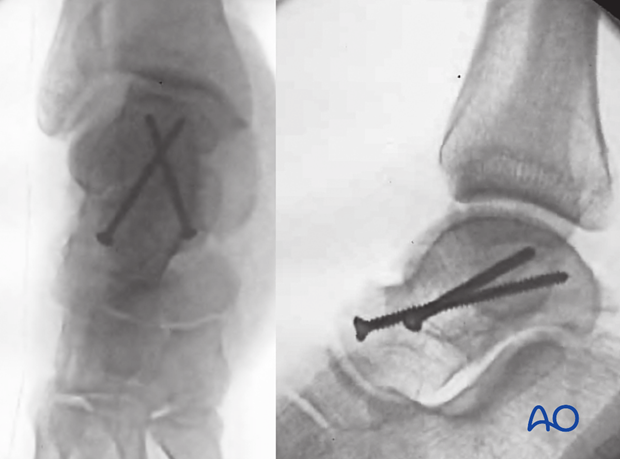
These screws do not need to be parallel because they each work through different means. The lateral screw provides compression while the medial screw acts simply as a position screw.
Completed fixation
Image intensification intraoperatively will ensure accurate reduction of all talar facets. The Canale views of the ankle and foot will demonstrate whether talar neck reduction and fixation has been achieved satisfactorily.
Stable fixation with this Hawkins type 2 fracture shows non-parallel screws. The lateral screw is in compression and the medial screw is a position screw.
In experienced hands, posterior to anterior screws are sometimes used.
6. Aftertreatment
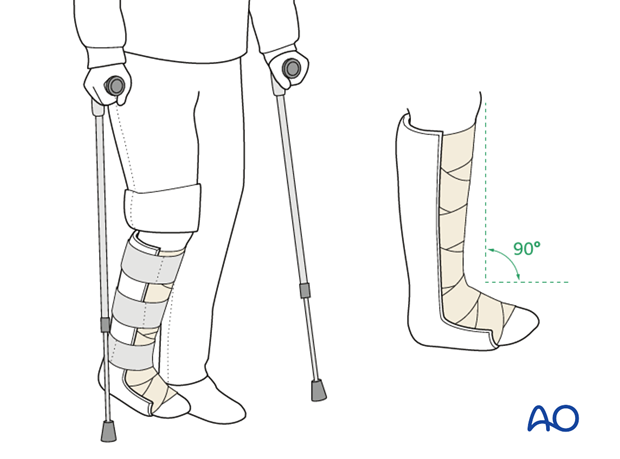
After surgery, a posterior splint with the foot in neutral position is applied. Early range of motion of the ankle and subtalar joint is advised.
Weight bearing should be restricted for 6 weeks. Follow-up visits with x-rays should be at 2 and 6 weeks.
Range-of-motion exercises are important to commence as soon as they are tolerated in order to restore a good range of motion.
Radiography at 6 weeks will confirm whether healing has occurred. Once bony union has been achieved, graduated weight-bearing can commence.
Patients with talar neck fractures should not begin weight bearing as long as there is pain at the fracture site.