Hemiarthroplasty
1. Principles
Key to successful arthroplasty
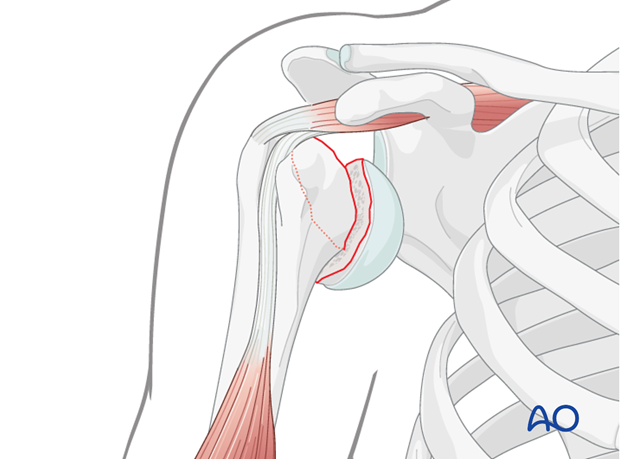
- Exposure of the shoulder joint. In these fractures, the tuberosities are not fractured and the humeral head is dislocated in isolation. Therefore, the approach to the glenohumeral joint is completely different. Depending on the surgeon’s preference, an osteotomy of the lesser tuberosity or a tenotomy of the subscapularis tendon may be used. However, an osteotomy of the lesser tuberosity is recommended.
- Correct determination of the surgical landmarks
- Proper determination of prosthesis size and position
Teaching video
AO teaching video: Shoulder arthroplasty
2. Patient preparation and approach
Patient preparation
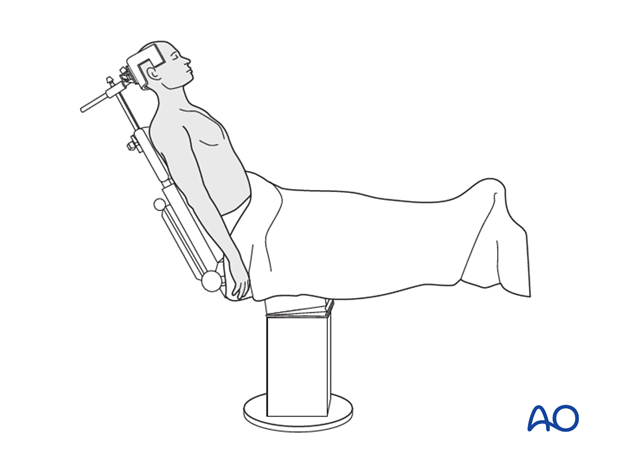
It is recommended to perform this procedure with the patient in a beach chair position.
Alternatively the patient may be positioned supine if the procedure is converted from ORIF.
Approach
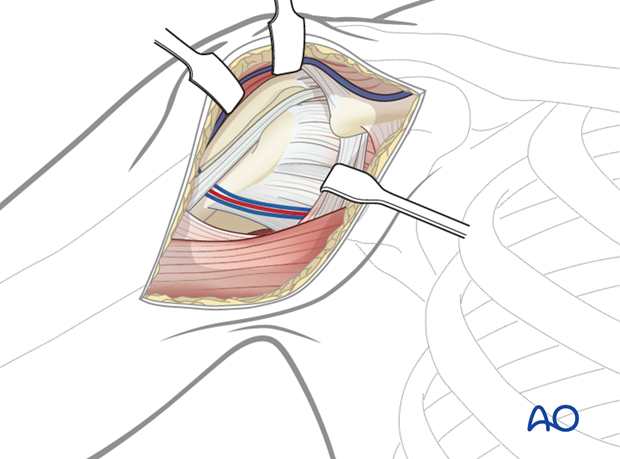
For this procedure the deltopectoral approach is normally used.
3. Treatment
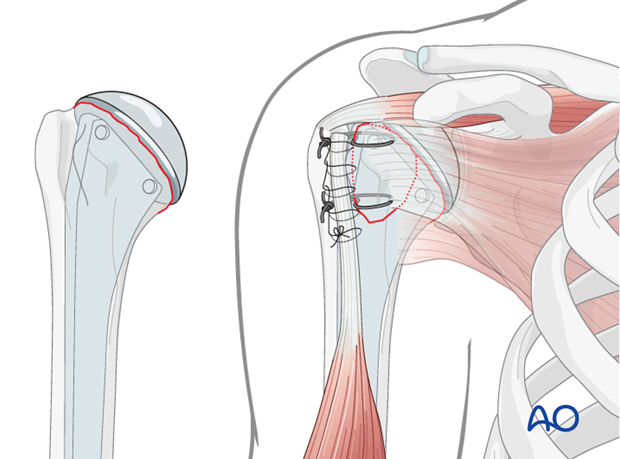
The implantation of a hemiarthroplasty in these fractures is comparable to hemiarthroplasty in degenerative arthrosis.
Key steps are:
- Retrieval of humeral head
- Measurement of humeral head size
- Exposure of proximal humerus in external rotation and adduction
- Exposure of most medial insertion line of supraspinatus tendon
- Rasping of humeral shaft
- Probe insertion
- Trimming of anatomic neck using oscillating saw and using probe as a template
- Defining final size and position of prosthetic humeral head
- Assembly of prosthesis according to individual parameters
- Insertion of definitive prosthesis
- Closure of osteotomy/tenotomy
These fractures are rare. Therefore, the surgical procedure of this treatment is not detailed here. Please refer to the manufacturer’s technique guide.
4. Rehabilitation
Overview of rehabilitation
The shoulder is perhaps the most challenging joint to rehabilitate both postoperatively and after conservative treatment. Early passive motion according to pain tolerance can usually be started after the first postoperative day - even following major reconstruction or prosthetic replacement. The program of rehabilitation has to be adjusted to the ability and expectations of the patient and the quality and stability of the repair. Poor purchase of screws in osteoporotic bone, concern about soft-tissue healing (eg tendons or ligaments) or other special conditions (eg percutaneous cannulated screw fixation without tension-absorbing sutures) may enforce delay in beginning passive motion, often performed by a physiotherapist.
The full exercise program progresses to protected active and then self-assisted exercises. The stretching and strengthening phases follow. The ultimate goal is to regain strength and full function.
Postoperative physiotherapy must be carefully supervised. Some surgeons choose to manage their patient’s rehabilitation without a separate therapist, but still recognize the importance of carefully instructing and monitoring their patient’s recovery.
Activities of daily living (ADL) can generally be resumed while avoiding certain stresses on the shoulder. Mild pain and some restriction of movement should not interfere with this. The more severe the initial displacement of a fracture, and the older the patient, the greater will be the likelihood of some residual loss of motion.
Progress of physiotherapy and callus formation should be monitored regularly. If weakness is greater than expected or fails to improve, the possibility of a nerve injury or a rotator cuff tear must be considered.
With regard to loss of motion, closed manipulation of the joint under anesthesia, may be indicated, once healing is sufficiently advanced. However, the danger of fixation loosening, or of a new fracture, especially in elderly patients, should be kept in mind. Arthroscopic lysis of adhesions or even open release and manipulation may be considered under certain circumstances, especially in younger individuals.
Special considerations for humeral head replacement
Following osteosynthesis of the tuberosities in combination with a hemiarthroplasty or a reverse shoulder arthroplasty rehabilitation must take into account the suture fixation of the tuberosities. It is recommended to place the arm in a neutral position on an abduction pillow for 6 weeks to ensure uneventful healing of the tuberosities. During this time, active assisted motion and therapy on a continuous passive motion (CPM) chair is helpful to prevent shoulder stiffness.
After removal of the abduction pillow, active motion over the horizontal plane is allowed and trained.
Shoulder rehabilitation protocol
Generally, shoulder rehabilitation protocols can be divided into three phases. Gentle range of motion can often begin early without stressing fixation or soft-tissue repair. Gentle assisted motion can frequently begin within a few weeks, the exact time and restriction depends on the injury and the patient. Resistance exercises to build strength and endurance should be delayed until bone and soft-tissue healing is secure. The schedule may need to be adjusted for each patient.
An example of a dedicated rehabilitation program for fractures in combination with reverse shoulder arthroplasty is shown below. This protocol addresses the fixed tuberosities which have to be protected for uneventful healing. This protocol can be modified according to the individual needs and expectations.
Phase 1 (approximately first 6 weeks)
Bandage
- Immobilization on a shoulder abduction pillow in neutral position of rotation
Range of motion
- Passive motion within the pain free interval for abduction, adduction and flexion
- No internal or external rotation
- No retroflexion
- Glenohumeral motion up to 90°
- ADL for eating and writing allowed
Physiotherapy
- Passive motion up to 90°
- Preservation and training of scapula mobility (manual therapy and proprioceptive neuromuscular facilitation stretching)
- Relaxation/stretching of neck muscles
- Training of elbow and hand functions
- Specific stabilization therapy for the glenohumeral joint
- Isometric exercises in all directions
- Treatment of scars after proper wound healing
- CPM up to 90° of abduction
Massage
- Neck
- Shoulder girdle
- Thoracic spine
Lymph drainage
- During hospitalization
Ice/warmth
- Ice/cold air for pain reduction
Training therapy
- Training of the contralateral arm (overflow cardiovascular training)
Phase 2 (approximately week 7-11)
Bandage
- No longer required
Range of motion
- Assisted/active motion within the pain free interval, also beyond 90°
- Careful rotation
Physiotherapy
- Free motion of shoulder girdle (scapula, clavicle, cervicothoracic junction, cervical and thoracic spine) with specific mobilization and decontraction techniques (manual therapy)
- Strengthening exercises especially for ADL
- Eccentric muscle activity
Massage
- As required
Lymph drainage
- As required
Ice/warmth
- As required
Training therapy
- Mobilization bath, wound permitting
- Training of hand and forearm muscles
- Set for shoulder therapy
- 3D movement pattern with pulling device
Phase 3 (after week 11)
Range of motion
- No restrictions on glenohumeral movement
- Muscle growth for shoulder girdle and all arm muscles
Physiotherapy
- All physiotherapeutic techniques allowed, active and against resistance
- Increasing eccentric muscle activity
Training therapy
- Handcycling
- Training for specific ADL and sports
- Machine training
- Free weight training













