ORIF - Plate fixation
1. Simple surgical neck with angulation: Principles
Reduction technique
For unimpacted surgical neck fractures generally, the most appropriate reduction technique will depend upon the fracture morphology.
Medial hinge intact:
- Fix plate to the humeral head and use it as reduction aid
- Reduce and fix the shaft to the plate
Proper reduction
After reduction, both, the sagittal and the coronal plane should be correct. Particular attention should be paid to the correct rotation.
Particularly with comminuted surgical neck fractures, remember that rotator cuff sutures can help reduce the humeral head against the plate to restore normal alignment.
Correct plate position
A correct plate position must be ensured in order to avoid loss of reduction and impingement.
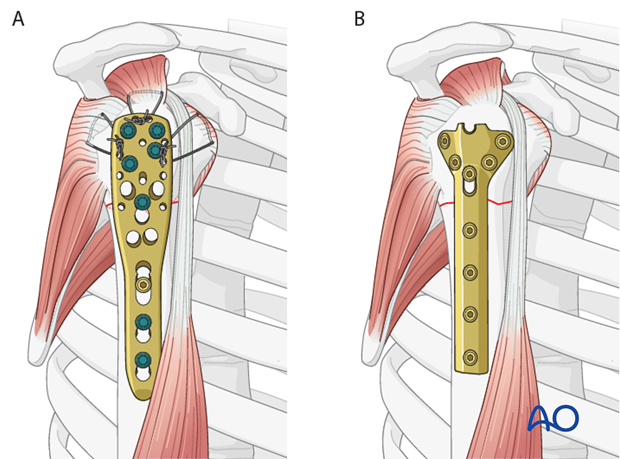
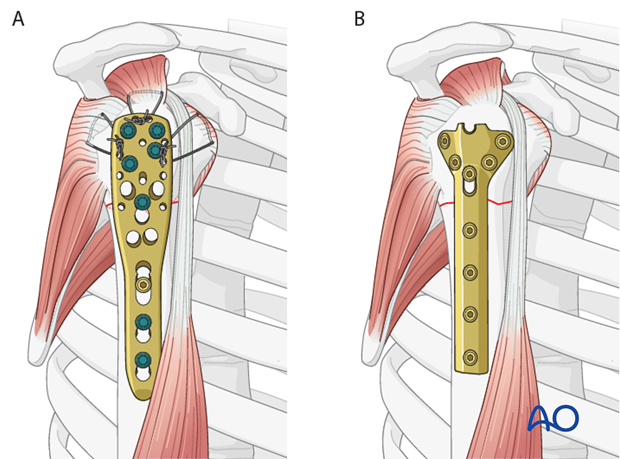
Angular stable versus standard plates
This procedure describes proximal humeral fracture fixation with an angular stable plate (A). Sometimes, these implants are not available. Standard plates provide an alternative option, for example the modified cloverleaf plate (B). Presently, the specific indications, advantages, and disadvantages of angular stable and standard plates are being clarified. There is some evidence that angular stable plates provide better outcomes. In addition to type and technique of fixation, the quality of reduction, the soft-tissue handling, and the characteristics of the injury and patient significantly influence the results. There is no evidence that the use of angular stable plates will overcome these other factors.
2. Patient preparation and approaches
Patient preparation
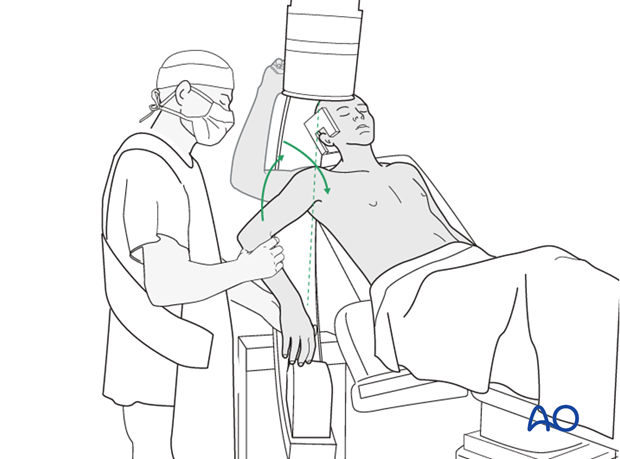
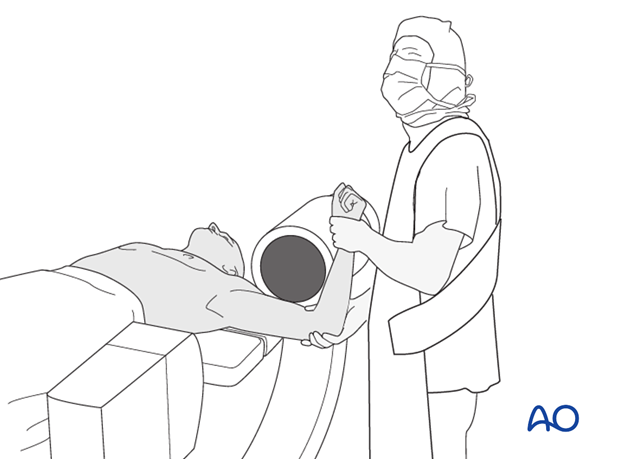
It is recommended to perform this procedure with the patient in a supine position (with the beach chair position as alternative).
Approaches
Choose whichever approach is best suited for anticipated reduction maneuvers:
The deltopectoral approach, while more extensile, is more invasive, but may provide easier access to a longer plate.
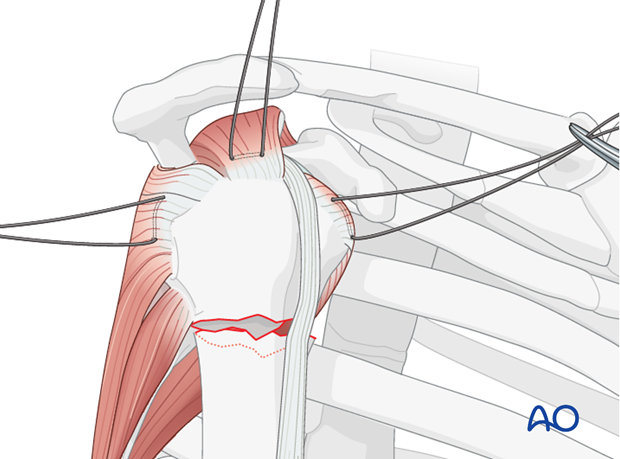
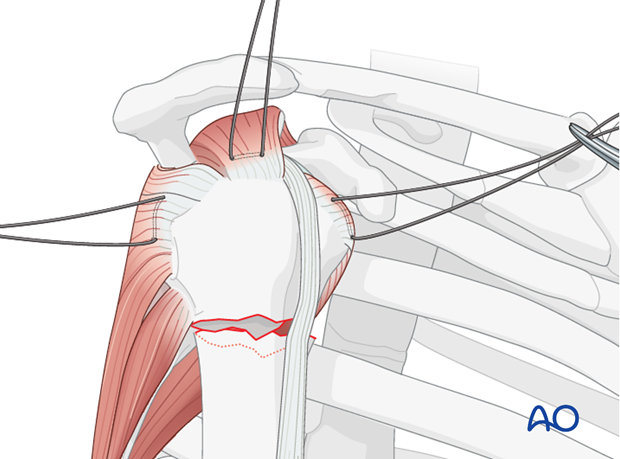
3. Simple surgical neck with angulation: Insert sutures
Insert holding sutures through the insertions of the subscapularis, supraspinatus, and infraspinatus tendon.
4. Simple surgical neck with angulation: Plate position
Correct plate position
The correct plate position is:
- about 5-8 mm distal to the top of the greater tuberosity
- aligned properly along the axis of the humeral shaft
- slightly posterior to the bicipital groove (2-4 mm)
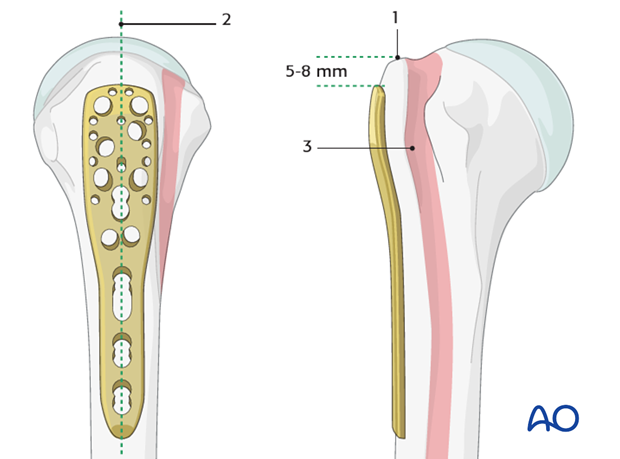
Confirmation of correct plate position
The correct plate position can be checked by palpation of its relationship to the bony structures and also confirmed by image intensification.
To confirm a correct axial plate position insert a K-wire through the proximal hole of the insertion guide. The K-wire should rest on the top of the humeral head.

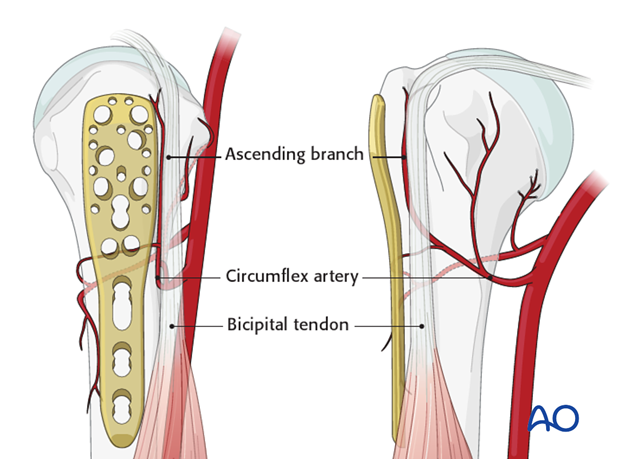
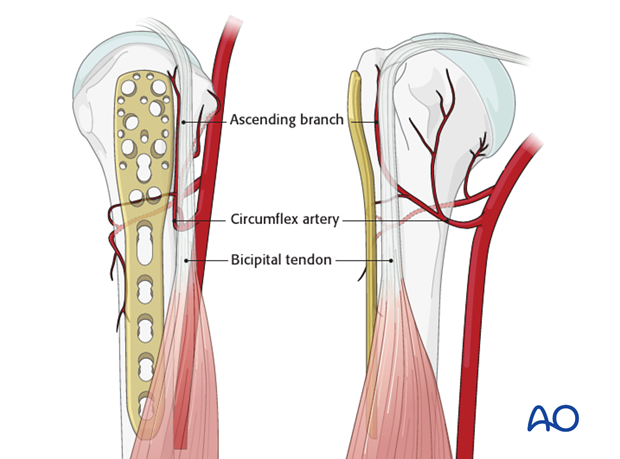
Pitfall 1: plate too close to the bicipital groove
The bicipital tendon and the ascending branch of the anterior humeral circumflex artery are at risk if the plate is positioned too close to the bicipital groove. (The illustration shows the plate in correct position, posterior to the bicipital groove).
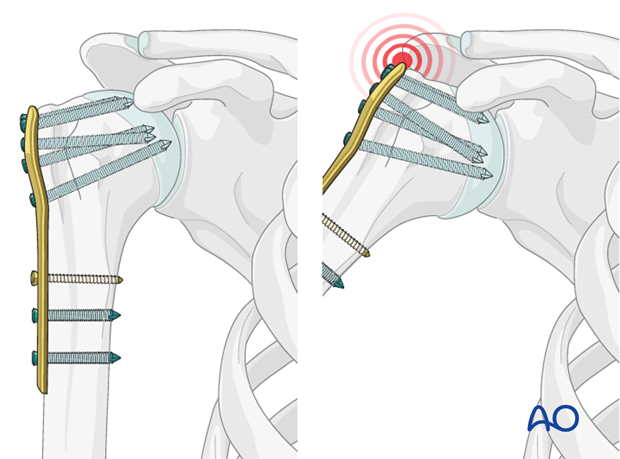
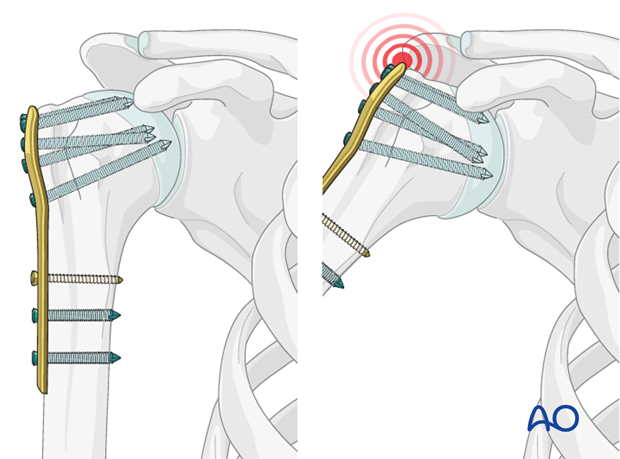
Pitfall 2: plate too proximal
A plate positioned too proximal carries two risks:
- The plate can impinge the acromion
- The most proximal screws might penetrate or fail to securely engage the humeral head
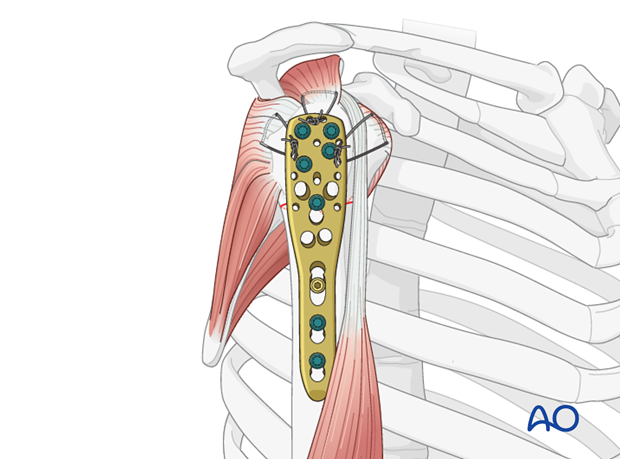
5. Simple surgical neck with angulation: Attaching the plate to the humeral head
The plate is fixed on the lateral side of the humeral head with locking-head screws.
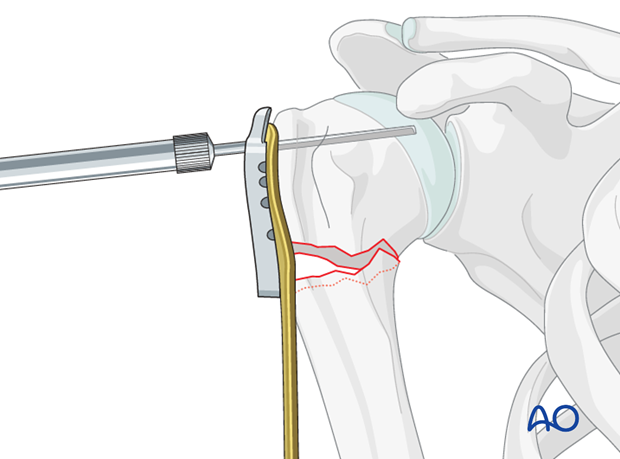
Drill holes
Use an appropriate sleeve to drill holes for the humeral head screws. Do not drill through the subchondral bone and into the shoulder joint.
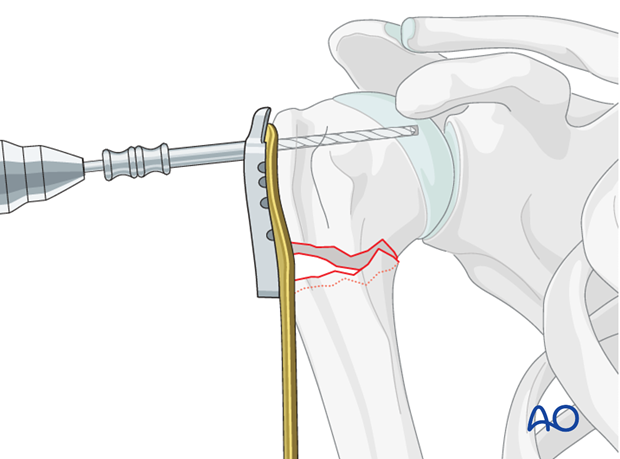
If the plate is properly positioned, the screws will be placed correctly in the humeral head. If there is any question about plate positioning (eg, very short proximal segment) confirm proper placement with two K-wires inserted through wire guides before inserting screws.
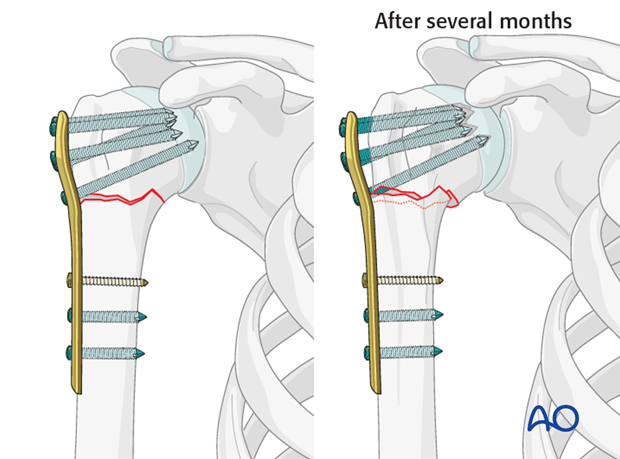
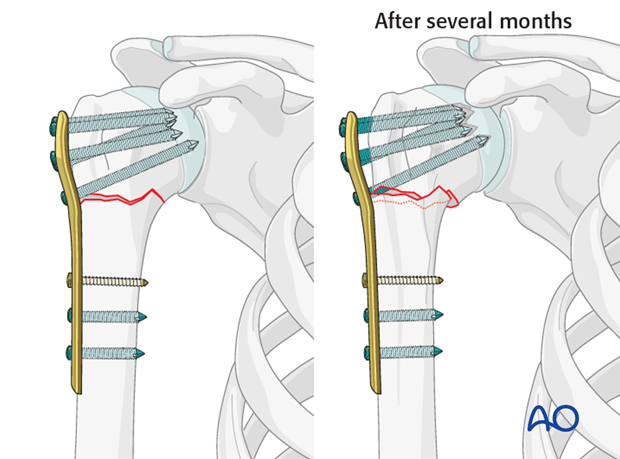
Avoiding intraarticular screw placement
Screws that penetrate the humeral head may significantly damage the glenoid cartilage. Primary penetration occurs when the screws are initially placed. Secondary penetration is the result of subsequent fracture collapse. Drilling into the joint increases the risk of screws becoming intraarticular.
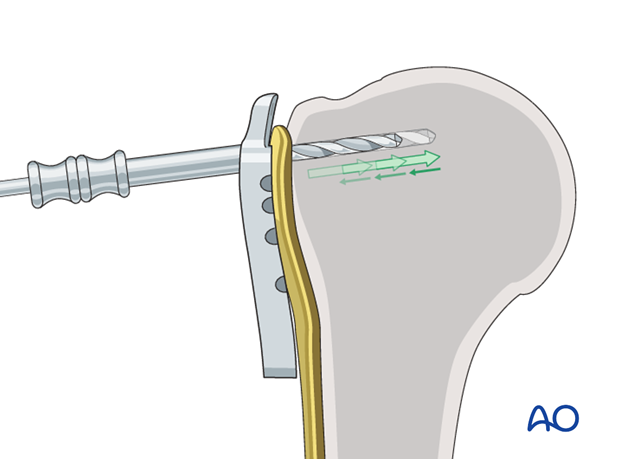
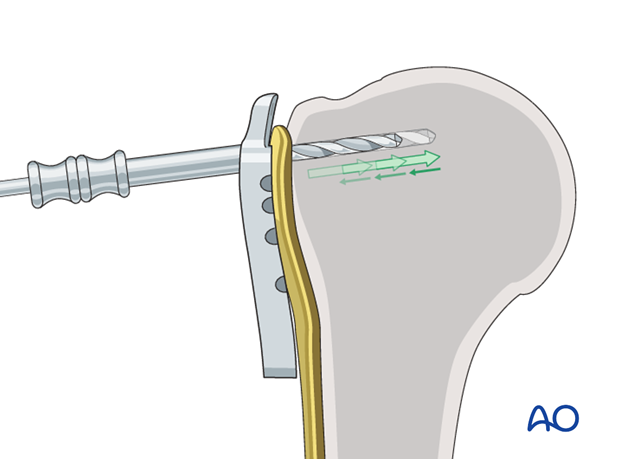
Two drilling techniques help to avoid drilling into the joint.
Pearl 1: “Woodpecker”-drilling technique (as illustrated)
In the woodpecker-drilling technique, advance the drill bit only for a short distance, then pull the drill back before advancing again. Keep repeating this procedure until subchondral bone contact can be felt. Take great care to avoid penetration of the humeral head.
Pearl 2: Drilling near cortex only
Particular in osteoporotic bone, one can drill only through the near cortex. Push the depth gauge through the remaining bone until subchondral resistance is felt.
Determine screw length
The intact subchondral bone should be felt with a depth gauge or blunt pin to ensure that the screw stays within the humeral head. The integrity of the subchondral bone can be confirmed by palpation or the sound of the instrument tapping against it. Typically, choose a screw slightly shorter than the measured length.
Insert screw
Insert a locking-head screw through the screw sleeve into the humeral head. The sleeve aims the screw correctly. Particularly in osteoporotic bone, a screw may not follow the hole that has been drilled.
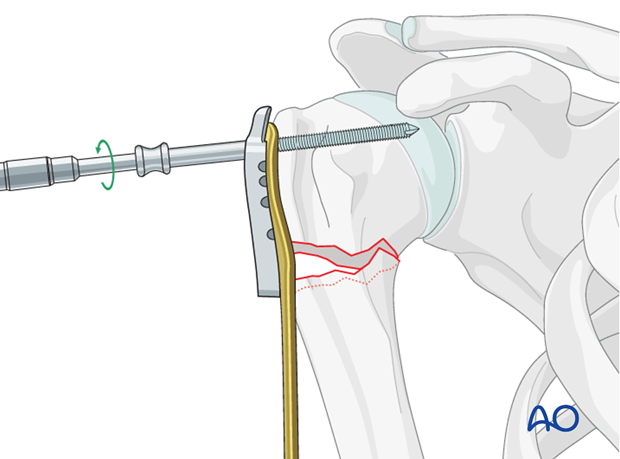
Number of screws and location
Place a sufficient number of screws into the humeral head. At this stage, only four screws are sufficient to fix the plate and allow for reduction using the plate. After reduction has been achieved, further screws might be inserted into the humeral head. Bone quality and fracture morphology should be considered. In osteoporotic bone a higher number of screws may be required.
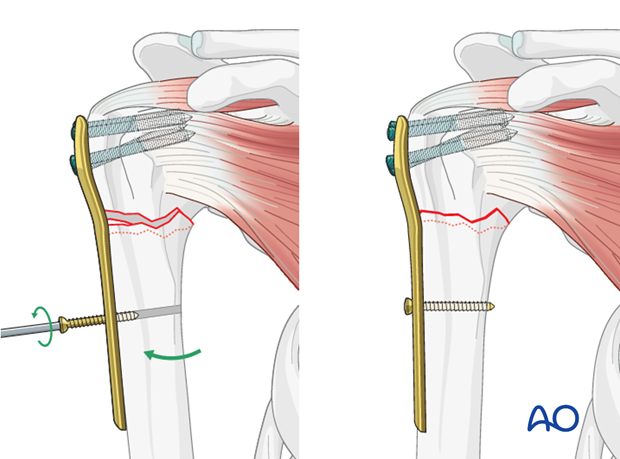
6. Simple surgical neck with angulation: Reduction and fixation of the plate to the humeral shaft
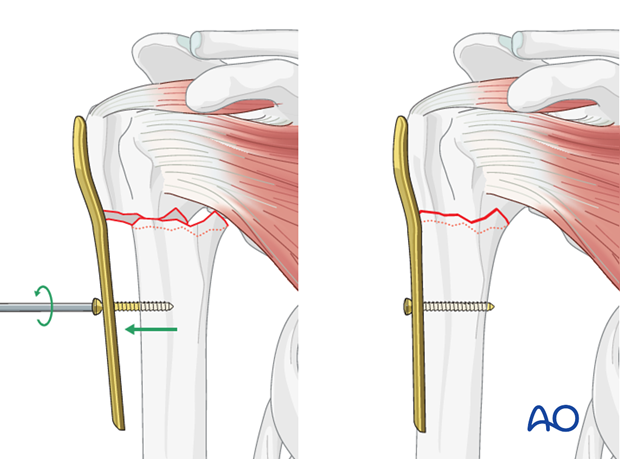
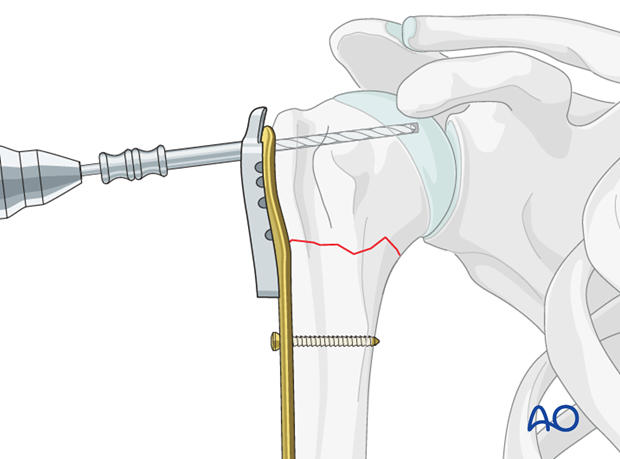
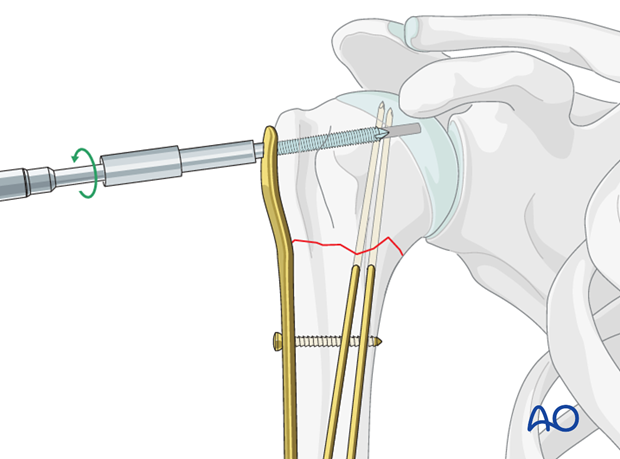
Use the plate as reduction aid
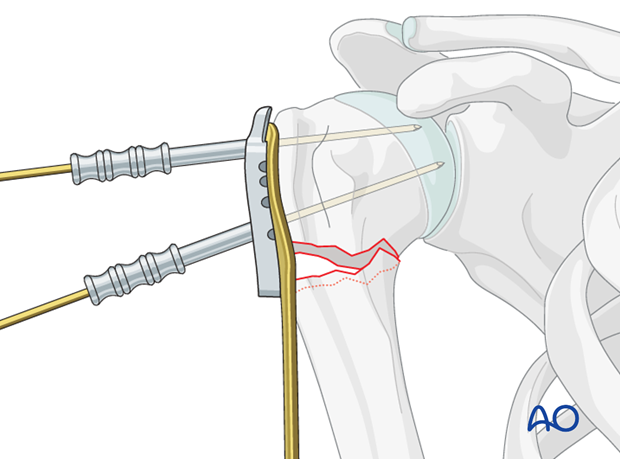
The plate is used as a handle to reduce the humeral head towards the shaft. It must be attached correctly to the humeral head before this is done. Provisional K-wire fixation using K-wire guides can help with this as demonstrated above.
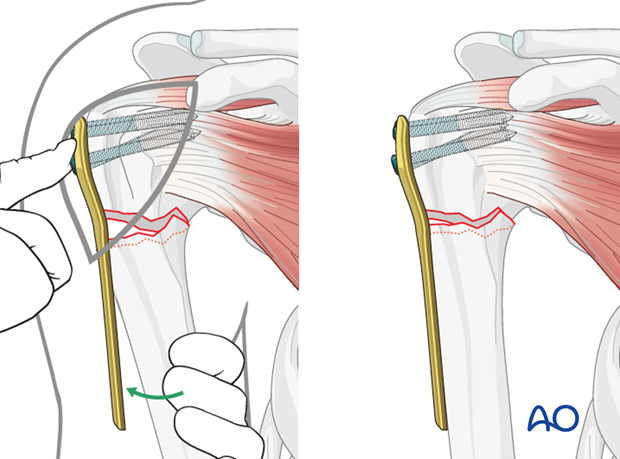
Once preliminary reduction is achieved a bicortical non-locking screw is inserted through the elongated hole. Make sure to insert the screw perpendicular to the humeral shaft.
By tightening this screw in the humeral shaft, the malpositioned humeral head will be aligned to the humeral shaft, thus achieving a correct reduction.
Option: preliminary fracture fixation with K-wires
As an alternative to reducing the fracture with a plate, an open reduction can be performed manually and temporarily secured using 2 K-wires. Make sure to place them from anterior in order to avoid interference with the foreseen plate position.
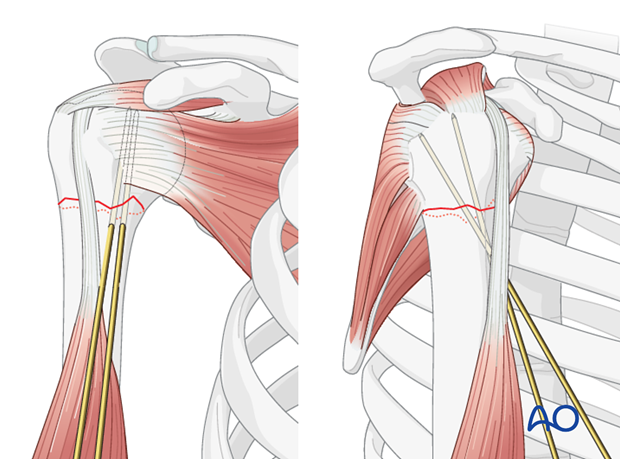
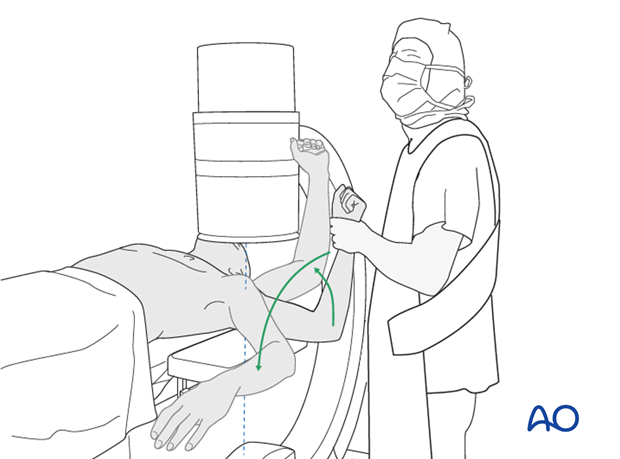
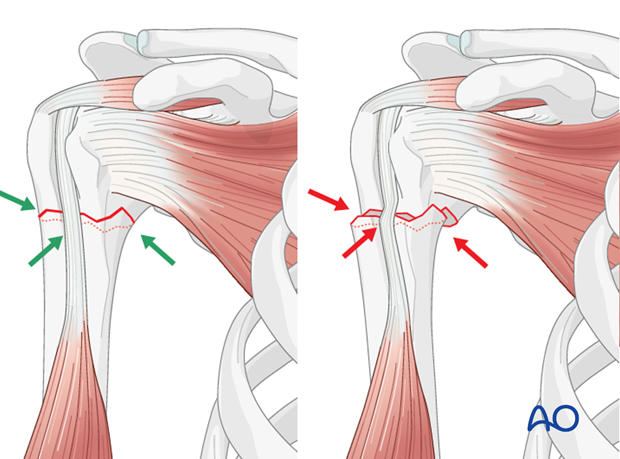
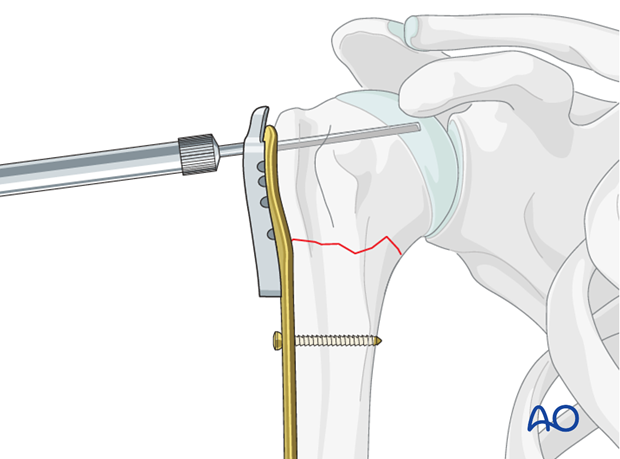
Confirm proper rotational alignment
Correct rotational alignment must be confirmed. This can be done by matching the fracture configurations on both sides of the fracture. This would be useful in the more transverse fracture configuration as shown in the illustration.
Pearl: check retroversion
The bicipital groove might be a good indicator for correct rotation. In case of correct rotation, no gap/angulation is visible at the level of the fracture.
Remember that the humeral head is normally retroverted, facing approximately 25° posteriorly (mean range: 18°-30°) relative to the distal humeral epicondylar axis. This axis is perpendicular to the forearm with the elbow flexed to 90°.
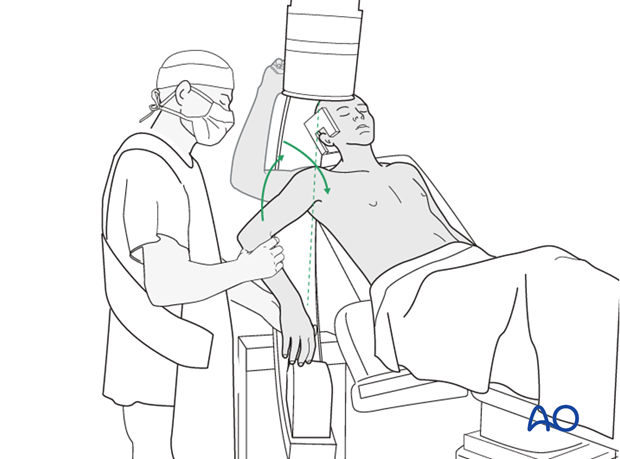
Confirmation of overall reduction
The correct reduction must be confirmed by image intensification in both AP and lateral views.
Insert additional screws
Insert one or two additional bicortical screws into the humeral shaft. Additional screws might also be inserted into the humeral head.
Supplementary rotator cuff tendon sutures
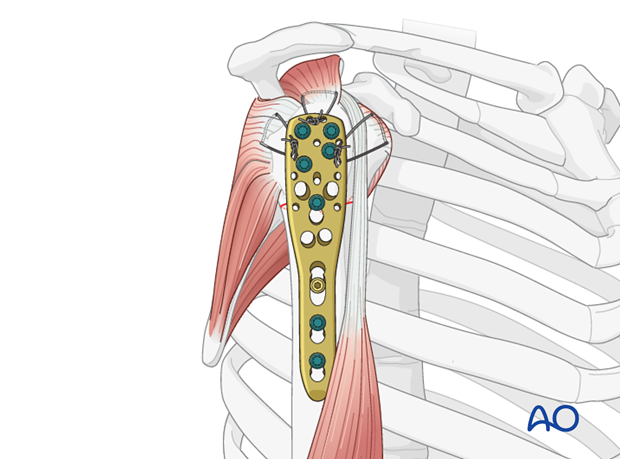
Secure the tendons of the rotator cuff (subscapularis, supraspinatus, infraspinatus) with additional neutralization sutures through the small holes in the plate.
This form of fixation was referred to as a “Tension band suture fixation”. We now prefer the term “Neutralization sutures” because the tension band mechanism cannot be applied consistently to each component of the fracture fixation. An explanation of the limits of the Tension band mechanism/principle can be found here.
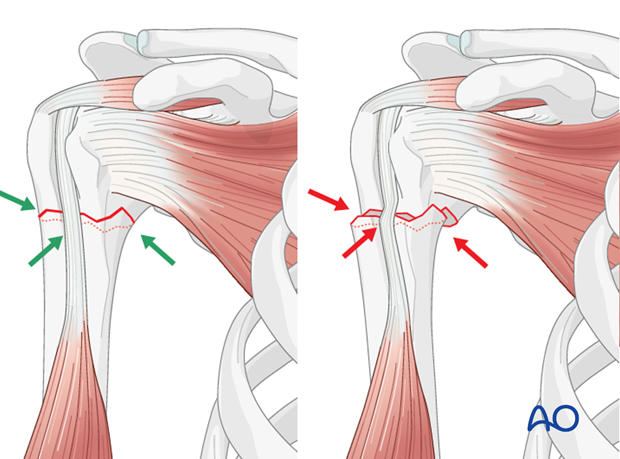
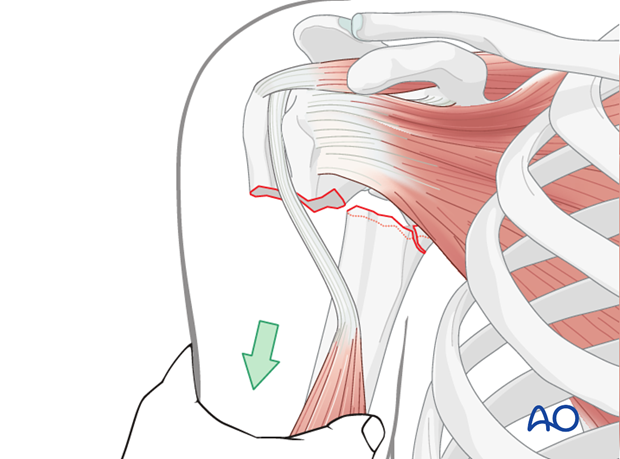
Pitfall: inadequate reduction
A common mistake is inadequate reduction. Residual varus malalignment often results in further (secondary) displacement with varus malunion or fixation failure and possible nonunion.
Final check of osteosynthesis
Using image intensification, carefully check for correct reduction and fixation (including proper implant position and length) at various arm positions. Ensure that screw tips are not intraarticular.
Also obtain an axial view.
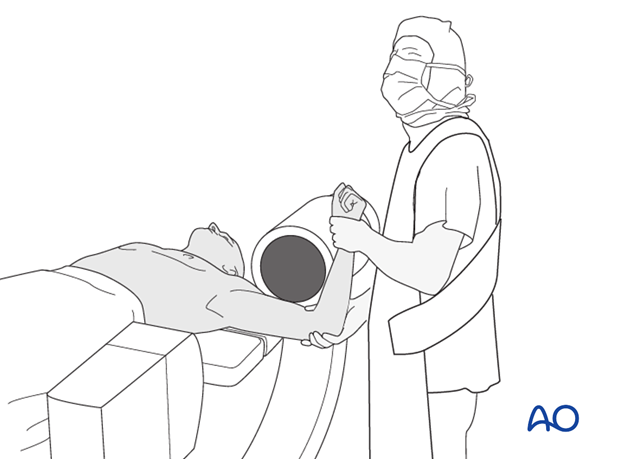
In the beach chair position, the C-arm must be directed appropriately for orthogonal views. Position arm as necessary to confirm that reduction is satisfactory, fixation is stable, and no screw is in the joint.
7. Surgical neck with translation or multifragmentary: Principles
Reduction technique
For unimpacted surgical neck fractures generally, the most appropriate reduction technique will depend upon the fracture morphology.
For fractures with medial hinge disruption or medial fragmentation, reduce a medially displaced fracture by pulling the humeral shaft to the plate by tightening an initial bicortical non-locking screw in the humeral shaft.
Proper reduction
Achieving proper reduction may be very demanding due to the characteristic metaphyseal instability of these fractures. Multifragmentary fractures may be reduced appropriately by using the laterally applied plate as a model for an appropriate reduction. The plate is first attached distally and then brought into contact with the fragmentary zone and proximal segment, to which it is affixed. Once initially stabilized, confirm satisfactory reduction before insertion of all the planned screws.
After reduction, both, the sagittal and the coronal plane should be correct. Particular attention should be paid to the correct rotation.
Particularly with comminuted surgical neck fractures, remember that rotator cuff sutures can help reduce the humeral head against the plate to restore normal alignment.
Correct plate position
A correct plate position must be ensured in order to avoid loss of reduction and impingement.
Angular stable versus standard plates
This procedure describes proximal humeral fracture fixation with an angular stable plate (A). Sometimes, these implants are not available. Standard plates provide an alternative option, for example the modified cloverleaf plate (B). Presently, the specific indications, advantages, and disadvantages of angular stable and standard plates are being clarified. There is some evidence that angular stable plate provide better outcomes. In addition to type and technique of fixation, the quality of reduction, the soft-tissue handling, and the characteristics of the injury and patient significantly influence the results. There is no evidence that the use of angular stable plates will overcome these other factors.
8. Surgical neck with translation or multifragmentary: Insert sutures
Insert holding sutures through the insertions of the subscapularis, supraspinatus, and infraspinatus tendon.
9. Surgical neck with translation or multifragmentary: Reduction and preliminary fixation
Reduction
Attempt to reduce these fractures with distal traction on the arm. In transverse fractures with translation, proper placement of the shaft against the proximal fragment may be stable. An oblique or fragmentary fracture is usually unstable.
Care should be taken to restore the medial calcar. To gain more stability slight impaction of the humeral shaft into the humeral head might be considered.
If there is medial fragmentation, special attention must be paid to prevent varus malalignment.
Use the plate as reduction aid
In these fractures, the fracture may be reduced with the help of the plate. This is most effective when the shaft is medially displaced or the fracture is in valgus malalignment. As illustrated, the plate is positioned on the lateral side of the humeral shaft. A single non-locking screw is placed perpendicularly into the shaft.
By tightening this screw, the humeral shaft will be pulled toward the plate. This maneuver “fine-tunes” the reduction.
Confirm proper rotational alignment
Correct rotational alignment must be confirmed. This can be done by matching the fracture configurations on both sides of the fracture. This would be useful in the more transverse fracture configuration as shown in the illustration.
Pearl: check retroversion
The bicipital groove might be a good indicator for correct rotation. In case of correct rotation, no gap/angulation is visible at the level of the fracture.
Remember that the humeral head is normally retroverted, facing approximately 25° posteriorly (mean range: 18°-30°) relative to the distal humeral epicondylar axis. This axis is perpendicular to the forearm with the elbow flexed to 90°.
Confirmation of overall reduction
The correct reduction must be confirmed by image intensification in both AP and lateral views.
10. Surgical neck with translation or multifragmentary: Plate position
Correct plate position
The correct plate position is:
- about 5-8 mm distal to the top of the greater tuberosity
- aligned properly along the axis of the humeral shaft
- slightly posterior to the bicipital groove (2-4 mm)
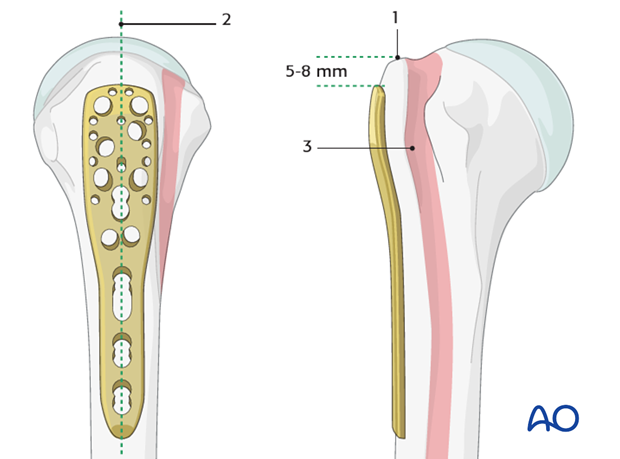
Confirmation of correct plate position
The correct plate position can be checked by palpation of its relationship to the bony structures and also confirmed by image intensification.
To confirm a correct axial plate position insert a K-wire through the proximal hole of the insertion guide. The K-wire should rest on the top of the humeral head.

Pitfall 1: plate too close to the bicipital groove
The bicipital tendon and the ascending branch of the anterior humeral circumflex artery are at risk if the plate is positioned too close to the bicipital groove. (The illustration shows the plate in correct position, posterior to the bicipital groove).
Pitfall 2: plate too proximal
A plate positioned too proximal carries two risks:
- The plate can impinge the acromion
- The most proximal screws might penetrate or fail to securely engage the humeral head
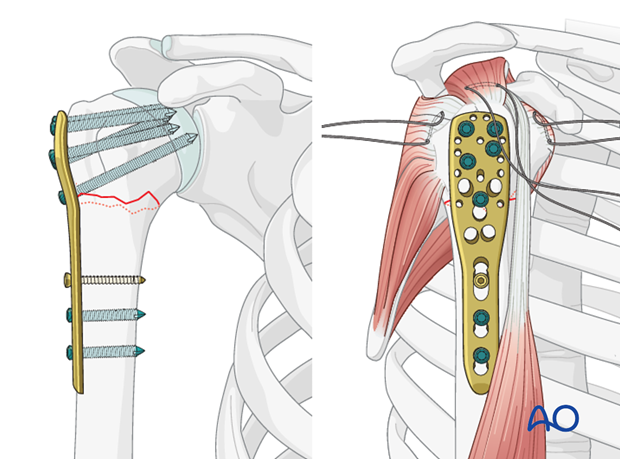
11. Surgical neck with translation or multifragmentary: Plate fixation
Fix plate to the humeral head
Drill holes
Use an appropriate sleeve to drill holes for the humeral head screws. Do not drill through the subchondral bone and into the shoulder joint.
Avoiding intraarticular screw placement
Screws that penetrate the humeral head may significantly damage the glenoid cartilage. Primary penetration occurs when the screws are initially placed. Secondary penetration is the result of subsequent fracture collapse. Drilling into the joint increases the risk of screws becoming intraarticular.
Two drilling techniques help to avoid drilling into the joint.
Pearl 1: “Woodpecker”-drilling technique (as illustrated)
In the woodpecker-drilling technique, advance the drill bit only for a short distance, then pull the drill back before advancing again. Keep repeating this procedure until subchondral bone contact can be felt. Take great care to avoid penetration of the humeral head.
Pearl 2: Drilling near cortex only
Particular in osteoporotic bone, one can drill only through the near cortex. Push the depth gauge through the remaining bone until subchondral resistance is felt.
Determine screw length
The intact subchondral bone should be felt with a depth gauge or blunt pin to ensure that the screw stays within the humeral head. The integrity of the subchondral bone can be confirmed by palpation or the sound of the instrument tapping against it. Typically, choose a screw slightly shorter than the measured length.
Insert screw
Insert a locking-head screw through the screw sleeve into the humeral head. The sleeve aims the screw correctly. Particularly in osteoporotic bone, a screw may not follow the hole that has been drilled.
Number of screws and location
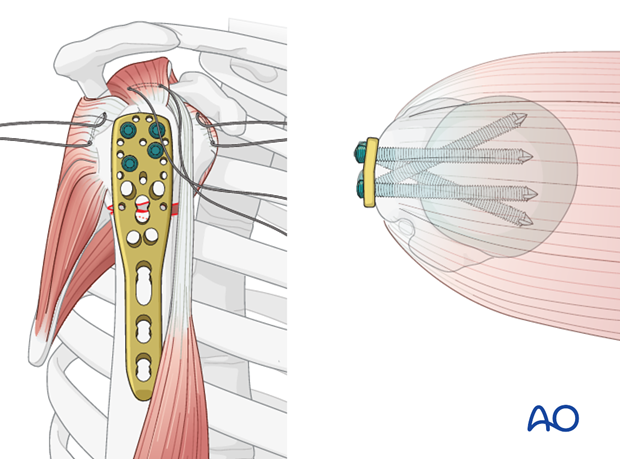
Place a sufficient number of screws (often 5) into the humeral head. The optimal number and location of screws has not been determined. Bone quality and fracture morphology should be considered. In osteoporotic bone a higher number of screws may be required.
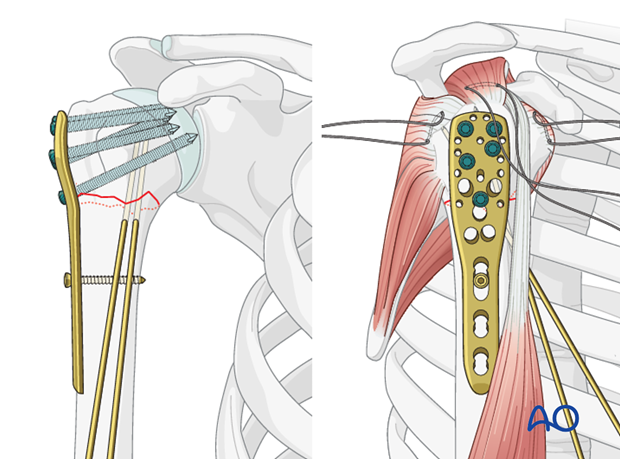
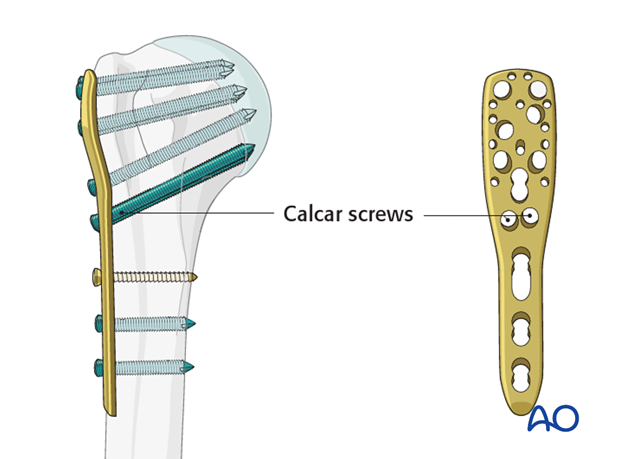
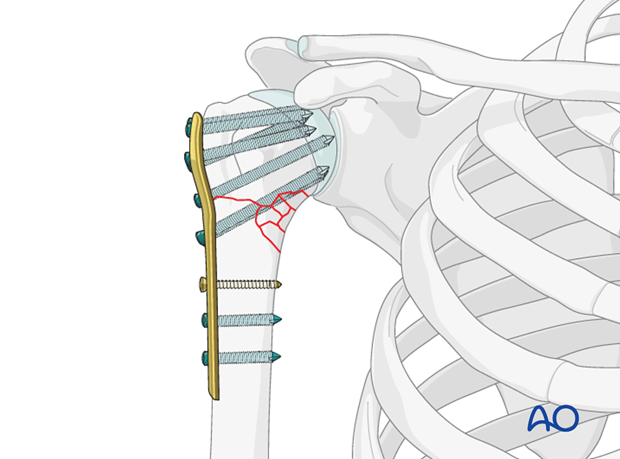
Calcar screws
It is strongly recommended to use “calcar screws” in all varus displaced fractures, especially, if there is medial fragmentation. Their purchase in the inferomedial humeral head adds mechanical stability.
Insert additional screws into the humeral shaft
Insert one or two additional bicortical screws into the humeral shaft.
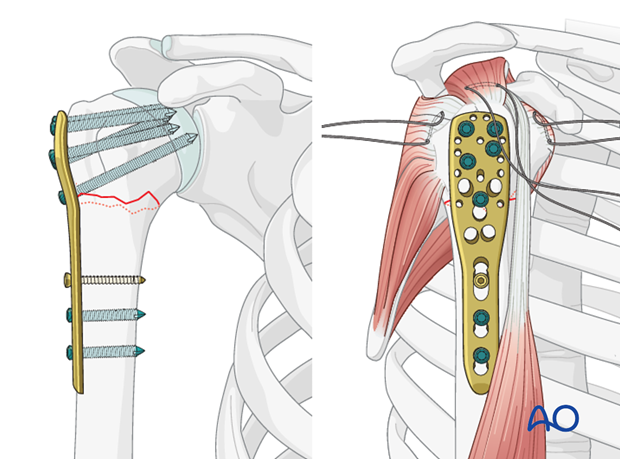
Supplementary rotator cuff tendon sutures
Secure the tendons of the rotator cuff (subscapularis, supraspinatus, infraspinatus) with additional neutralization sutures through the small holes in the plate.
This form of fixation was referred to as a “Tension band suture fixation”. We now prefer the term “Neutralization sutures” because the tension band mechanism cannot be applied consistently to each component of the fracture fixation. An explanation of the limits of the Tension band mechanism/principle can be found here.
Pitfall: inadequate reduction
A common mistake is inadequate reduction. Residual varus malalignment often results in further (secondary) displacement with varus malunion or fixation failure and possible nonunion.
Completed osteosynthesis
This illustration shows the completed osteosynthesis for a medially fragmentary fracture using calcar screws.
Final check of osteosynthesis
Using image intensification, carefully check for correct reduction and fixation (including proper implant position and length) at various arm positions. Ensure that screw tips are not intraarticular.
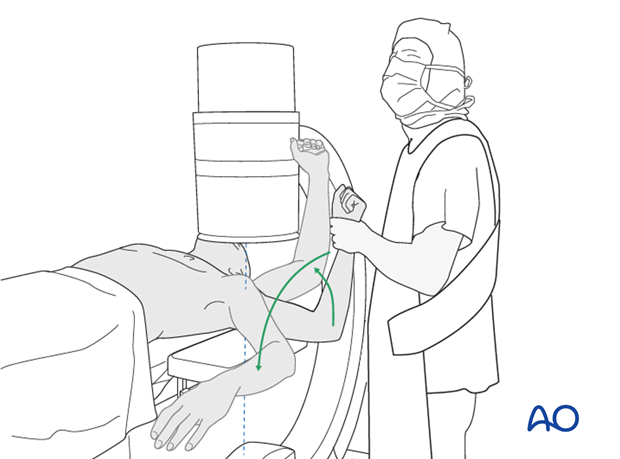
Also obtain an axial view.
In the beach chair position, the C-arm must be directed appropriately for orthogonal views.
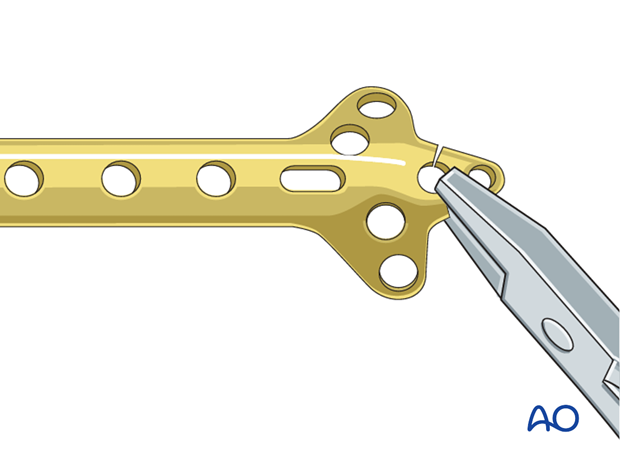
12. Use of standard plates
If no angular stable plate is available, a standard plate provides an alternative. The described procedure (reduction, preliminary fixation, and rotator cuff sutures) is essentially the same for standard plates, except for the screws. A good choice from the standard plates is the small fragment cloverleaf plate, with its tip cut off, and contoured as necessary. This plate allows multiple small fragment screws for the humeral head.
Be aware that angular stable implants provide better fixation, especially in osteoporotic bone. On the other hand, even angular stable plates are not a substitute for good surgical technique and judgment. Advances in fracture classification, understanding of the blood supply, use of rotator cuff tendon sutures, anatomical fracture reduction, and provisional fixation, represent improvements in care. When combined with optimal implants, these contributions offer the best chance of a good outcome.
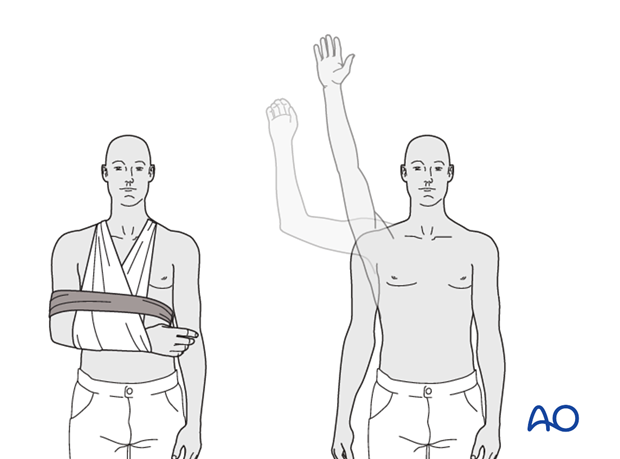
13. Overview of rehabilitation
The shoulder is perhaps the most challenging joint to rehabilitate both postoperatively and after conservative treatment. Early passive motion according to pain tolerance can usually be started after the first postoperative day - even following major reconstruction or prosthetic replacement. The program of rehabilitation has to be adjusted to the ability and expectations of the patient and the quality and stability of the repair. Poor purchase of screws in osteoporotic bone, concern about soft-tissue healing (eg tendons or ligaments) or other special conditions (eg percutaneous cannulated screw fixation without tension-absorbing sutures) may enforce delay in beginning passive motion, often performed by a physiotherapist.
The full exercise program progresses to protected active and then self-assisted exercises. The stretching and strengthening phases follow. The ultimate goal is to regain strength and full function.
Postoperative physiotherapy must be carefully supervised. Some surgeons choose to manage their patient’s rehabilitation without a separate therapist, but still recognize the importance of carefully instructing and monitoring their patient’s recovery.
Activities of daily living can generally be resumed while avoiding certain stresses on the shoulder. Mild pain and some restriction of movement should not interfere with this. The more severe the initial displacement of a fracture, and the older the patient, the greater will be the likelihood of some residual loss of motion.
Progress of physiotherapy and callus formation should be monitored regularly. If weakness is greater than expected or fails to improve, the possibility of a nerve injury or a rotator cuff tear must be considered.
With regard to loss of motion, closed manipulation of the joint under anesthesia, may be indicated, once healing is sufficiently advanced. However, the danger of fixation loosening, or of a new fracture, especially in elderly patients, should be kept in mind. Arthroscopic lysis of adhesions or even open release and manipulation may be considered under certain circumstances, especially in younger individuals.
Progressive exercises
Mechanical support should be provided until the patient is sufficiently comfortable to begin shoulder use, and/or the fracture is sufficiently consolidated that displacement is unlikely.
Once these goals have been achieved, rehabilitative exercises can begin to restore range of motion, strength, and function.
The three phases of nonoperative treatment are thus:
- Immobilization
- Passive/assisted range of motion
- Progressive resistance exercises
Immobilization should be maintained as short as possible and as long as necessary. Usually, immobilization is recommended for 2-3 weeks, followed by gentle range of motion exercises. Resistance exercises can generally be started at 6 weeks. Isometric exercises may begin earlier, depending upon the injury and its repair. If greater or lesser tuberosity fractures have been repaired, it is important not to stress the rotator cuff muscles until the tendon insertions are securely healed.
Special considerations
Glenohumeral dislocation: Use of a sling or sling-and-swath device, at least intermittently, is more comfortable for patients who have had an associated glenohumeral dislocation. Particularly during sleep, this may help avoid a redislocation.
Weight bearing: Neither weight bearing nor heavy lifting are recommended for the injured limb until healing is secure.
Implant removal: Implant removal is generally not necessary unless loosening or impingement occurs. Implant removal can be combined with a shoulder arthrolysis, if necessary.
Shoulder rehabilitation protocol
Generally, shoulder rehabilitation protocols can be divided into three phases. Gentle range of motion can often begin early without stressing fixation or soft-tissue repair. Gentle assisted motion can frequently begin within a few weeks, the exact time and restriction depends on the injury and the patient. Resistance exercises to build strength and endurance should be delayed until bone and soft-tissue healing is secure. The schedule may need to be adjusted for each patient.
Phase 1 (approximately first 3 weeks)
- Immobilization and/or support for 2-3 weeks
- Pendulum exercises
- Gently assisted motion
- Avoid external rotation for first 6 weeks
Phase 2 (approximately weeks 3-9)
If there is clinical evidence of healing and fragments move as a unit, and no displacement is visible on the x-ray, then:
- Active-assisted forward flexion and abduction
- Gentle functional use week 3-6 (no abduction against resistance)
- Gradually reduce assistance during motion from week 6 on
Phase 3 (approximately after week 9)
- Add isotonic, concentric, and eccentric strengthening exercises
- If there is bone healing but joint stiffness, then add passive stretching by physiotherapist













