ORIF - Pubic ramus plate
1. Introduction
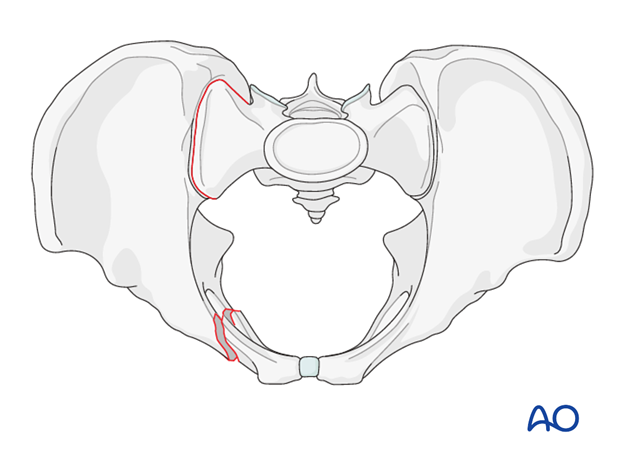
Fractures of the pubic rami are nearly always associated with further pelvic ring injuries. The treatment of these fractures is guided by the displacement and other associated pelvic ring injuries.
In many cases, a strong periosteum, the inguinal ligament and the pectineal ligament will provide adequate stability and no additional treatment is required. With more complex, unstable pelvic ring injuries, ramus fractures may require fixation to restore stability and promote healing.
The decision for operative vs. nonoperative is best made by evaluating the entire pelvic ring and its stability instead of focusing only on the ramus fracture.
For more complex injuries, posterior reduction and fixation must precede fixation of the ramus fractures. In these cases, the anterior fixation supplements and stabilizes the posterior fixation.
Options for fixation
Stabilization of ramus fractures can be performed by a variety of techniques:
- Internal fixation with an intramedullary screw
- Internal fixation with a plate
- Indirect stabilization with external fixation
For plate fixation, open anatomic reduction is desired. Typically, 3.5 mm reconstruction plates are utilized. Alternatively, any appropriate pelvic plate can also be used.
In osteoporotic bone and in comminuted fractures, angular stable plates are preferred.
The decision to use this technique is based on the pelvic injury pattern, nature of the ramus fractures, and the surgeon's comfort with the anatomy and imaging.
2. Patient preparation and approach
Patient preparation
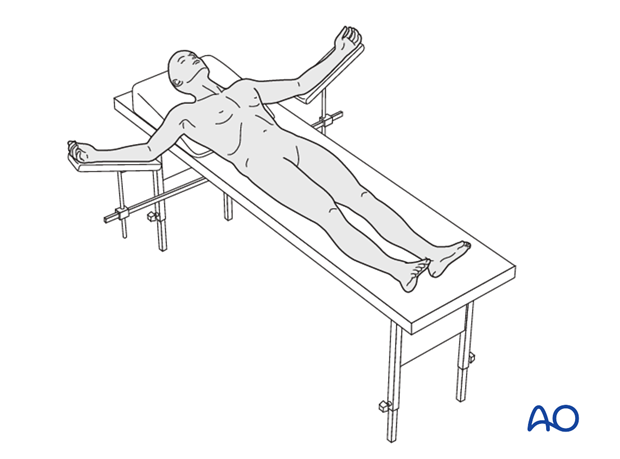
This procedure is performed with the patient in a supine position.
Approaches
For this procedure either an approach to the pubic symphysis or a modified stoppa approach is used.
3. Open reduction
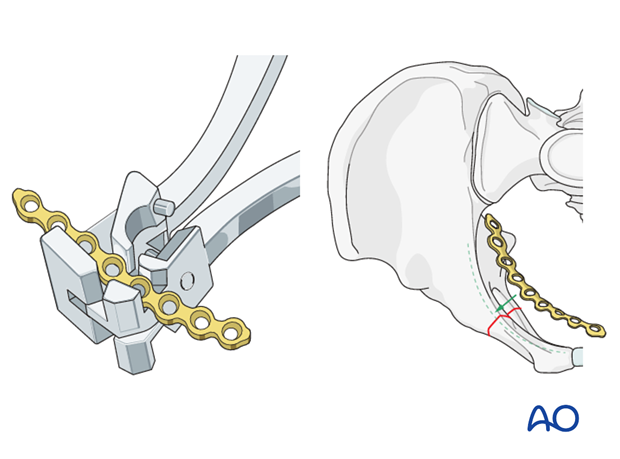
After adequate exposure of the fracture site is gained through an anterior approach, bone holding forceps are used to reduce the fracture by direct manipulation.
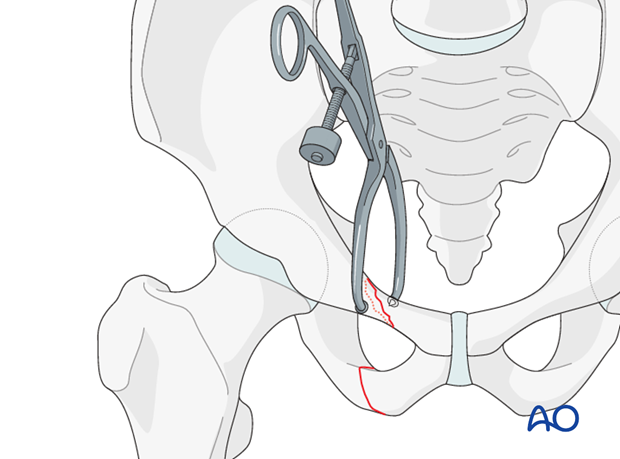
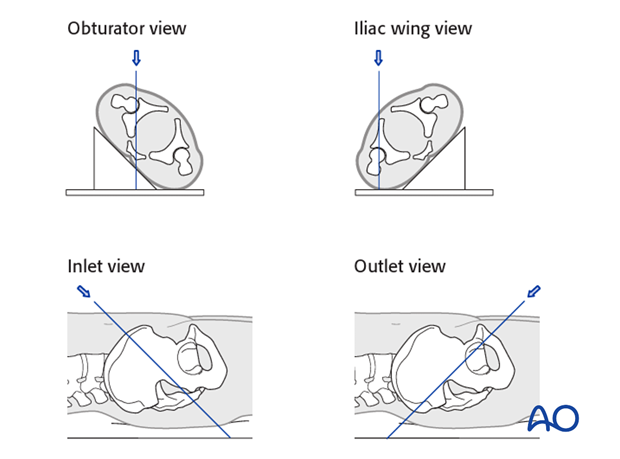
Reduction is verified by direct vision as well as with image intensifier using inlet and outlet views.
If anatomic reduction is not possible in comminuted fractures, a bridging technique with an appropriately contoured plate is used.
Note
Be alert for rotational malalignment of the fracture. This can be corrected by derotation by bone holding forceps.
4. Fixation
Fixation of oblique fractures
When anatomic reduction is achieved, K-wires are inserted perpendicular to the fracture plane to fix the fracture temporarily.
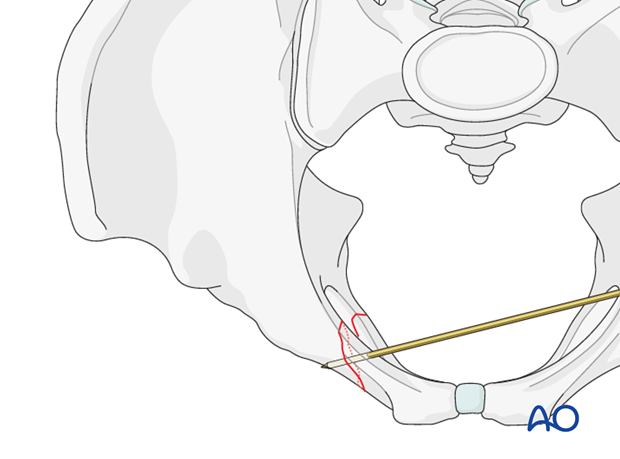
Insert the lag screw as perpendicular as possible to the fracture line.
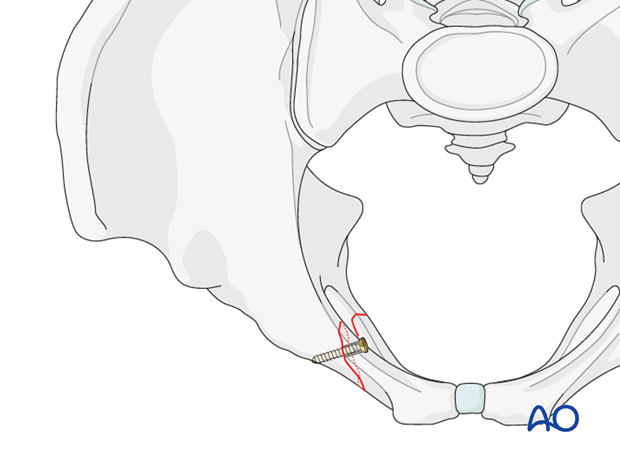
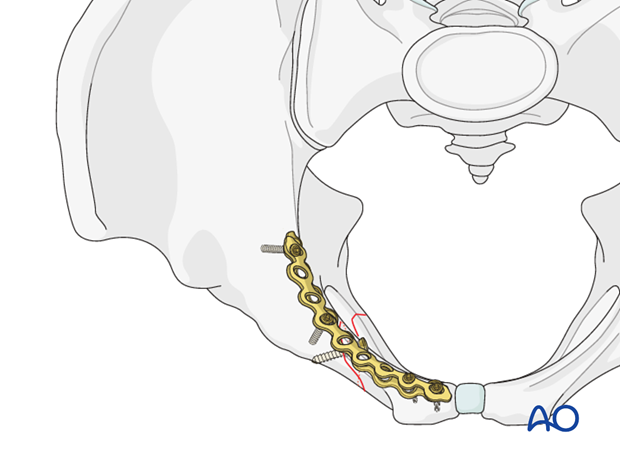
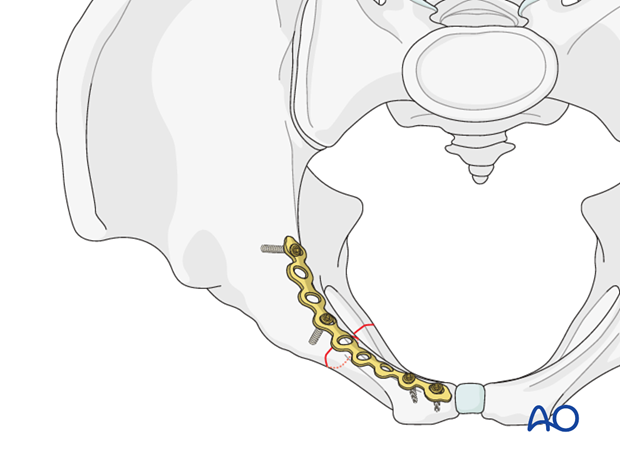
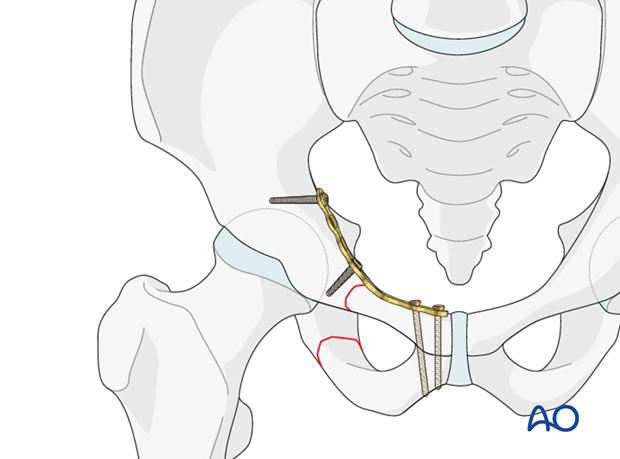
Place an appropriately contoured neutralization plate on the superomedial surface of the superior pubic ramus and fix it.
Fixation of transverse fractures
If the reduced fracture is stable, it will provide a template for appropriate contouring of the plate.
Remember to achieve compression of the transverse fracture by slightly underbending the plate which is being applied to a concave surface.
The plate is placed superomedial on the superior pubic ramus and inserted in compression mode.
Fixation of comminuted fractures
In comminuted fractures it is important to evaluate the overall geometry of the pelvis.
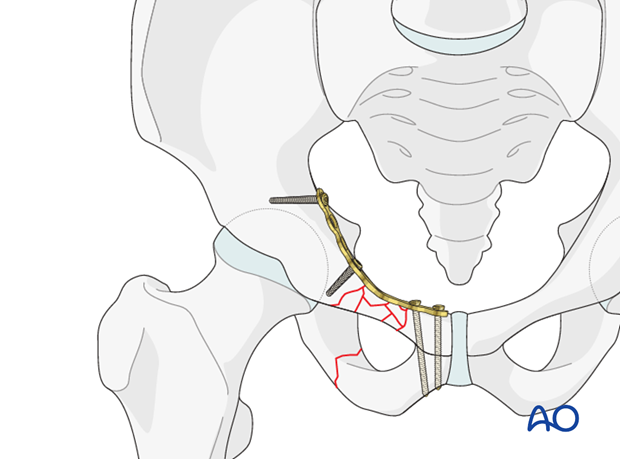
When acceptable reduction of the pubic rami is achieved, an appropriately contoured plate is inserted as a bridging plate, superomedially on the superior pubic ramus.
Comment to medial and lateral fractures
In medial fractures, it is possible to fix the plate to the ramus alone, both medially and laterally. At least two screws should be inserted on each side of the fracture line.
Extension of the plate across the symphysis to gain additional screws is possible if fixation is poor.
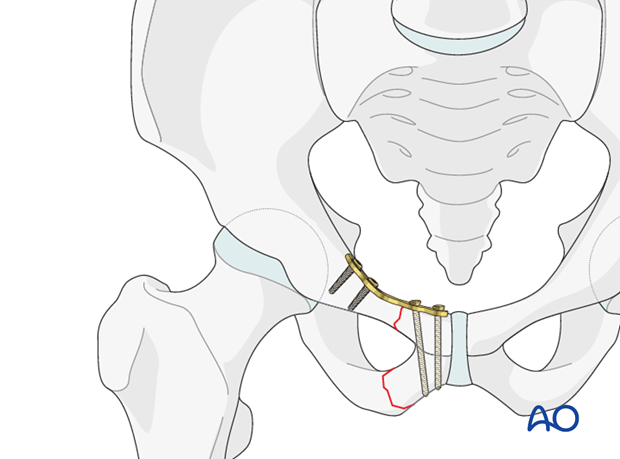
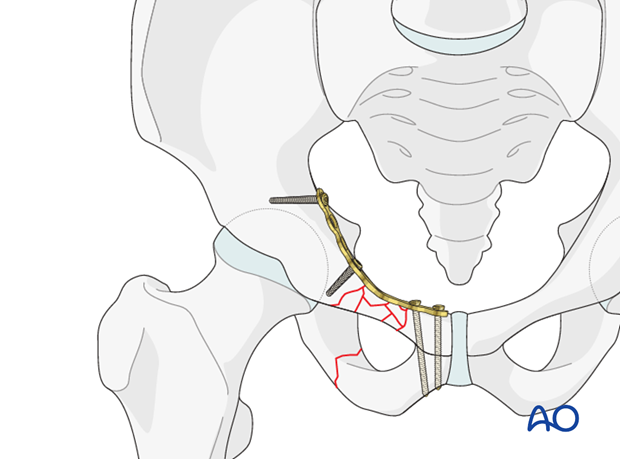
In lateral fracture patterns of the superior ramus, the lateral end of the plate should be fixed posterior to the acetabulum, as illustrated.
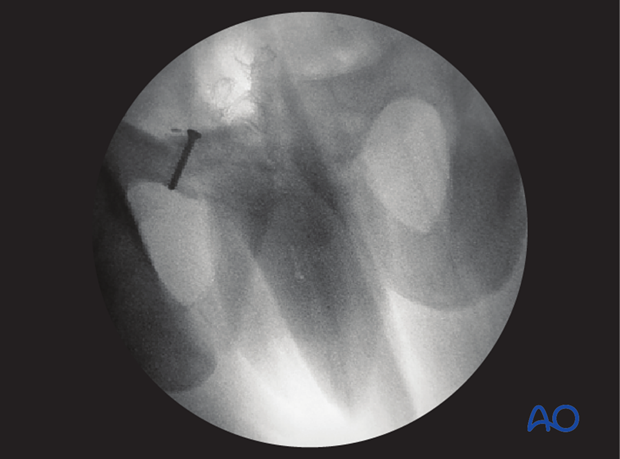
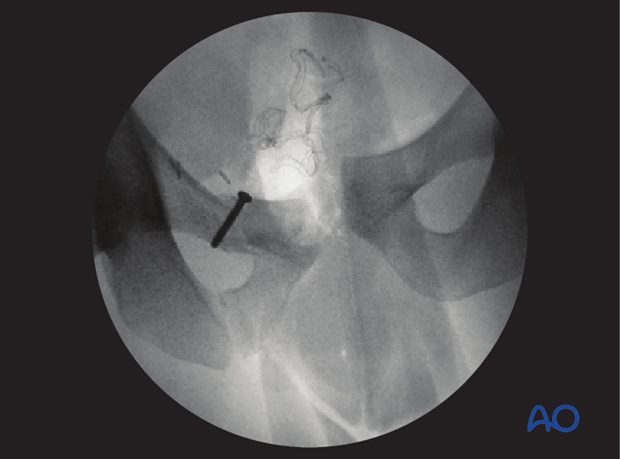
Verification of screw position
The position of each screw should be verified by C-arm to prevent screw penetration into the symphysis or the acetabulum.
Lateral screw positions are verified in the obturator and the iliac wing view.
The medial screws are verified using inlet and outlet views.
X-rays
After completion of internal fixation, confirm the final reduction and hardware position intraoperatively by AP, inlet and outlet radiographic imaging.

5. Aftercare following open reduction and fixation
Postoperative blood test
After pelvic surgery, routine hemoglobin and electrolyte check out should be performed the first day after surgery and corrected if necessary.
Bowel function and food
After extensile approaches in the anterior pelvis, the bowel function may be temporarily compromised. This temporary paralytic ileus generally does not need specific treatment beyond withholding food and drink until bowel function recovers.
Analgesics
Adequate analgesia is important. Non pharmacologic pain management should be considered as well (eg. local cooling and psychological support).
Anticoagulation
Prophylaxis for deep vein thrombosis (DVT) and pulmonary embolus is routine unless contraindicated. The optimal duration of DVT prophylaxis in this setting remains unproven, but in general it should be continued until the patient can actively walk (typically 4-6 weeks).
Drains
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Wound dressing
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Physiotherapy
The following guidelines regarding physiotherapy must be adapted to the individual patient and injury.
It is important that the surgeon decide how much mechanical loading is appropriate for each patient's pelvic ring fixation. This must be communicated to physical therapy and nursing staff.
For all patients, proper respiratory physiotherapy can help to prevent pulmonary complications and is highly recommended.
Upper extremity and bed mobility exercises should begin as soon as possible, with protection against pelvic loading as necessary.
Mobilization can usually begin the day after surgery unless significant instability is present.
Generally, the patient can start to sit the first day after surgery and begin passive and active assisted exercises.
For unilateral injuries, gait training with a walking frame or crutches can begin as soon as the patient is able to stand with limited weight bearing on the unstable side.
In unstable unilateral pelvic injuries, weight bearing on the injured side should be limited to "touch down" (weight of leg). Assistance with leg lifting in transfers may be necessary.
Progressive weight bearing can begin according to anticipated healing. Significant weight bearing is usually possible by 6 week but use of crutches may need to be continued for three months. It should remembered that pelvic fractures usually heal within 6-8 weeks, but that primarily ligamentous injuries may need longer protection (3-4 months).
Fracture healing and pelvic alignment are monitored by regular X-rays every 4-6 weeks until healing is complete.
Bilateral unstable pelvic fractures
Extra precautions are necessary for patients with bilaterally unstable pelvic fractures. Physiotherapy of the torso and upper extremity should begin as soon as possible. This enables these patients to become independent in transfer from bed to chair. For the first few weeks, wheelchair ambulation may be necessary. After 3-4 weeks walking exercises in a swimming pool are started.
After 6 weeks, if pain allows, the patient can start walking with a three point gait, with less weight bearing on the more unstable side.
Full weight bearing is possible after complete healing of the bony or ligamentous legions, typically not before 12 weeks.













