Pubic ramus screw
1. Introduction
Operative treatment of pubic rami fractures
Fractures of the pubic rami are nearly always associated with further pelvic ring injuries.
The treatment of these fractures is guided by the displacement and other associated pelvic ring injuries.
In many cases, a strong periosteum, the inguinal ligament and the pectineal ligament will provide adequate stability and no additional treatment is required.
With more complex, unstable pelvic ring injuries, ramus fractures may require fixation to restore stability and promote healing.
The decision for operative vs. nonoperative is best made by evaluating the entire pelvic ring and its stability instead of focussing only on the ramus fracture.
For more complex injuries, posterior reduction and fixation must precede fixation of the ramus fractures. In these cases, the anterior fixation supplements and stabilizes the posterior fixation.
Options for fixation
Stabilization of ramus fractures can be performed by a variety of techniques:
- Internal fixation with an intramedullary screw
- Internal fixation with a plate
- Indirect stabilization with external fixation
Intramedullary screw fixation of ramus fractures is a form of anterior fixation that provides stability and can be inserted using either open or percutaneous techniques.
The decision to use this technique is based on the pelvic injury pattern, soft tissue, and the surgeons comfort with the anatomy and imaging.
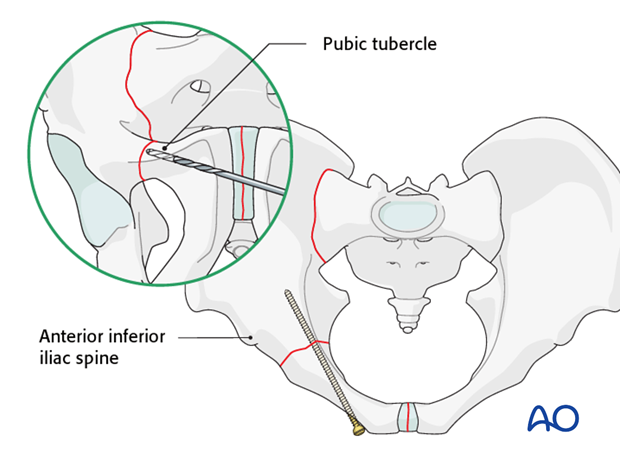
Percutaneous screws insertion sites
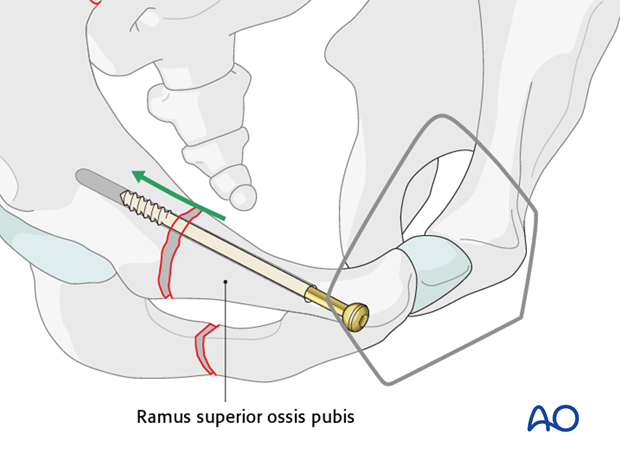
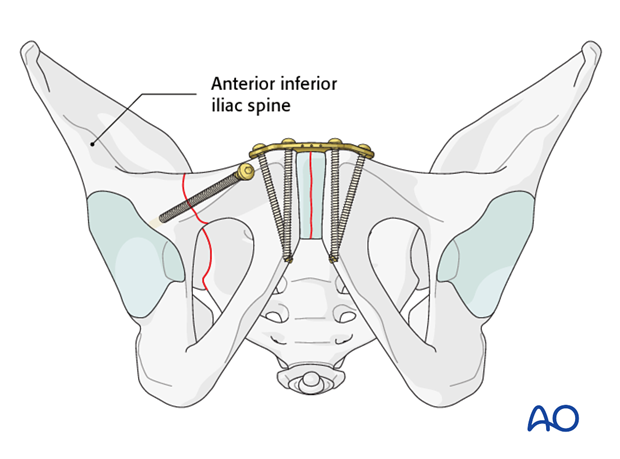
Intramedullary pubic ramus screws can be placed retrograde or antegrade through percutaneous stab wounds.
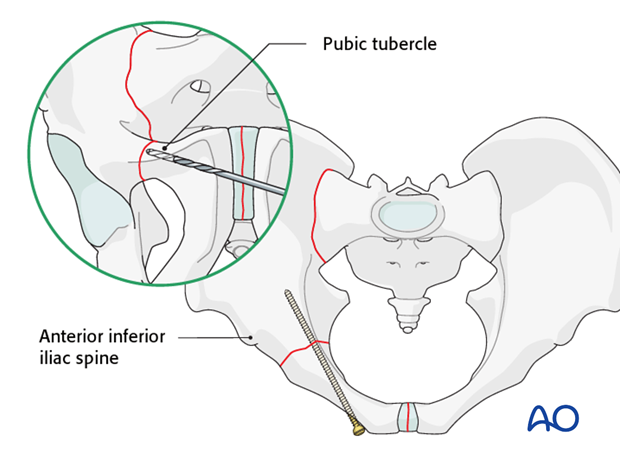
Retrograde screws, from the pubis laterally, are inserted through an incision made over the contralateral pubic tubercle. C-arm fluoroscopy is essential to define the starting point and passage of drill bit and screw within the superior pubic ramus, across the fracture, and cephalad to the acetabulum. The inlet and obturator outlet views are essential for confirming proper screw placement.
For more lateral fractures, an antegrade screw may be inserted from a stab wound cephalad to the hip joint along the same trajectory as the retrograde screw, but in the opposite direction.
2. Reduction
Reduction of the pelvic ring must be achieved prior to insertion of the intramedullary screw. It is important to understand that the screw functions simply to hold the reduction but in most cases does not achieve the reduction.
Reduction can be achieved by either closed or open methods.
Closed reduction
Closed reduction of ramus fractures typically requires reduction of the overall pelvic ring. In cases with displaced posterior ring injuries, reduction of the posterior ring may help to indirectly reduce the ramus fractures.
Other methods of closed reduction include percutaneous manipulation of the pelvic ring using Schanz screws. After reduction is achieved (verified by X-ray), the reduction may be held by an adjacent K-wire or external fixator during screw insertion.
A fracture gap in the ramus may be reduced by inserting a partially threaded lag screw. As the screw is tightened, the gap is closed.
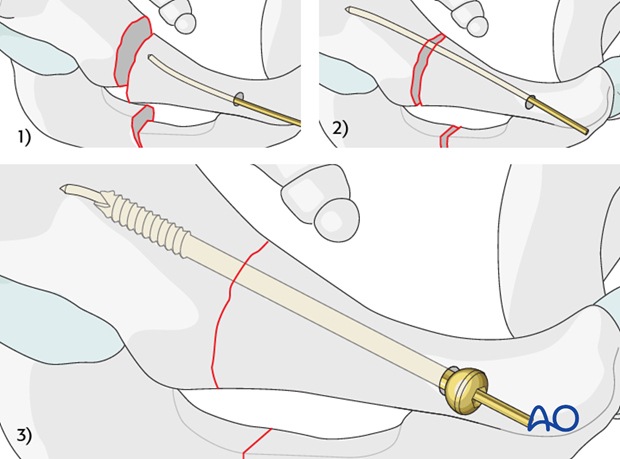
Small amounts of displacement may be able to be reduced using cannulated screws. In these cases, a gently curved guide wire is used to traverse the mildly displaced fracture. Once the screw is inserted over the guide wire the fracture is indirectly reduced by screw insertion.
The K-wire should be removed once the screw is sufficiently past the fracture line.
Open reduction
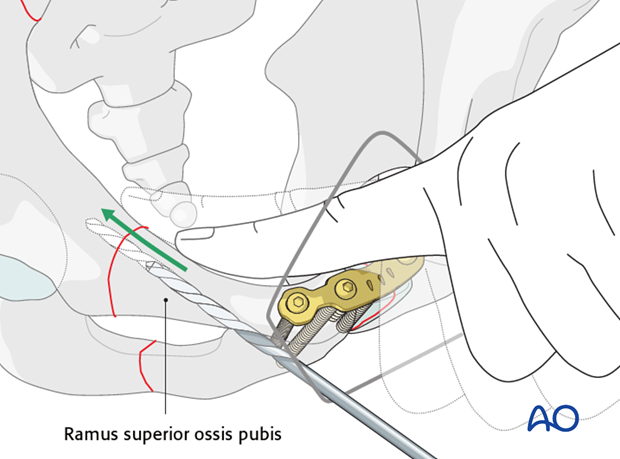
The medial aspects of the superior pubic rami are exposed using an extended Pfannenstiel approach.
After exposure, the fracture may be directly manipulated with bone holding forceps.
Note
Be alert for rotational malalignment of the fracture. This can be corrected by derotation by bone holding forceps.
3. Screw insertion
Determine the type of screw
The type of screw that is chosen for fixation depends on the fracture pattern, location, patient's size and anatomy, and surgeon's preference.
Screws that are commonly used are:
- 3.5 mm cortical screws
- 4.5 mm cortical screws
- 6.5 or 7.3 mm cancellous screws
Cannulated screws as described above are also advantageous.
Screw entry point
Intramedullary screws for fixation of ramus fractures may be inserted in an antegrade or retrograde fashion.
The choice of the direction of insertion depends on the location of the fracture and surgeon's preference. Ramus fractures that are located closer to the pubic symphysis are often easier to reduce and control using a retrograde screw. In contrast more proximal ramus fractures are better stabilized with an antegrade screw.
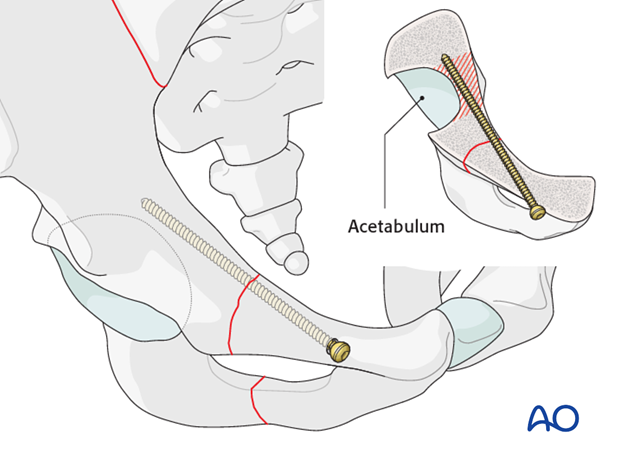
Retrograde screw
Choose the entry point caudal to the pubic tubercle as lateral as possible to optimize the screw direction in respect to the fracture line.
The screw is directed proximal and superior to avoid the acetabulum.
Check the orientation
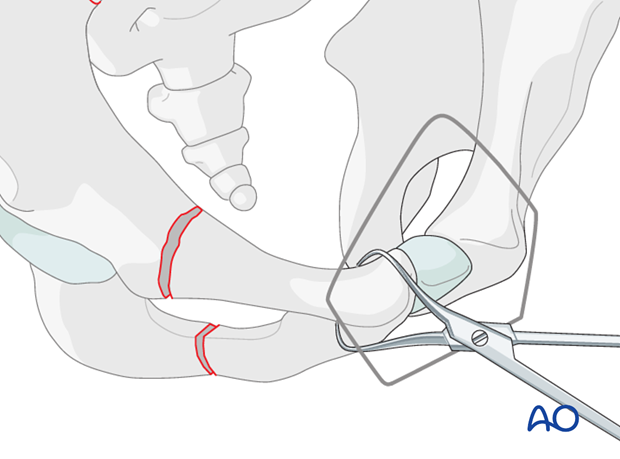
The direction of the screw is determined using X-ray guidance. If an open technique is used for a retrograde screw, then check the orientation with the index finger along the inner side of the pubic ramus, as illustrated.
Proximity to the hip joint
Whether inserting a retrograde or an antegrade screw, great care must be taken to prevent the screws from penetrating the hip joint.
The cross section of the anatomic model shows the correct screw position in the anterior column across the fracture side.
It displays the close relationship of the implant to the joint.
Drilling and length measurement
The type of drill used will depend on the diameter of screw chosen. The drill is observed using X-ray guidance as it is carefully advanced. Unless the bone is very hard, only the near cortex needs to be drilled, as the screw will advance through the cancellous bone by itself.
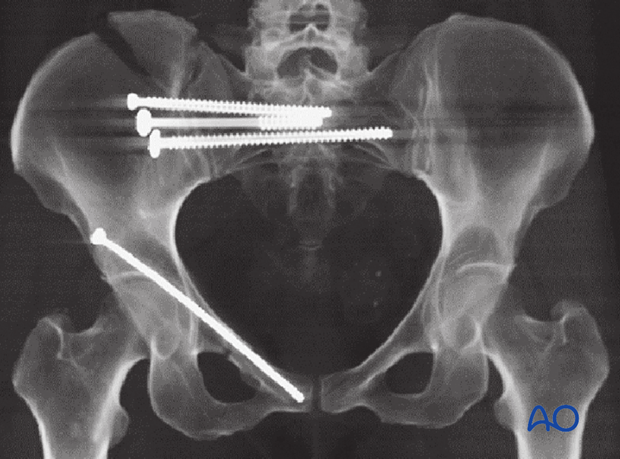
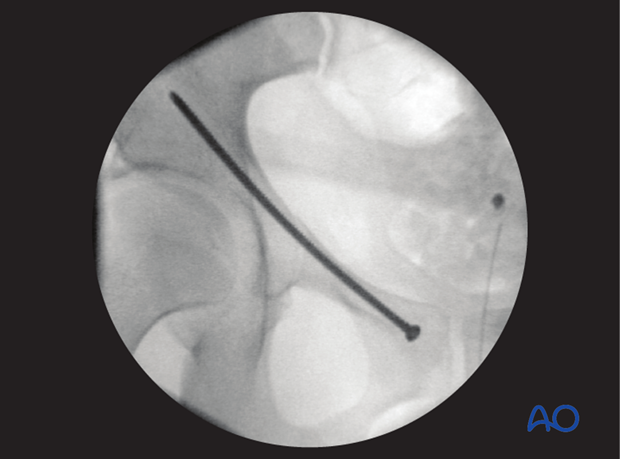
Multiple X-ray views are obtained intraoperatively to ensure that the screw does not penetrate the acetabulum and remains safely within the bone (inlet view, obturator oblique view).
The inlet view is used to ensure that the drill and later the screw do not penetrate the inner cortex of the ramus.
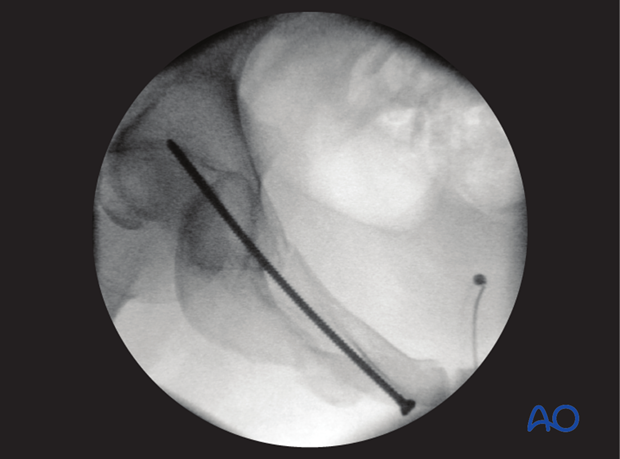
The obturator oblique view is used to ensure that the drill and later the screw do not penetrate the acetabulum.
A depth gauge could be used to measure the length of the screw.
When cannulated screws are used, the guide wire is used to determine the length and the position of the screw.
4. Post-operative X-rays
At the completion of fixation, it is necessary to obtain AP, inlet, and outlet X-ray views of the pelvic ring, and obturator and iliac oblique views to ensure the acetabulum is not penetrated by the screw.














