Lag screw fixation of proximal articular fractures of the 1st-4th metatarsal
1. General considerations
Strategy options for complete articular fractures
Two options are available:
- Reduce and fix the articular segment to create an A-type pattern. The extraarticular fracture is then reduced to the main fragment and fixed in a second step.
- Reduce all fragments with temporary fixation, followed by definitive screw fixation. Typically, the screw fixation would start with the fixation of the articular block.
Displaced fractures
Displaced fractures may be associated with first tarsometatarsal instability. Reduction of the articular surface and alignment of the first tarsometatarsal joint and its associated soft tissues are essential in treating this injury.
2. Reduction
Visualization
Expose the articular surfaces.
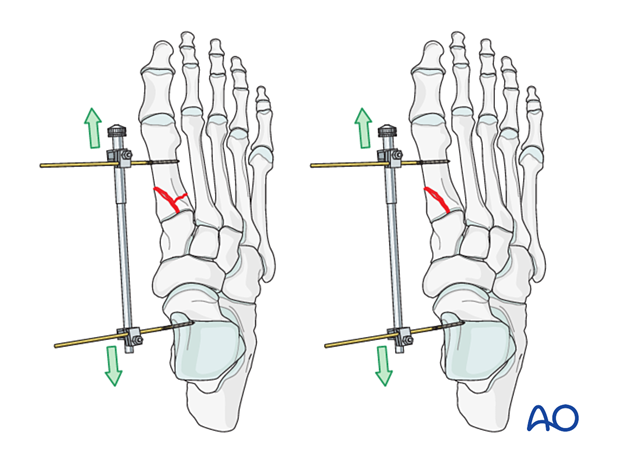
Visualization may be improved by longitudinal manual distraction.
For fractures involving the first metatarsal, a mini distractor may be helpful. Visualization may be improved by releasing the dorsal insertion of the extensor hallucis brevis or extensor digitorum brevis (EHB or EDB).
The extensor hallucis longus should be preserved.
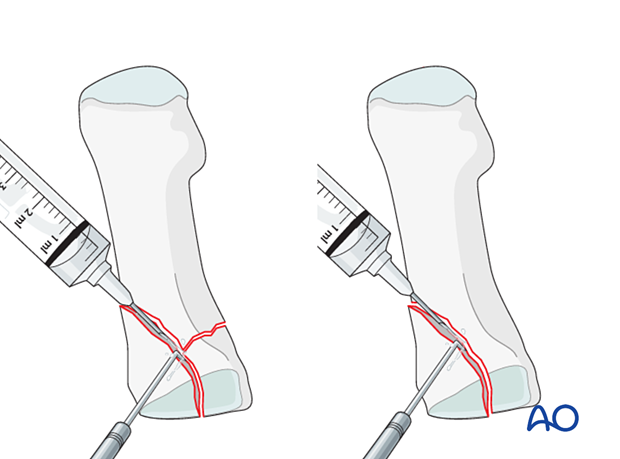
Irrigation
Clean the fracture using a dental pick. Direct suction or irrigation is helpful.
The fracture edges are exposed, and the fragment mobility is assessed. Take great care to avoid comminution of any fragment. It is essential to maintain the vascularity of small fragments.
The extent of articular involvement is assessed, including separate osteochondral fragments.
Reduction
Anatomical reduction of the joint surface is essential to prevent chronic instability or posttraumatic degenerative joint disease.
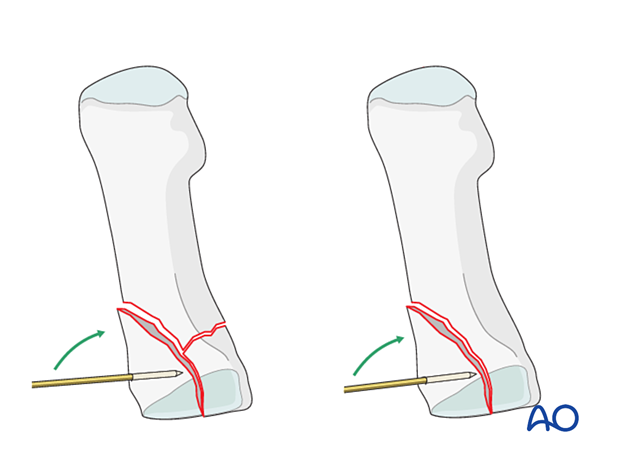
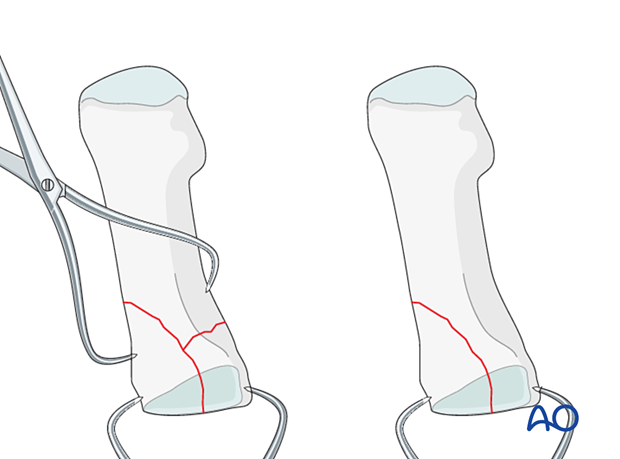
The articular fragments are manipulated using a dental pick, small K-wires as joysticks, or a small periosteal elevator.
If reconstruction of the articular surface is not feasible, a fusion of the joint should be considered.
Small K-wires can be inserted across the fracture line for preliminary fixation.
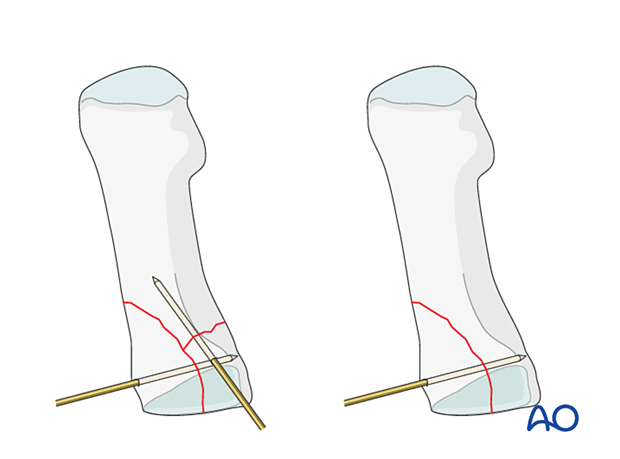
Depending on fracture configuration, pointed reduction forceps may also be used for reduction and preliminary fixation.
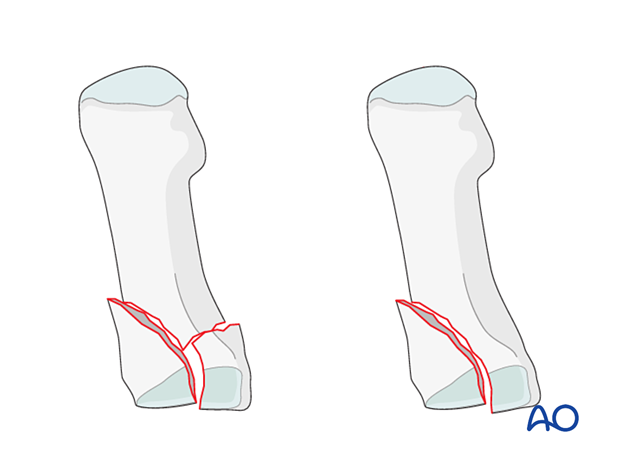
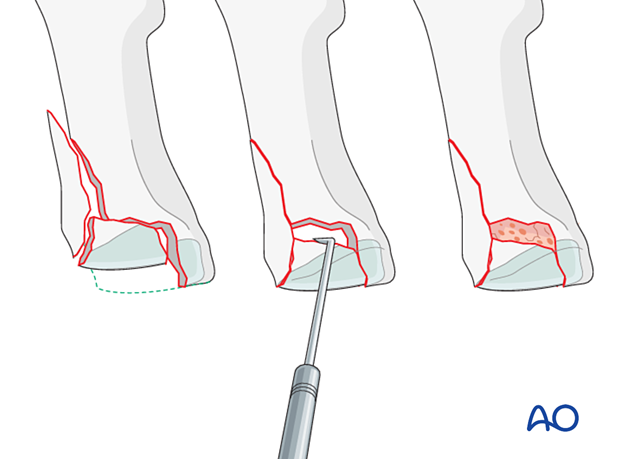
Reduction of impacted fractures
PrincipleCentrally impacted fragments in compression fractures are devoid of soft-tissue attachments and are therefore not reducible by ligamentotaxis.
Direct reduction is necessary.
The key to fixing compression fractures is restoring the joint surface to as close as normal as possible and supporting the reduction with bone graft and internal fixation.
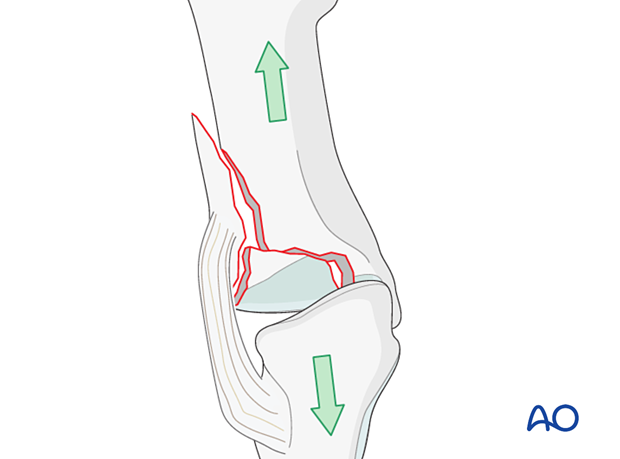
Using a K-wire, or dental pick, the fragments are disimpacted and pushed towards the opposing bone, which is used as a template to ensure congruity of the articular surface.
Since the metaphyseal cancellous bone is impacted, a void may be created by its disimpaction.
This void jeopardizes the fracture in two ways:
- It is a very unstable situation in which the articular fragments may easily displace (collapse)
- The healing process is delayed
The bony defect under the fragments is filled with cancellous bone graft. The bone graft also helps keep the fragments in place when the screw fixation is performed.
Visual inspection of the reduction
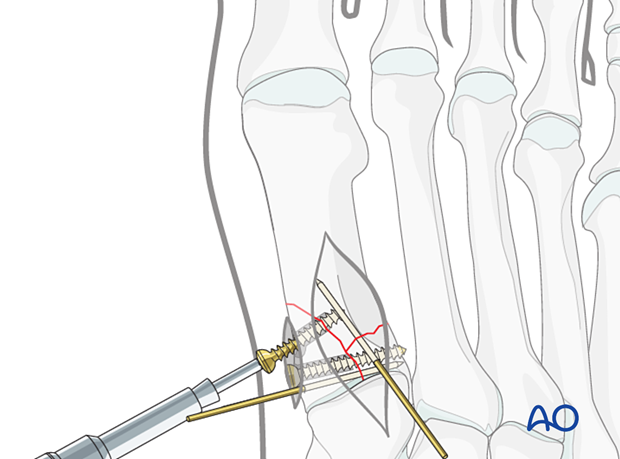
Anatomical reduction of the joint surface must be checked under direct visualization and image intensification.
Length, alignment, and rotation of all metatarsals and joints must be maintained.
3. Fixation
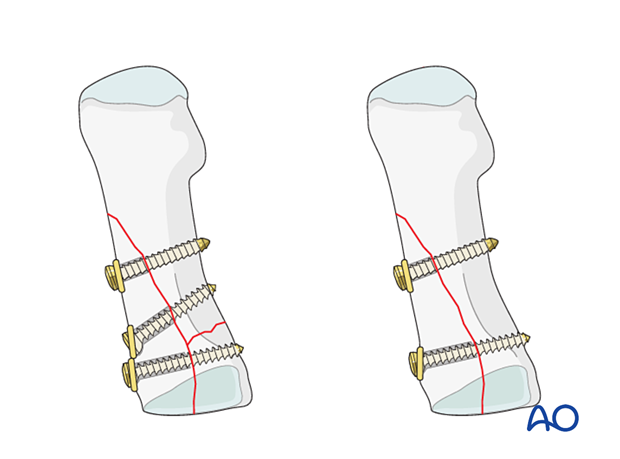
Fixation of the articular block
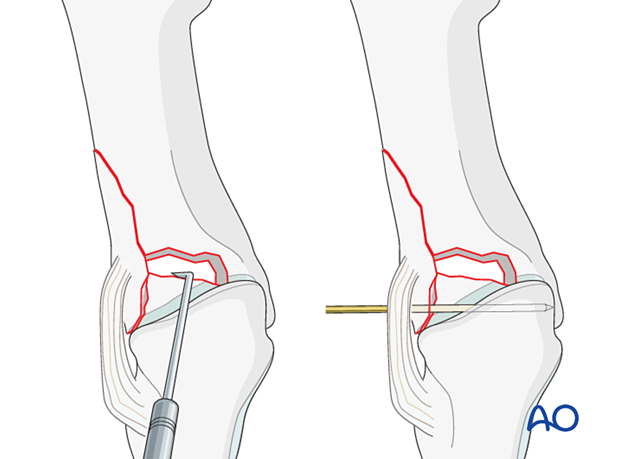
Lag screw fixation of the articular surface should be performed first.
Insert a 2.0 mm or 2.4 mm lag screw perpendicular to the fracture plane.
The lag screws should be placed outside of the articular surface.
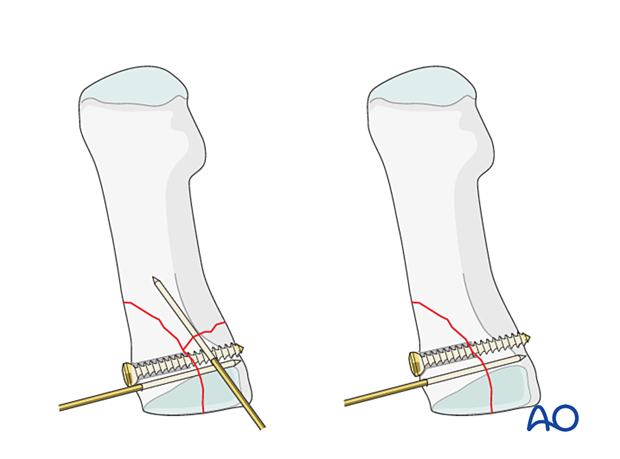
Fixation of the articular block to the shaft
If possible, fix the articular block to the shaft using lag screw.
The extraarticular fracture can be addressed with either a plate or K-wires if lag screw fixation is impossible (see fixation of simple extraarticular fractures).

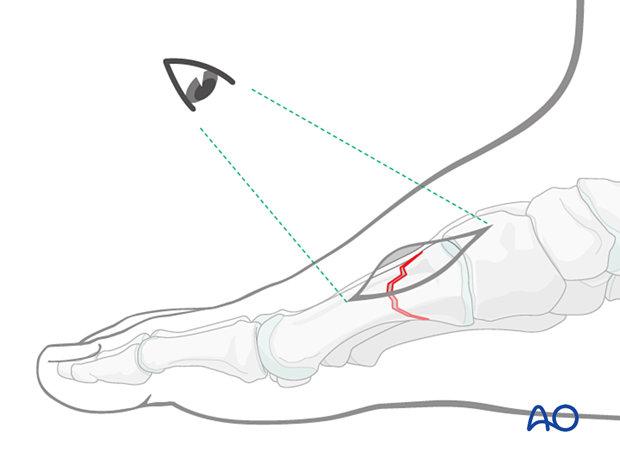
Percutaneous screw insertion
For fractures of the first metatarsal, the lag screws may be inserted percutaneously.
Fixation in osteoporotic bone
If one is dealing with osteoporotic bone, then a washer under the head of the screw is helpful to prevent the head from sinking.
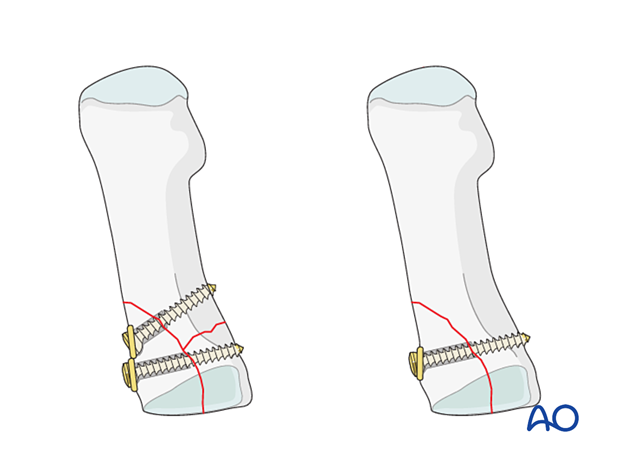
Insertion of additional lag screws for long oblique fractures
A second or third lag screw may be inserted for long oblique fractures. If one is dealing with osteoporotic bone, then a washer under the head of the screw is helpful to prevent the head from sinking.
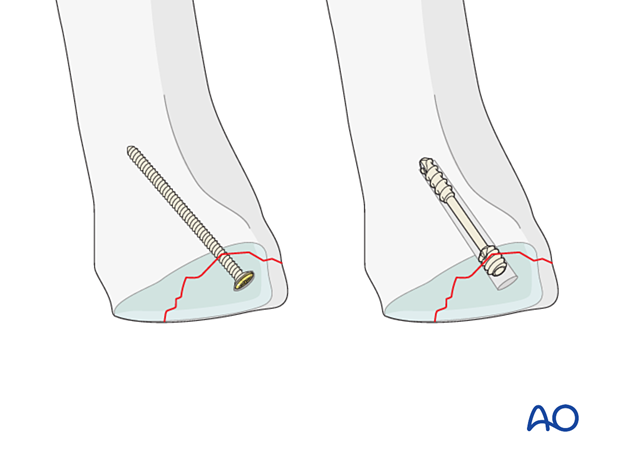
4. Fixation of osteochondral fragments
Small fragments are best stabilized with screws inserted through the articular cartilage.
Choose the smallest possible screw diameter to minimize the damage to the joint surface.
If headless screws are available in very small sizes, they have the advantage that they can be inserted deeper into the fragment without protruding.
The opposite cortex may be engaged depending on the fracture configuration and available screw lengths.
Drilling and measuring
Drill carefully not to displace the fragments.
Measure the correct screw length with a depth gauge. When measuring, be careful not to displace the reduced fragments.
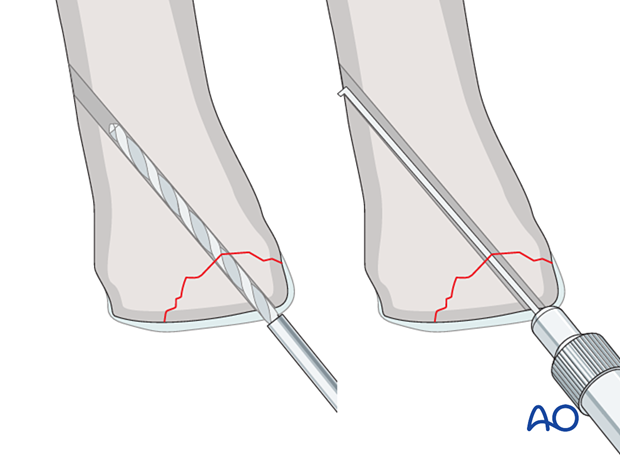
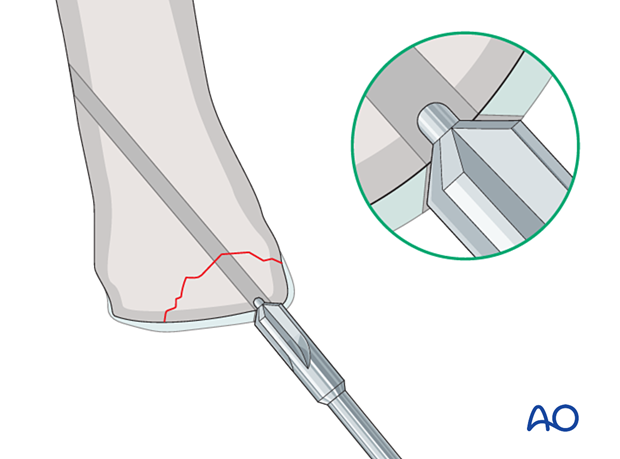
Countersinking the articular cartilage
When standard (headed) screws are used, the cartilage is countersunk to facilitate the burial of the screw head.
Screw insertion
Carefully insert the screw without displacing the reduced fragments. Ensure that the screw head is buried in the articular cartilage and does not protrude into the joint.
Insert additional screws as needed using a similar technique.
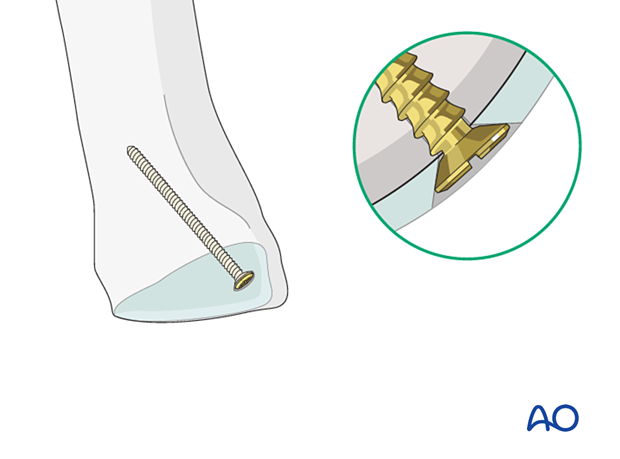
Intraoperative radiologic and visual assessment of joint motion is critical to verify sufficient countersinking.













