Intramedullary screw or lag screw fixation
1. Principles
Anatomical considerations
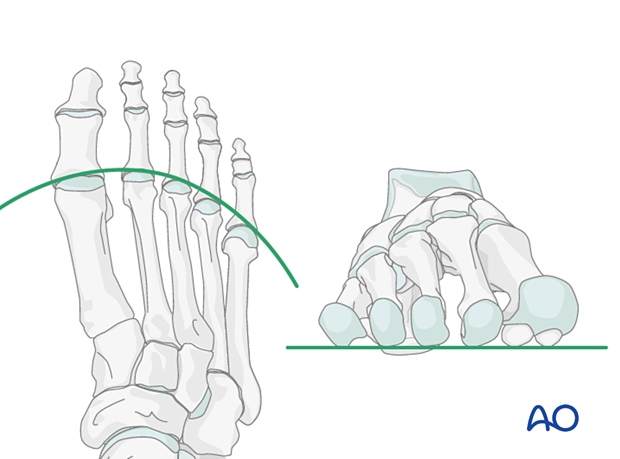
Proper alignment of the metatarsal heads is a critical goal in restoring the forefoot mechanics.
A normal curved “cascade” (Lelièvre’s parabola) appearance, which is symmetric with the other foot, is mandatory on the AP view. See illustration. This symmetry ensures that the normal length of the metatarsal is restored.
It is also critical to restore the metatarsals in their axial or horizontal plane so that all the metatarsal heads are on the same level in the axial view.
Any malalignment, particularly flexion, will recreate focally high pressure during the stance phase and toe-off, resulting in pain and subsequent callus formation.
The sesamoids, rather than the first metatarsal head, bear weight in the first row. Therefore, one must look at the sesamoid level in establishing the alignment in the axial or horizontal plane of the first metatarsal.
Fixation options
One should strive for maximal stability when fixing extraarticular fractures of the proximal 5th metatarsal (Jones fracture).
In a single-plane fracture with good bone stock, one single interfragmentary lag screw is adequate.
The screw may be inserted as a standard bicortical lag crew or an intramedullary lag screw.
Both techniques will be illustrated below.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

2. Patient preparation
This procedure is typically performed with the patient placed supine with the knee flexed at 90°.

3. Approach
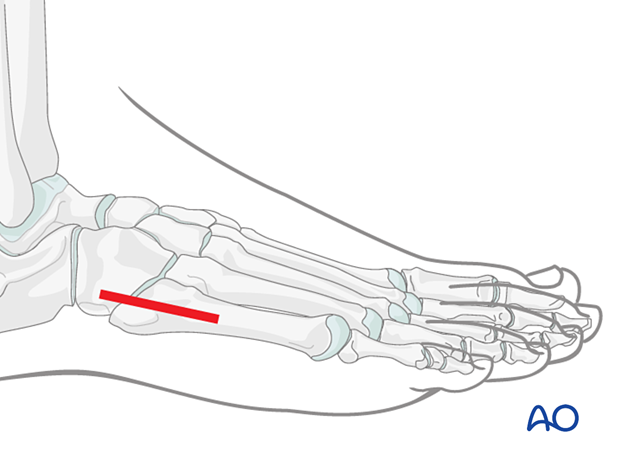
Most of these fractures can be fixed with percutaneous screw fixation.
The fracture can be accessed through a lateral approach to the fifth metatarsal when an open procedure is needed.
4. Reduction
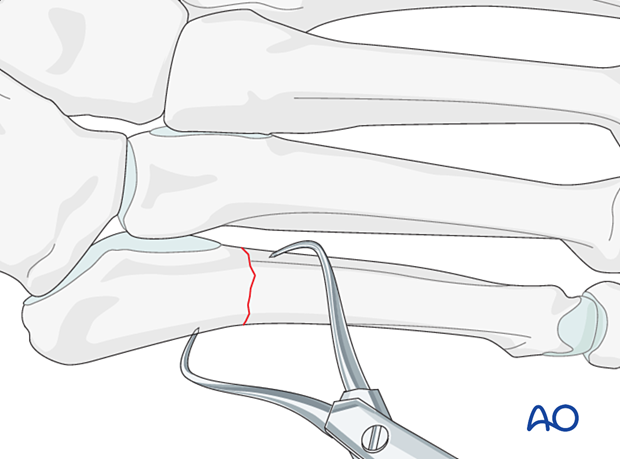
In cases of displaced fractures, an open reduction will be required.
Secure and maintain the reduction with pointed reduction forceps.
5. Screw fixation
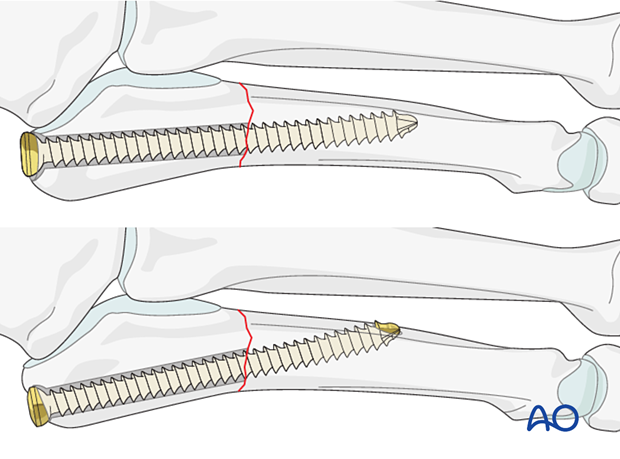
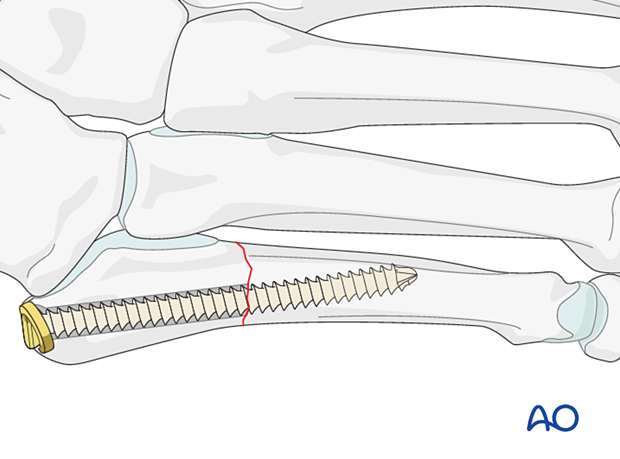
Intramedullary lag screw fixation
The screw entry point is identified using fluoroscopy. It is colinear with the medullary canal in AP and lateral views.
The intermedullary screw is inserted following the standard procedure but with the considerations listed below.
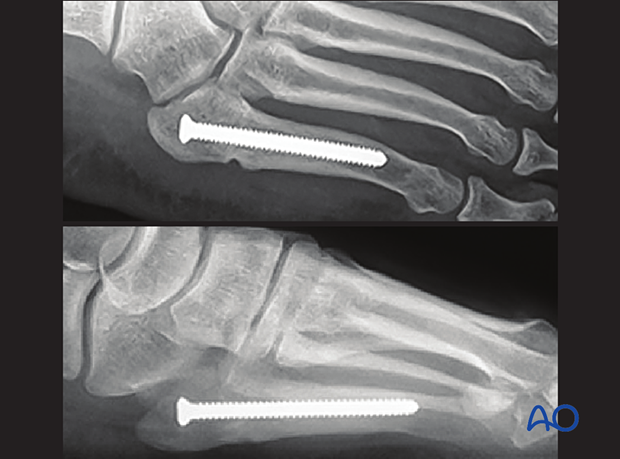
The screw must be of sufficient diameter to obtain purchase in the endosteum of the medullary canal to generate compression. Depending on the size of the canal, a 3.5 mm or 4.5 mm cortex screw is chosen.
Due to the curvature of the 5th metatarsal, care must be taken when selecting the screw length such that it does not inadvertently exit the medullary canal. This will increase the risk of an iatrogenic shaft fracture.
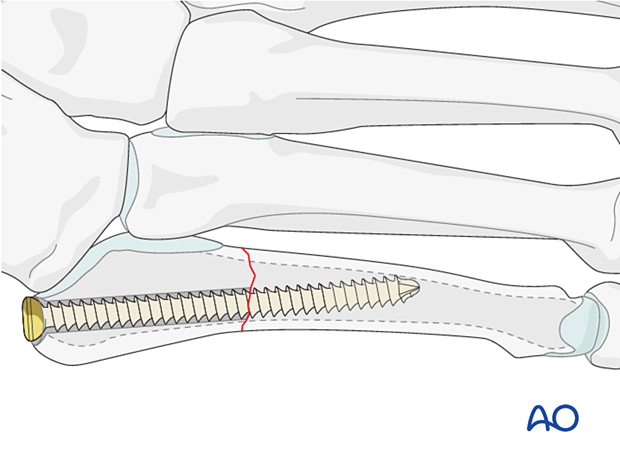
A washer may be indicated in osteoporotic bone.
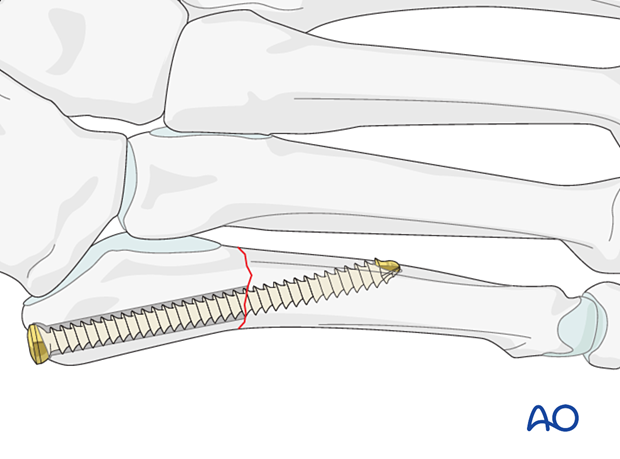
Bicortical lag screw
An alternative technique is bicortical lag screw fixation.
The screw enters the styloid process through the peroneus brevis tendon insertion and continues obliquely as it proceeds medially and distally. It gains purchase in the strong medial cortex distal to the fracture.
The screw size should be selected according to the size of the bone. 3.5 screws are usually sufficient.
6. Aftercare
An appropriate well-padded dressing should be applied to protect the surgical incision. Compression will help control swelling.
If present, the skin-pin interface should be similarly well-padded but with dressings that can be readily removed to inspect for pin site infection.
Immediate postoperative treatment is rest, ice, and elevation.
The patient should restrict weight-bearing for six weeks until signs of radiographic healing are present. After this, patients can be weight-bearing as tolerated.
Patients must exercise their ankle and subtalar joints out of the orthosis to prevent stiffness (eg, by stretching their Achilles).
X-ray the metatarsals at six weeks to confirm satisfactory union and remove K-wires if present. Once the fracture is united, the orthosis may be gradually discontinued.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid- and hindfoot.
If the gastrocnemius muscle has been released, a splint or cam walker can be used to protect the surgical site.













