Intramedullary K-wire fixation
1. Introduction
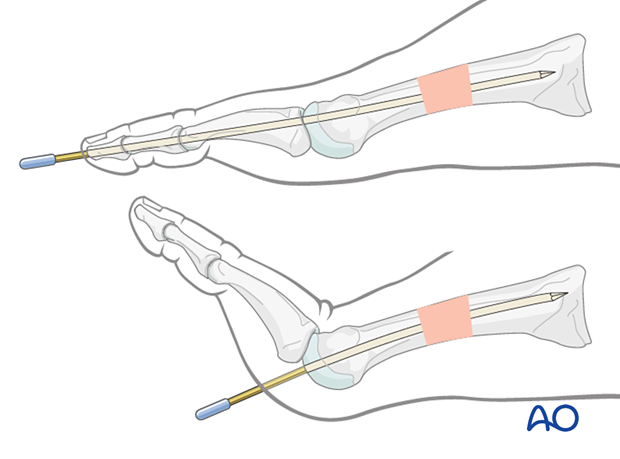
Intramedullary implants can be inserted retrograde, either directly through the metatarsal head or from the tip of the phalanx.
One variation of this technique is to insert the K-wire in an antegrade manner through the fracture site, protruding distally through the skin. The fracture is reduced, and the K-wire is passed retrograde across the fracture.
Here we will describe the direct insertion through the metatarsal head as it is less damaging and easier to perform.
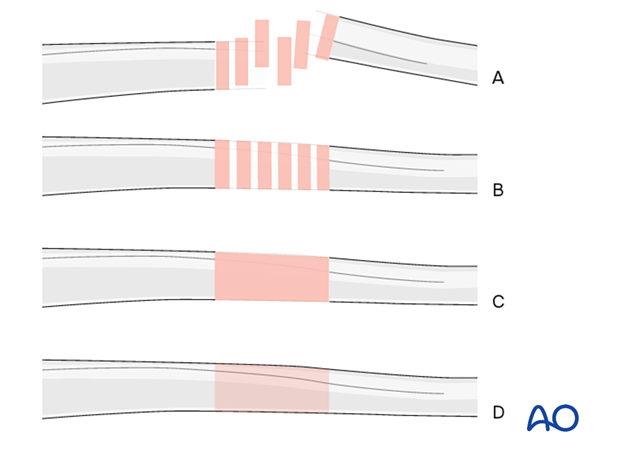
Throughout this treatment option illustrations of generic fracture patterns are shown, as four different types:
A) Unreduced fracture
B) Reduced fracture
C) Fracture reduced and fixed provisionally
D) Fracture fixed definitively
Anatomical considerations
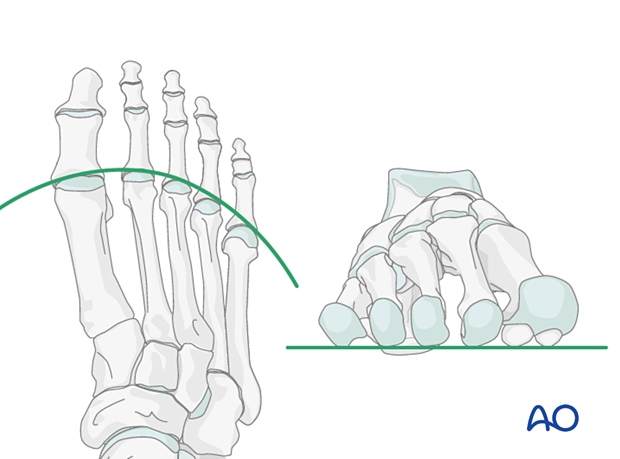
Proper alignment of the metatarsal heads is a critical goal in restoring the forefoot mechanics.
A normal curved “cascade” (Lelièvre’s parabola) appearance, which is symmetric with the other foot, is mandatory on the AP view. See illustration. This symmetry ensures that the normal length of the metatarsal is restored.
It is also critical to restore the metatarsals in their axial or horizontal plane so that all the metatarsal heads are on the same level in the axial view.
Any malalignment, particularly flexion, will recreate focally high pressure during the stance phase and toe-off, resulting in pain and subsequent callus formation.
The sesamoids, rather than the first metatarsal head, bear weight in the first row. Therefore, one must look at the sesamoid level in establishing the alignment in the axial or horizontal plane of the first metatarsal.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

2. Patient preparation
This procedure is typically performed with the patient placed supine with the knee flexed at 90°.

3. Approaches
A limited exposure using one of the following approaches may be needed to facilitate reduction:
4. Creating an entry portal
It is crucial to identify the correct starting point. However, this can be difficult.
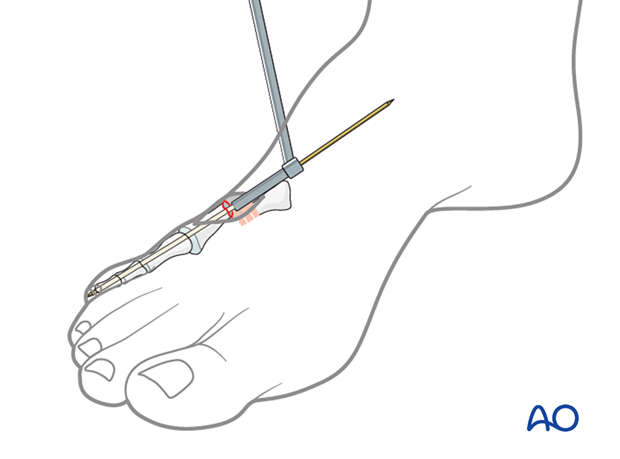
Hyperextend the MTP joint.
At the flexion crease, insert a 2.0 K-wire in the midline of the digit.
Manipulate the K-wire under fluoroscopic control to locate the apex of the metatarsal head.
Verify this location in AP and, if possible, in lateral or oblique views.
5. Reduction and fixation
Control of distal segment
An additional K-wire inserted dorsally may be needed to control the distal segment.
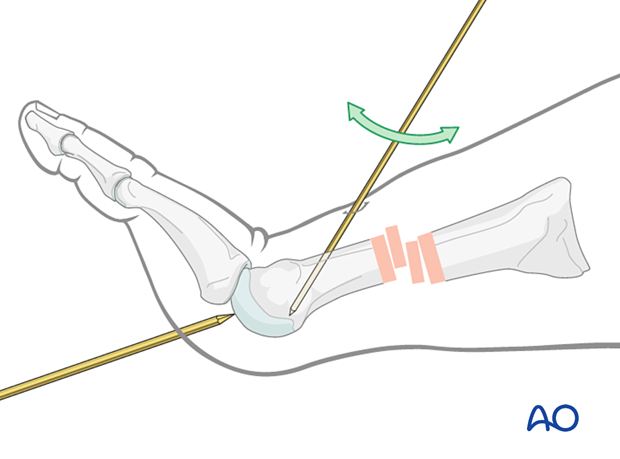
K-wire insertion in distal segment
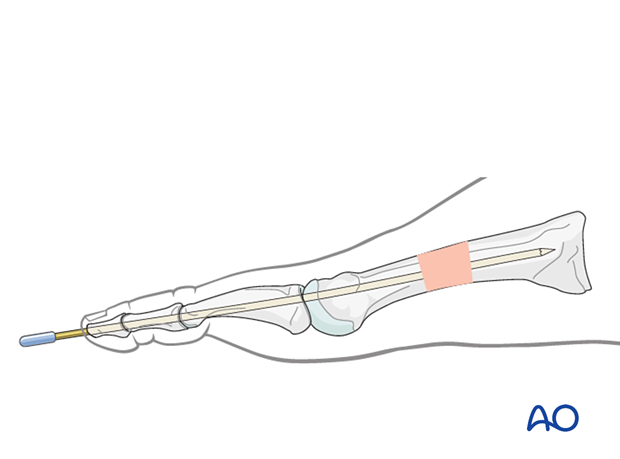
Insert a straight 1.6 or 2.0 K-wire trochar tip wire through the articular surface into the medullary canal.
Insertion is facilitated by oscillating the wire.
Confirm the K-wire trajectory using fluoroscopy.
Advance the K-wire up to the fracture.
Reduction
A closed reduction will often be challenging to accomplish. In some cases, an open reduction may need to be performed through a small incision centered over the fracture dorsally.
In shaft fractures, perform the reduction using reduction forceps on either end of the fracture. If possible, apply the forceps across the fracture.
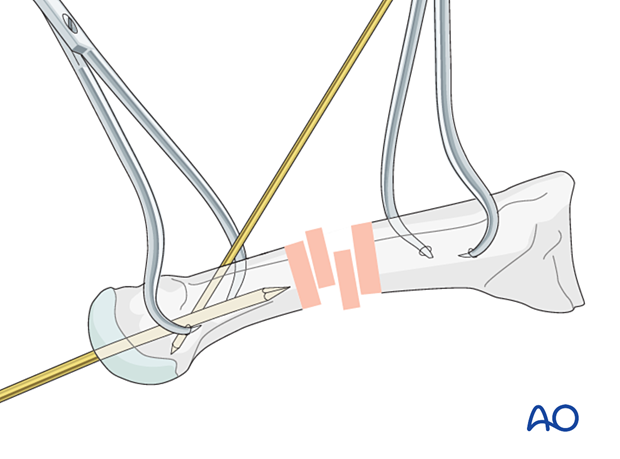
Gross alignment of the medullary canal will suffice for K-wire passage in multifragmentary fractures.
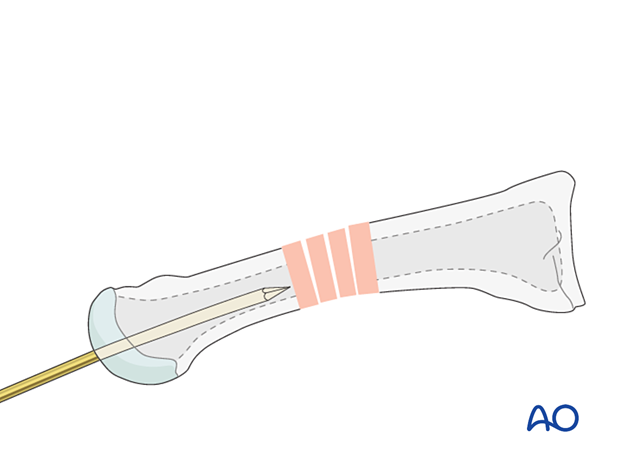
Advance the wire across the fracture up to the base of the metatarsal. Ensure appropriate length, alignment, and rotation.
The wire may be inserted across the tarsometatarsal joint for additional stability.
Trim the wire 2–5 mm from the skin margin and place a wire cap.

6. Alternative K-wire insertion techniques
Insertion at the tip of the toe
An alternative start point would be at the tip of the digit, which would require the K-wire to be inserted across the DIP and PIP joints along the central axis of the toe.
Inside-out technique
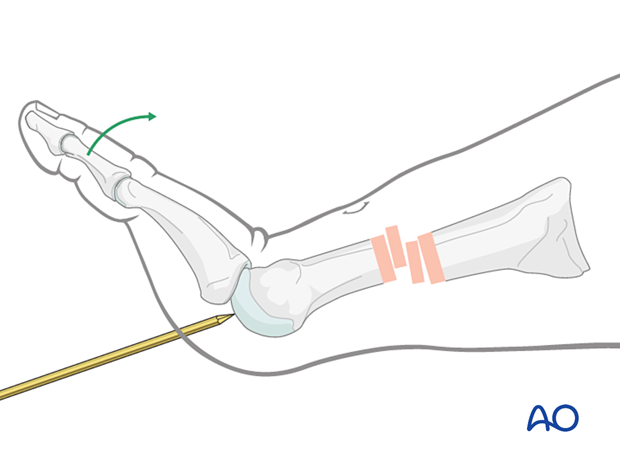
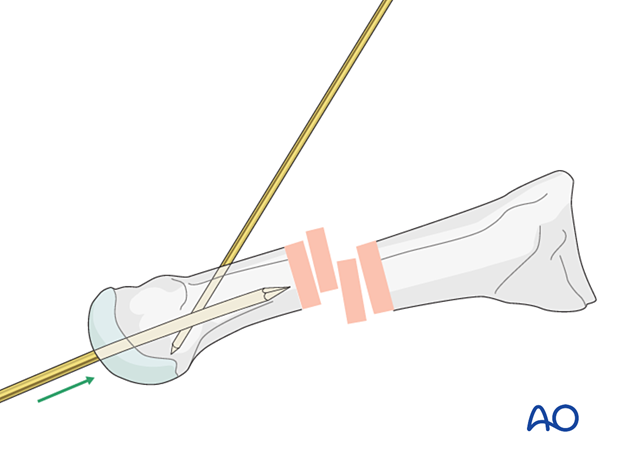
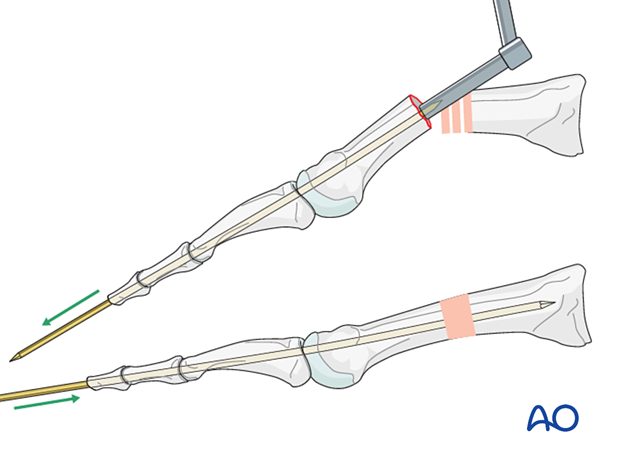
Another option is to introduce a double-ended K-wire in an antegrade fashion with the inside-out technique.
A limited dorsal approach to the metatarsal is centered over the fracture site.
Flex the distal fragment to gain an optimal view of the fracture surface.
Debride the fracture site.
Hyperflex the toe and insert the K-wire into the medullary canal. Advance the K-wire distally within the medullary canal, through the metatarsal head, and until it exits the skin.
Leaving the drill guide in place for soft-tissue protection, pull on the K-wire's distal end until the proximal end is flush with the fracture surface.
Use the K-wire as a joystick to reduce or manipulate the fracture manually.
Advance the K-wire retrograde to the base of the fractured metatarsal or cuneiform.
7. K-wire removal
The K-wire is removed in the clinic upon evidence of radiographic healing (typically at 6–8 weeks).
8. Aftercare
An appropriate well-padded dressing should be applied to protect the surgical incision. Compression will help control swelling.
If present, the skin-pin interface should be similarly well-padded but with dressings that can be readily removed to inspect for pin site infection.
Immediate postoperative treatment is rest, ice, and elevation.
The patient should restrict weight-bearing for six weeks until signs of radiographic healing are present. After this, patients can be weight-bearing as tolerated.
Patients must exercise their ankle and subtalar joints out of the orthosis to prevent stiffness (eg, by stretching their Achilles).
X-ray the metatarsals at six weeks to confirm satisfactory union and remove K-wires if present. Once the fracture is united, the orthosis may be gradually discontinued.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid- and hindfoot.
If the gastrocnemius muscle has been released, a splint or cam walker can be used to protect the surgical site.













