Dorsal spanning plate
1. General considerations
Plating principles
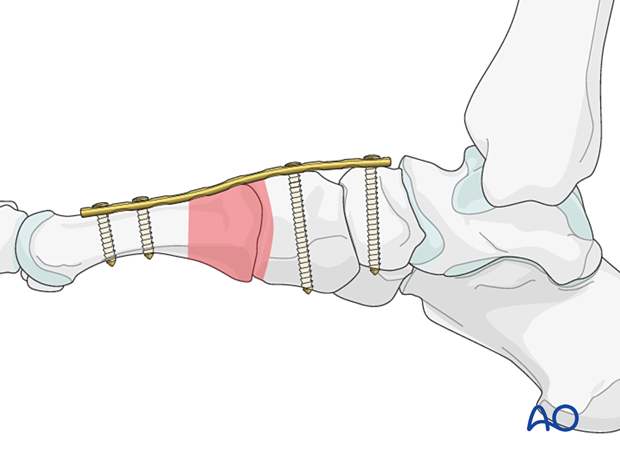
The plating technique can be used for definitive or temporary stabilization of the midfoot with damage control surgery. In this case, dorsal spanning plates are used to provisionally stabilize the foot’s medial and/or lateral columns.
Once the soft tissue envelope improves, the dorsal spanning plate can be removed, and definitive fixation is performed.
The plating technique can also protect reconstructions of the Lisfranc or Chopart joint.
When protecting a Chopart fracture, the plate goes from the talus to the metatarsals.
The plate is removed after the reconstruction has healed.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

2. Patient preparation
This procedure is typically performed with the patient placed supine with the knee flexed at 90°.

3. Approaches
In the case of damage control, the surgeon may use preexisting open wounds or smaller versions of the following approaches:
- Dorsal approach to multiple metatarsals
- Dorsal approach to single metatarsals 2–4
- Dorsal approach to the first metatarsal
Small incisions will preserve any remaining blood supply to the remaining blood and soft tissue envelope, which is particularly important in a severely traumatized foot.
When used as a protection plate for definitive reconstruction, the preexisting surgical incisions are extended proximally and distally to allow plate fixation.
4. Plate selection
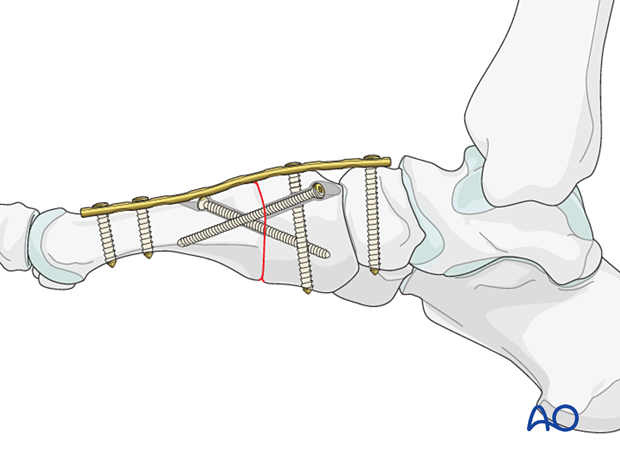
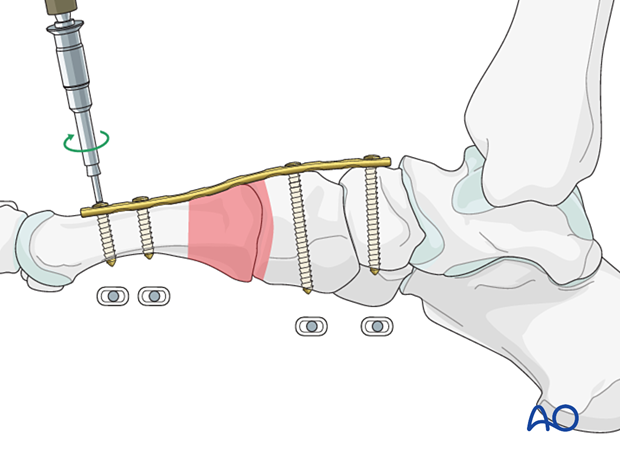
The plate should be long enough to allow two screws to be inserted into each side of the injured column.
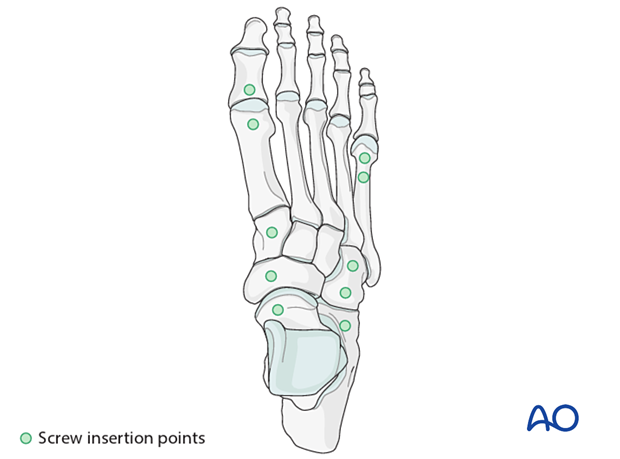
The distal screw insertion points include the distal metatarsals.
The proximal screw insertion points include the:
- Navicular
- Cuneiform
- Cuboid
- Calcaneum
A 3.5 mm plate(s) should be used for all metatarsals. However, 2.7 plates can be used in the lesser metatarsals depending on the patient's anatomy.
5. Reduction (in case of damage control)
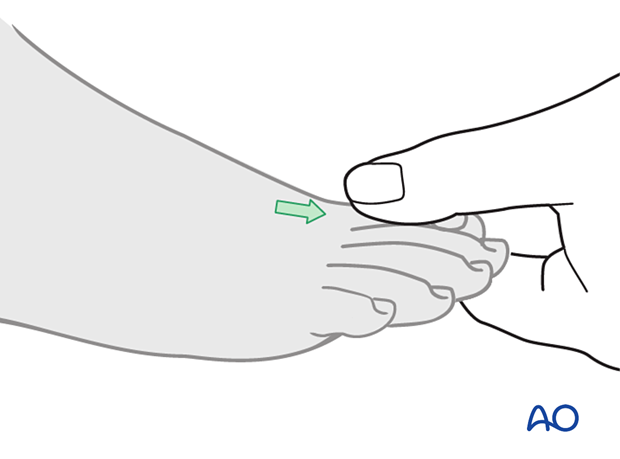
Manual traction
Manual traction on the toe or manual reduction of the Chopart or Lisfranc fracture/fracture-dislocation, as illustrated, will usually regain the correct length, rotation, and alignment of the distal metatarsal segment.
Most Lisfranc or Chopart injuries will displace dorsally and require a manual force to reduce them.
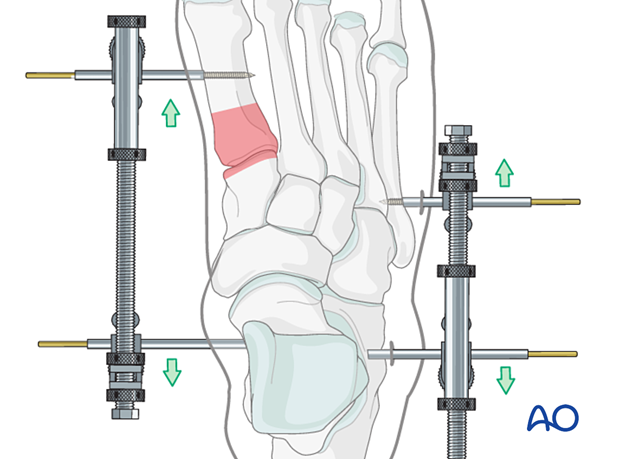
External fixation
Medial or lateral column external fixation may be used to assist in restoring the anatomy before plate fixation.
The external fixator may be left in place in some instances until definitive reconstruction is performed.
6. Plate application
An appropriately contoured plate is placed dorsally to span the injured region.
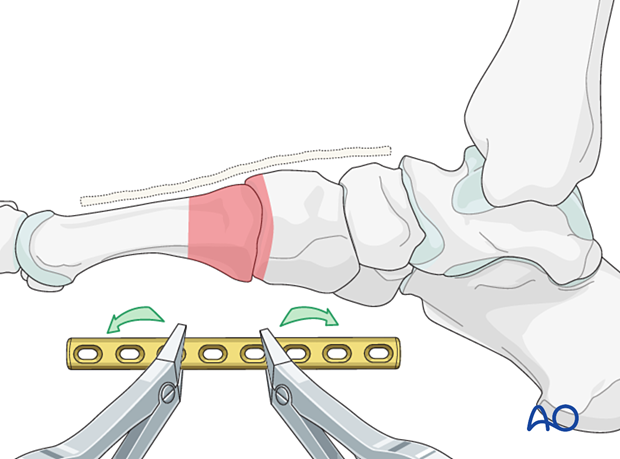
The plate is fixed by inserting screws in neutral mode, with the fracture reduced and out to length.
7. Aftercare
An appropriate well-padded dressing should be applied to protect the surgical incision. Compression will help control swelling.
If present, the skin-pin interface should be similarly well-padded but with dressings that can be readily removed to inspect for pin site infection.
Immediate postoperative treatment is rest, ice, and elevation.
The patient should restrict weight-bearing for six weeks until signs of radiographic healing are present. After this, patients can be weight-bearing as tolerated.
Patients must exercise their ankle and subtalar joints out of the orthosis to prevent stiffness (eg, by stretching their Achilles).
X-ray the metatarsals at six weeks to confirm satisfactory union and remove K-wires if present. Once the fracture is united, the orthosis may be gradually discontinued.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid- and hindfoot.
If the gastrocnemius muscle has been released, a splint or cam walker can be used to protect the surgical site.













