T-plate fixation with compression
1. Preliminary remarks
In transverse or short oblique extraarticular fractures of the metatarsal base, fixation can be achieved by compression plating.
Anatomical considerations
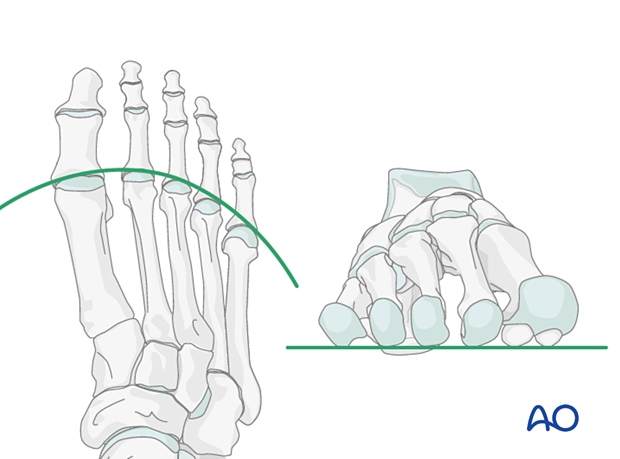
Proper alignment of the metatarsal heads is a critical goal in restoring the forefoot mechanics.
A normal curved “cascade” (Lelièvre’s parabola) appearance, which is symmetric with the other foot, is mandatory on the AP view. See illustration. This symmetry ensures that the normal length of the metatarsal is restored.
It is also critical to restore the metatarsals in their axial or horizontal plane so that all the metatarsal heads are on the same level in the axial view.
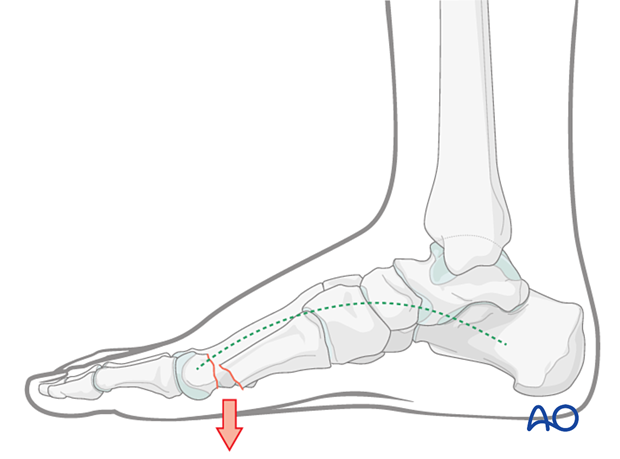
Any malalignment, particularly flexion, will recreate focally high pressure during the stance phase and toe-off, resulting in pain and subsequent callus formation.
The sesamoids, rather than the first metatarsal head, bear weight in the first row. Therefore, one must look at the sesamoid level in establishing the alignment in the axial or horizontal plane of the first metatarsal.
Any malreduction of the medial metatarsals will have a deleterious effect on the medial arch of the foot and foot mechanics.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

2. Patient preparation
This procedure is typically performed with the patient placed supine with the knee flexed at 90°.

3. Approaches
For this procedure, the following approaches may be used:
4. Reduction and preliminary fixation of the articular block to the shaft
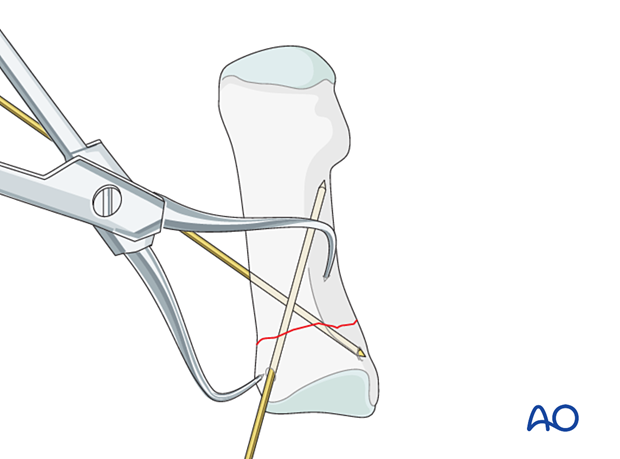
Expose the fracture ends with minimal soft tissue dissection off the bone.
Clean out the debris to allow reduction.
Reduce the fracture with the help of a reduction forceps and provisionally fix it with one or two 1.6 mm K-wires or reduction clamps.
Anticipate the plate position when placing the K-wires to avoid interference.
5. Fixation
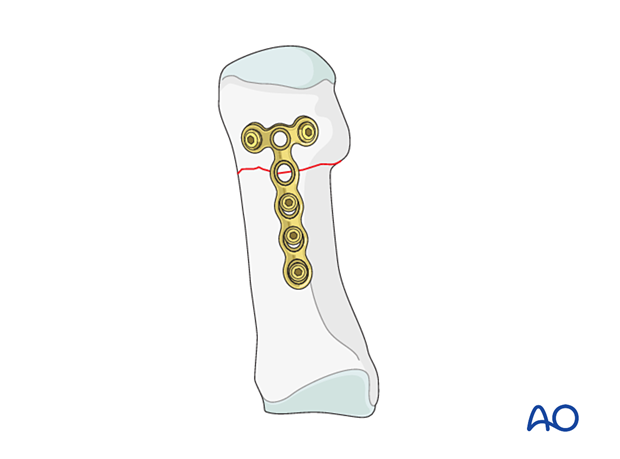
Plate selection and adaptation
As the metatarsal base is a small fragment, a 2.0 or 2.4 T-plate may be used.
A locking construct will be more stable in the setting of osteoporosis.
The plate should be long enough to allow the insertion of at least two screws in the shaft.

Bending and contouring the plate
The plate is contoured to approximate the shape of the normal dorsal surface of the proximal metatarsal.
The plate may be slightly over-bent for simple fractures to prevent gapping at the opposite cortex when tightening the screws.
The plate’s T-end must be bent to follow the convexity of the dorsal surface of the metatarsal base.
A dorsal plate will generally cause less soft tissue irritation than a medial plate for the first metatarsal. Here, we will only demonstrate the application of a dorsal plate.
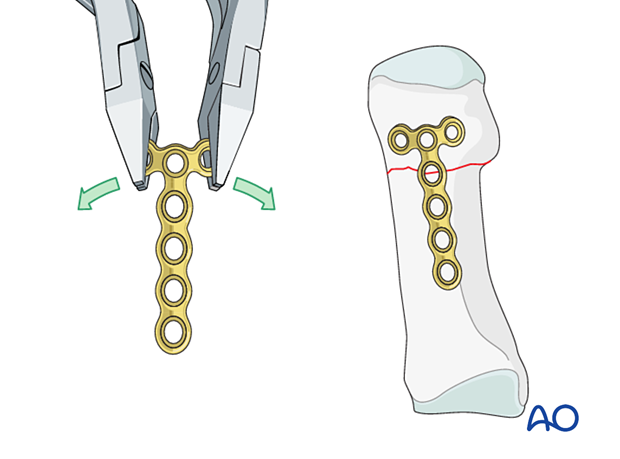
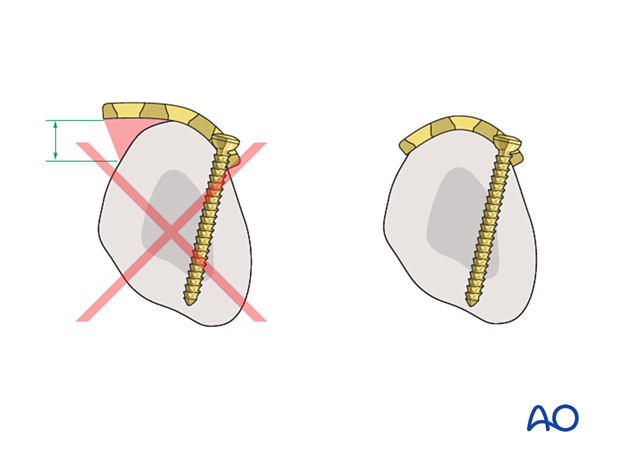
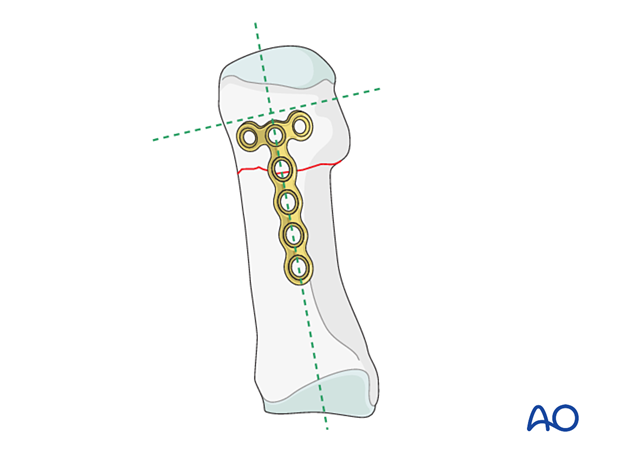
Plate application
The plate is placed distally enough from the fractured area to allow at least two screws to be inserted into the distal segment.
Ensure that the plate is centered on the long axis of the diaphysis.
Distal screw insertion
Insert the first screw but do not tighten it fully. Ensure that it engages the far cortex but does not protrude into underlying soft tissues.
Check the transverse part of the plate in relation to the metaphysis and the long axis of the bone. Insert the second screw in the opposite lug of the transverse part of the plate.
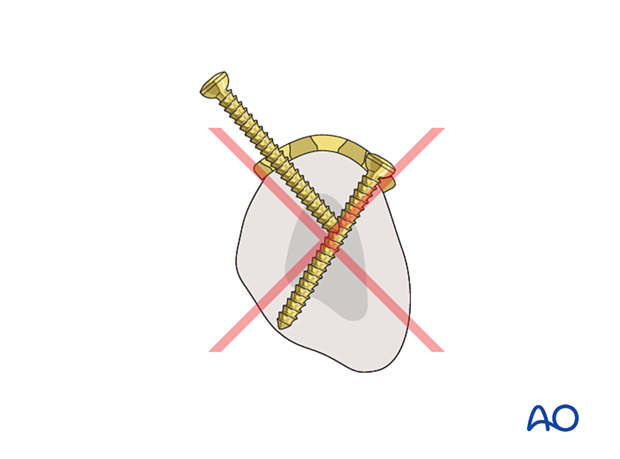
Joint penetration must be avoided.
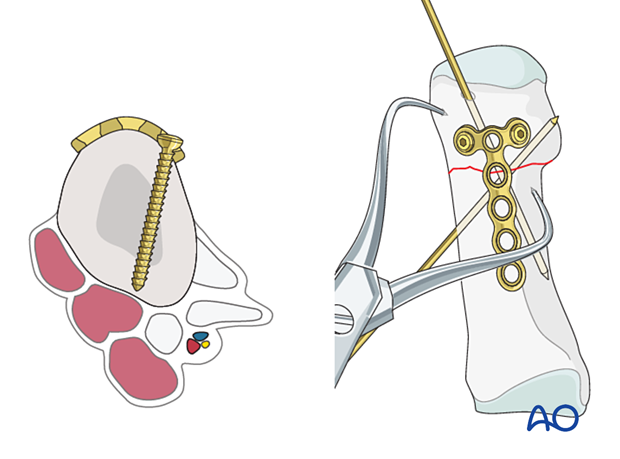
Fixation
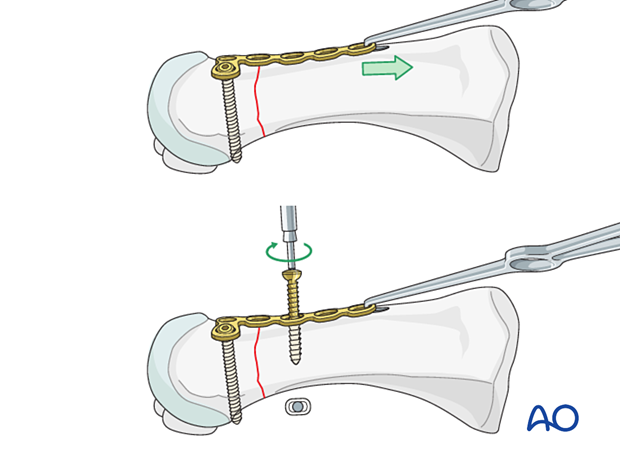
Attach a small bone hook in the distal hole of the plate and apply distal traction to the plate creating compression at the fracture site.
When applying compression, the temporary K-wires should be removed to enhance the compression effect. Use reduction forceps to stabilize the fracture.
Insert two or three bicortical screws into the distal fragment.
In osteoporotic bone, locking head screws may require a mini fragment locking plate.
6. Aftercare
An appropriate well-padded dressing should be applied to protect the surgical incision. Compression will help control swelling.
If present, the skin-pin interface should be similarly well-padded but with dressings that can be readily removed to inspect for pin site infection.
Immediate postoperative treatment is rest, ice, and elevation.
The patient should restrict weight-bearing for six weeks until signs of radiographic healing are present. After this, patients can be weight-bearing as tolerated.
Patients must exercise their ankle and subtalar joints out of the orthosis to prevent stiffness (eg, by stretching their Achilles).
X-ray the metatarsals at six weeks to confirm satisfactory union and remove K-wires if present. Once the fracture is united, the orthosis may be gradually discontinued.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid- and hindfoot.
If the gastrocnemius muscle has been released, a splint or cam walker can be used to protect the surgical site.













