Locking plate with/without lag screw
1. General considerations
Strategy options for complete articular fractures
The principle of this procedure is first to reduce and fix the articular block. Anatomical reduction of the joint surface is essential to prevent chronic instability or posttraumatic degenerative joint disease. The articular block is then fixed to the shaft using a plate.
An alternative strategy is to simultaneously reduce and temporarily fix all components of the fracture, followed by definitive fixation. Typically the definitive fixation would start with screw fixation of the articular block.
Anatomical considerations
Proper alignment of the metatarsal heads is a critical goal in restoring the forefoot mechanics.
A normal curved “cascade” (Lelièvre’s parabola) appearance, which is symmetric with the other foot, is mandatory on the AP view. See illustration. This symmetry ensures that the normal length of the metatarsal is restored.
It is also critical to restore the metatarsals in their axial or horizontal plane so that all the metatarsal heads are on the same level in the axial view.
Any malalignment, particularly flexion, will recreate focally high pressure during the stance phase and toe-off, resulting in pain and subsequent callus formation.
The sesamoids, rather than the first metatarsal head, bear weight in the first row. Therefore, one must look at the sesamoid level in establishing the alignment in the axial or horizontal plane of the first metatarsal.
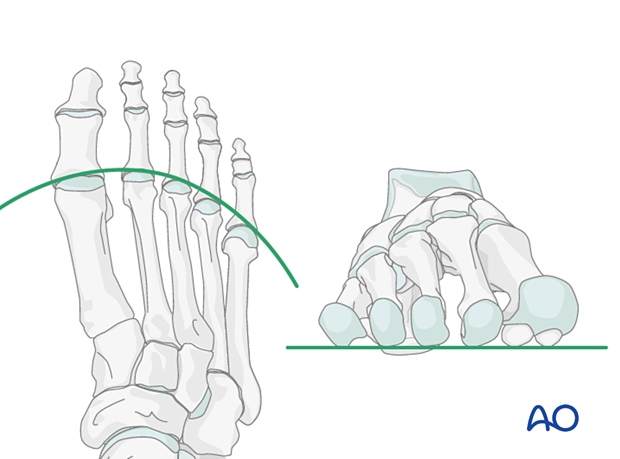
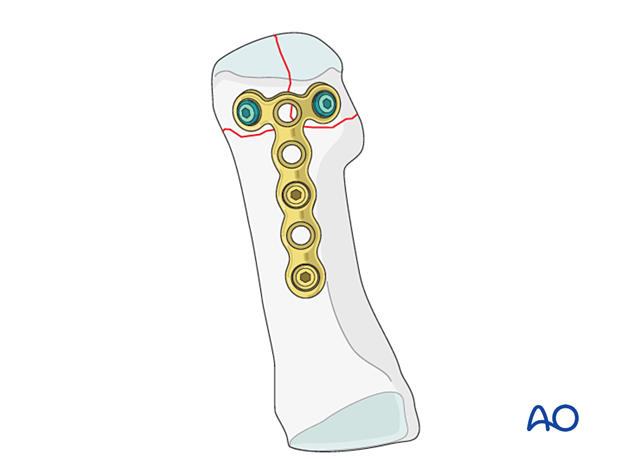
Plate placement on the first metatarsal
Depending on the fracture pattern of the first metatarsal, the plate can be applied medially or dorsally to allow lag screw insertion through the plate, perpendicular to the fracture plane.
As a dorsal plate will cause less soft tissue irritation than a medial plate, some surgeons prefer dorsal plate application.
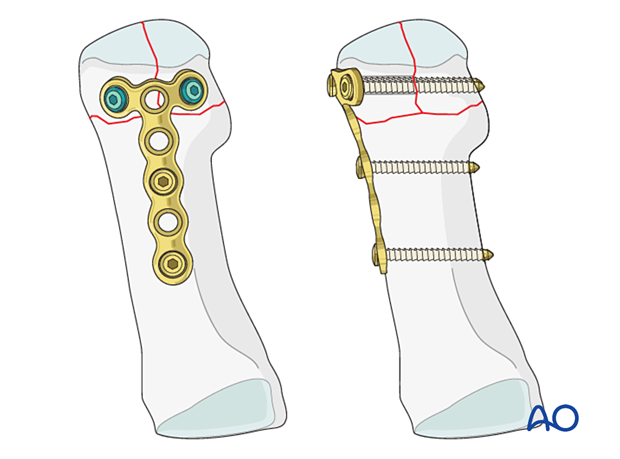
This illustration shows dorsal and medial plating for a complete articular fracture of the first metatarsal, where the articular component is in the sagittal plane.
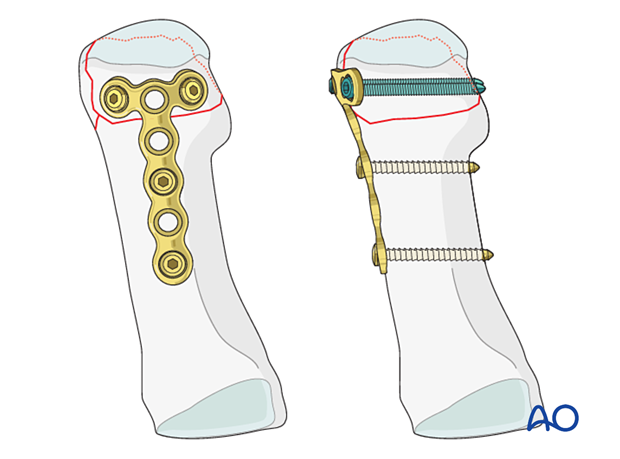
This illustration shows dorsal and medial plating for a complete articular fracture of the first metatarsal, where the articular component is in the coronal plane.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

2. Patient preparation
This procedure is typically performed with the patient placed supine with the knee flexed at 90°.

3. Surgical approach
Fractures of the first metatarsal can be approached through a medial or a dorsal approach:
4. Reduction
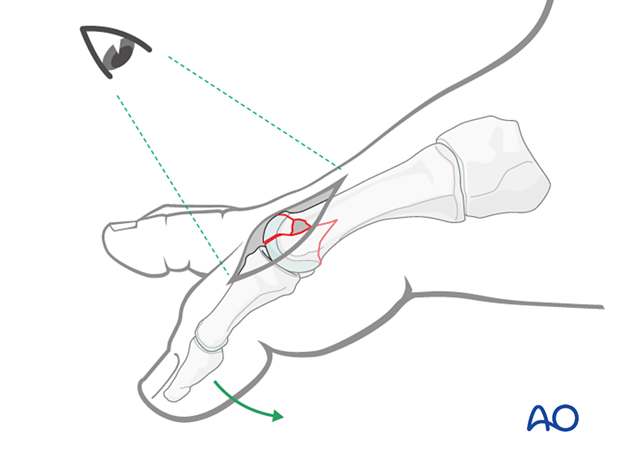
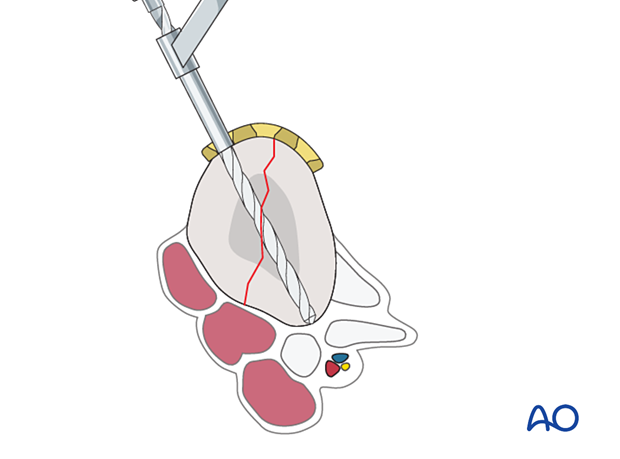
Visualization of the joint
Expose the articular surfaces.
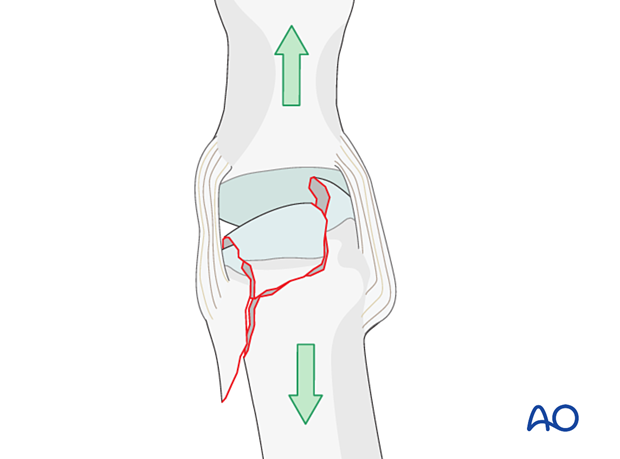
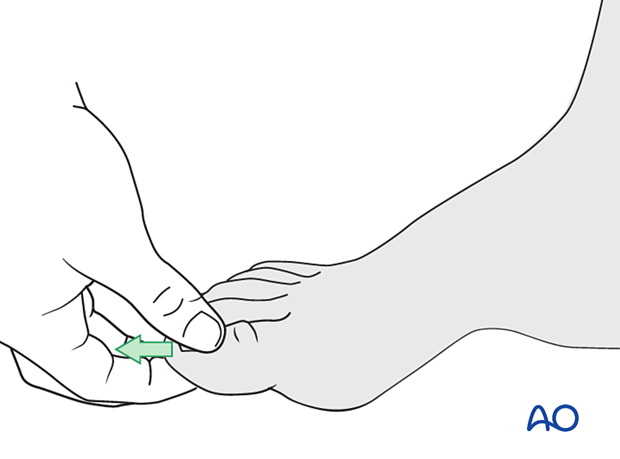
Visualization may be improved by longitudinal manual distraction.
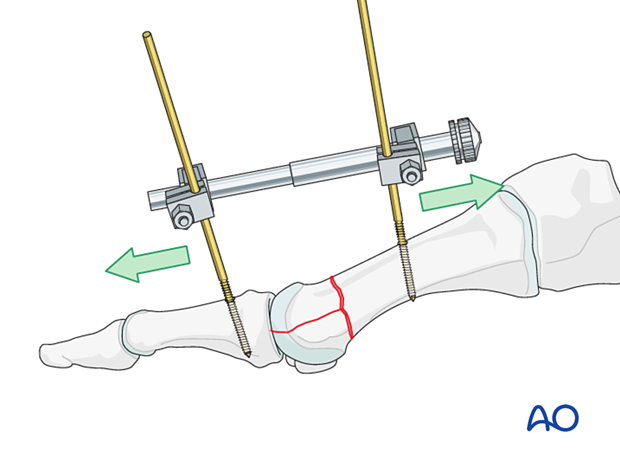
For fractures involving the first metatarsal, a mini distractor may be helpful. Visualization may be improved by releasing the dorsal insertion of the extensor hallucis brevis or extensor digitorum brevis (EHB or EDB).
The extensor hallucis longus should be preserved.
Irrigation
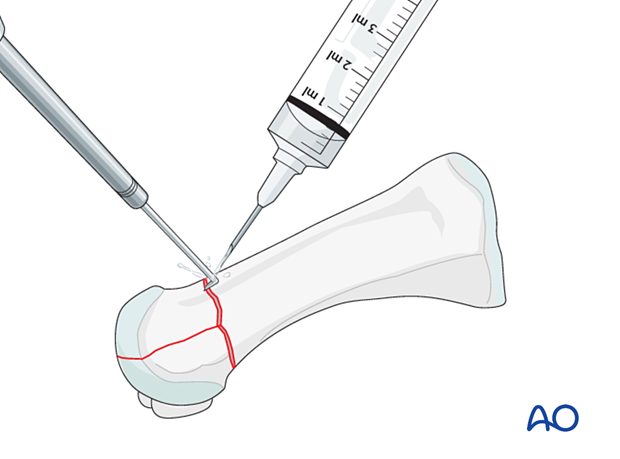
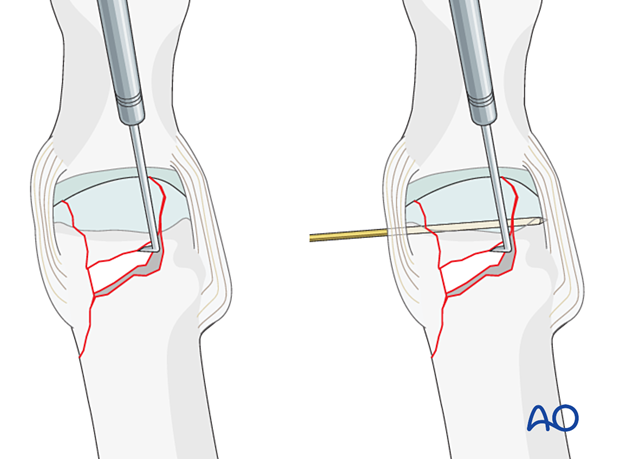
Clean the fracture using a dental pick. Direct suction or irrigation is helpful.
The fracture edges are exposed, and the fragment mobility is assessed. Take great care to avoid further fragmentation. It is essential to maintain the vascularity of small fragments.
The extent of articular involvement is assessed, including separate osteochondral fragments.
If reconstruction of the articular surface is not feasible, a joint fusion should be considered for the first metatarsal.
A fibrous union is acceptable when the joint surface is not reconstructible for metatarsals 2–5. This would be achieved by temporary pinning across the joint with the best possible reduction achieved through direct means.
Reduction
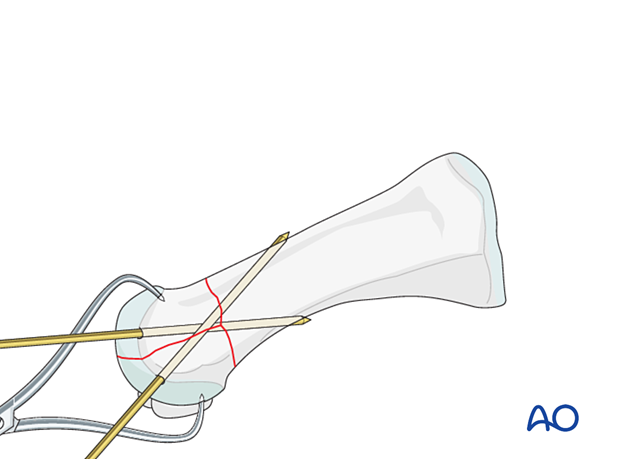
Under direct visualization, the articular fragments are manipulated using a dental pick, small K-wires as joysticks, or a small periosteal elevator.
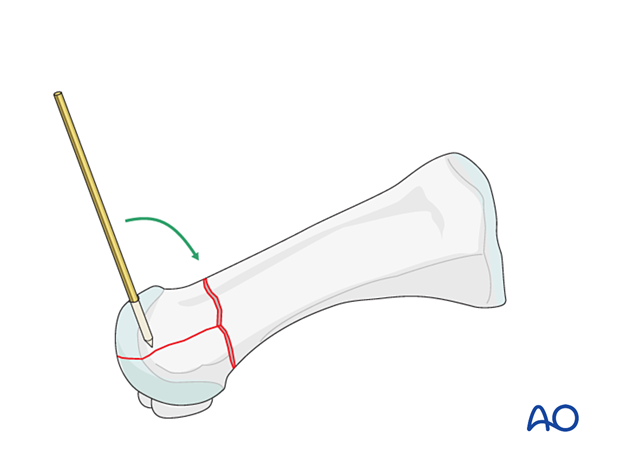
Small K-wires can be inserted across the fracture line for preliminary fixation.
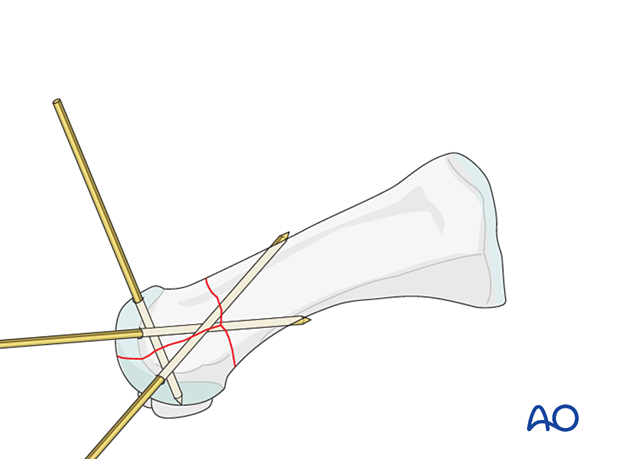
Depending on fracture configuration, pointed reduction forceps may be used for reduction and preliminary fixation.
Be careful not to apply excessive force as this can lead to fragmentation. If possible, apply the reduction forceps so that the forces created by the forces are at right angles to the fracture line. This forceps placement helps in reducing the fracture and in applying compression.
Reduction of impaction
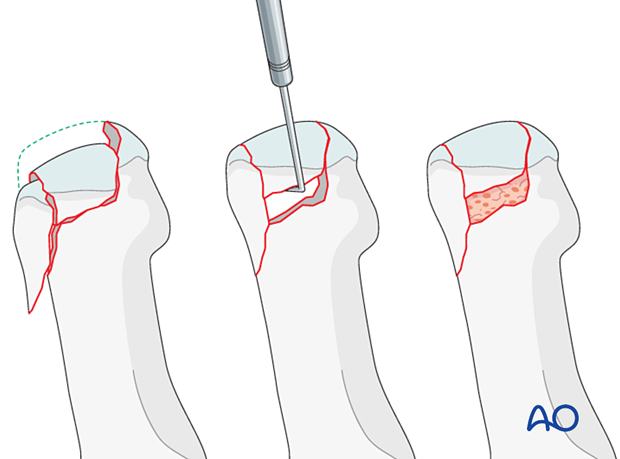
PrincipleCentrally impacted fragments in compression fractures are devoid of soft-tissue attachments and are therefore not reducible by ligamentotaxis.
Direct reduction is necessary.
The key to fixing compression fractures is restoring the joint surface to as close as normal as possible and supporting the reduction with bone graft and internal fixation.
Using a K-wire, or dental pick, the fragments are disimpacted and pushed towards the opposing bone, which is used as a template to ensure congruity of the articular surface.
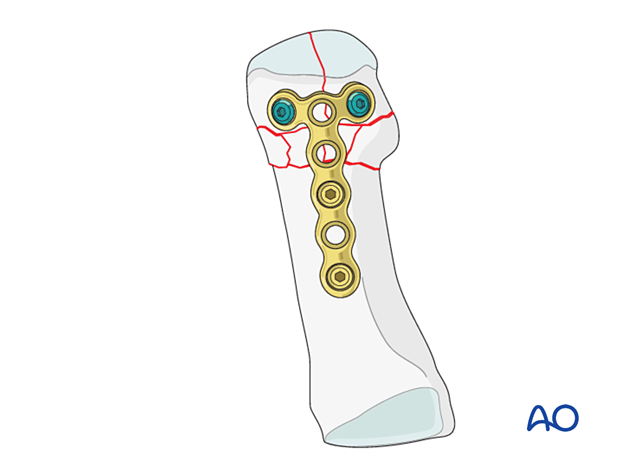
Since the metaphyseal cancellous bone is impacted, a void may be created by its disimpaction.
This void jeopardizes the fracture in two ways:
- It is a very unstable situation in which the articular fragments may easily displace (collapse)
- The healing process is delayed
The bony defect under the fragments is filled with cancellous bone graft. The bone graft also helps keep the fragments in place when the screw fixation is performed.
Visual inspection of the reduction
Anatomical reduction of the joint surface must be checked under direct visualization and image intensification.
Maximally flex the MP joint to gain a view of the plantar aspect of the metatarsal head.
The metatarsal head must not be plantarflexed once the final reduction is achieved.
Length, alignment, and rotation must be maintained in all metatarsals and joints.
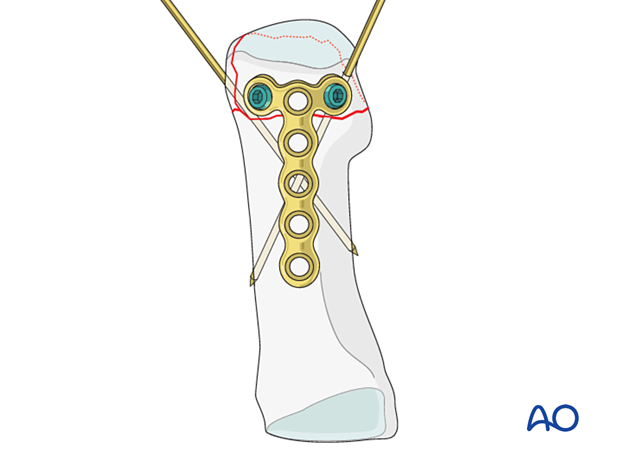
5. Fixation of the articular block using locking plate (fracture amenable to lag screw fixation)
Plate selection and contouring
A 2.0 or 2.4 T-plate is typically used. The length of the plate should allow at least two points of fixation in the shaft.
Contour the locking plate to fit the bone surface of the metatarsal.
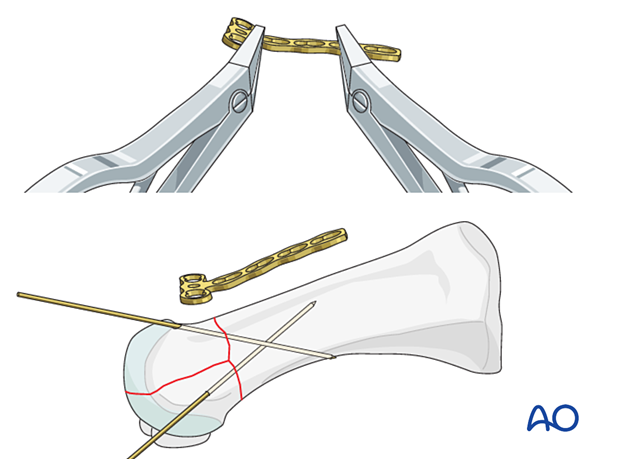
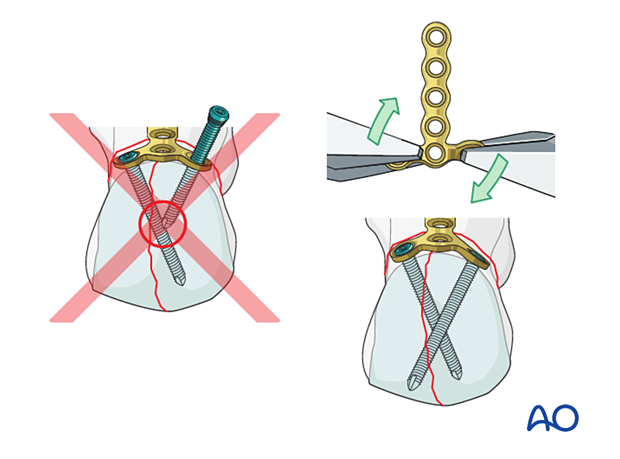
Insertion of a lag screw
The articular component should ideally be fixed and compressed using lag screws. When a locking plate is indicated, compression can be achieved using the following sequence.
Insert a lag screw either outside or through any plate hole, including the locking holes.
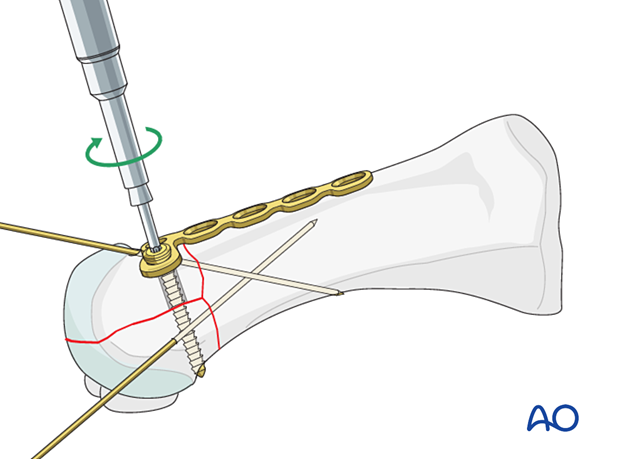
Insertion of locking head screw
Insert locking head screws into the articular block to secure the compression provided by the lag screw.
The locking head screw will also create a fixed angle between the articular block and the plate.
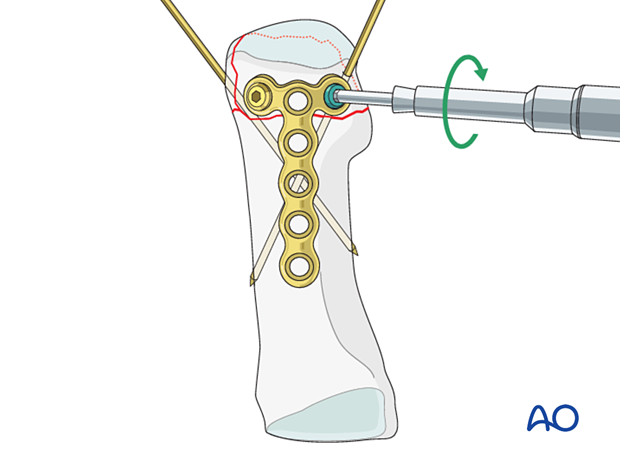
Replacement of lag screw
Replace the lag screw with a locking head screw (optional).
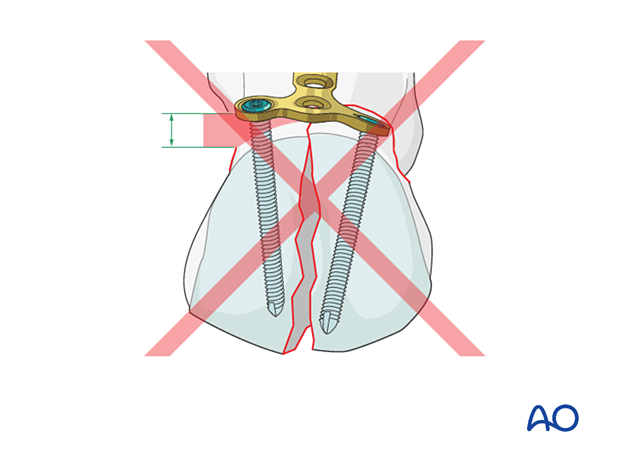
6. Fixation of the articular block using locking plate (fracture not amenable to lag screw fixation)
Manual compression of the fracture
Adjacent bones and soft tissues may prevent the insertion of lag screws. The transarticular fracture component must be compressed during the fixation of the articular block to achieve stability of the articular surface.
Ensure anatomic reduction of the intraarticular component and compress the fracture using pointed reduction forceps.
If possible, insert K-wires for temporary fixation.
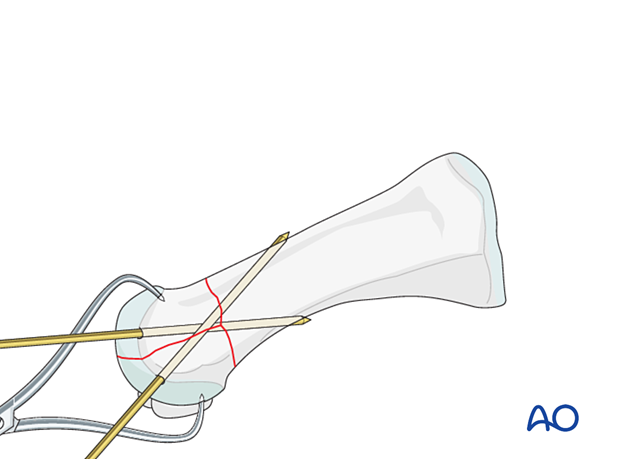
Plate selection and contouring
A 2.0 or 2.4 T-plate is typically used. The length of the plate should allow at least two points of fixation in the shaft.
Contour the plate to fit the bone surface of the metatarsal.
The plate is placed with the T-portion near the articular surface without interfering with the joint.
Ensure that the plate is centered on the long axis of the diaphysis.
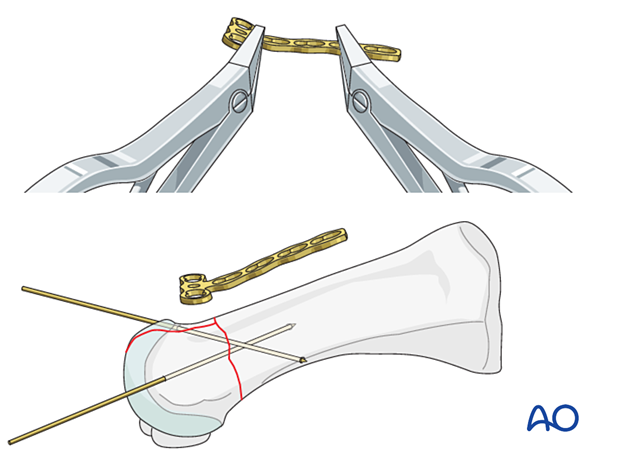
Plate fixation
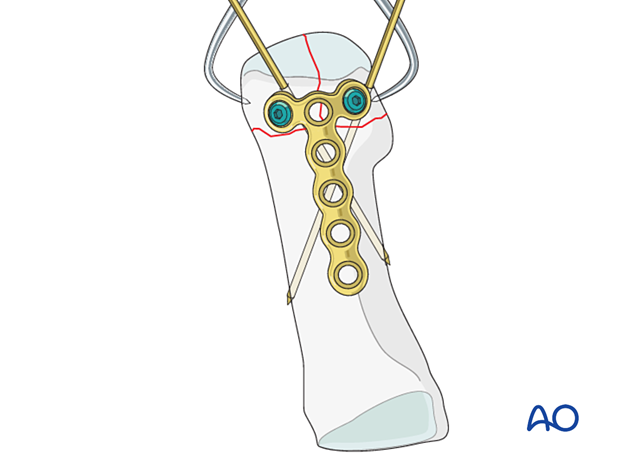
7. Reduction and fixation of the articular block to the shaft
Reduction
Reduce the articular block to the shaft and restore anatomical axial rotation, length, and angulation.
A periosteal elevator used as a lever may be helpful.
Alternatively, use a reduction forceps, dental pick, or a K-wire as a joystick as described above.
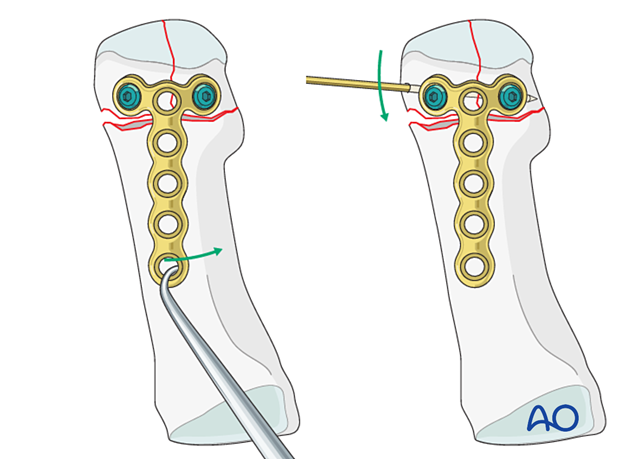
If there is any comminution in the shaft component, the fracture will shorten.
The length can be restored either by manual traction or a distractor.
A distractor will also maintain the length, whereas a manual distraction will not.
Verification of reduction
Use image intensification to confirm the reduction.
Fixation
Simple shaft fractureUse a small clamp to stabilize the fracture.
Using a small bone hook, apply traction to the plate to create compression at the fracture site before screw insertion.
Depending on bone quality, the articular block is fixed to the shaft using two 2.0 mm or 2.4 mm screws inserted in neutral mode.
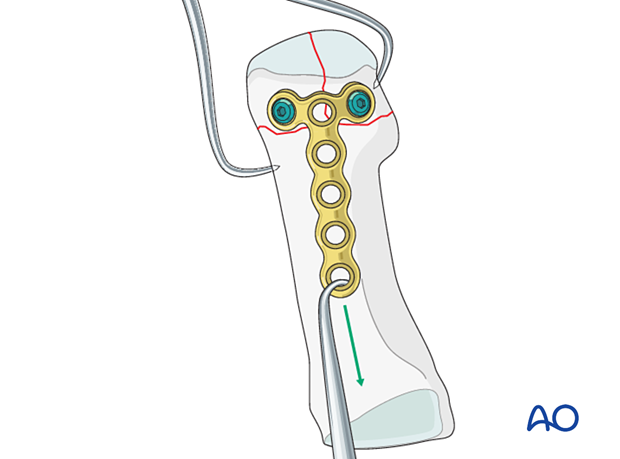
The articular block is fixed to the shaft by inserting two 2.0 mm or 2.4 mm screws inserted in neutral mode.
8. X-rays
Obtain x-rays to confirm length, rotation, angulation, and hardware placement.
Careful image intensifier review revealing flexed metatarsal heads requires revision of the reduction and fixation.
9. Aftercare
An appropriate well-padded dressing should be applied to protect the surgical incision. Compression will help control swelling.
If present, the skin-pin interface should be similarly well-padded but with dressings that can be readily removed to inspect for pin site infection.
Immediate postoperative treatment is rest, ice, and elevation.
The patient should restrict weight-bearing for six weeks until signs of radiographic healing are present. After this, patients can be weight-bearing as tolerated.
Patients must exercise their ankle and subtalar joints out of the orthosis to prevent stiffness (eg, by stretching their Achilles).
X-ray the metatarsals at six weeks to confirm satisfactory union and remove K-wires if present. Once the fracture is united, the orthosis may be gradually discontinued.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid- and hindfoot.
If the gastrocnemius muscle has been released, a splint or cam walker can be used to protect the surgical site.













