Bridge plate fixation
1. Principles
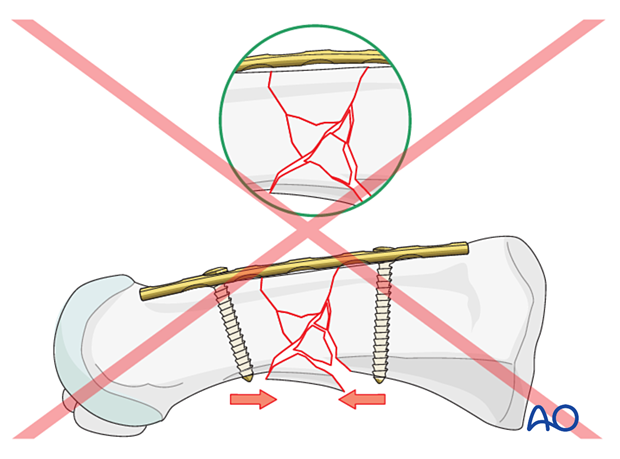
Bridge plating
The dissection required for anatomical reduction of all fragments would risk disturbing their blood supply and is not necessary. If the soft-tissue attachments of these fragments are preserved and the fragments are relatively well aligned, healing is predictable.
Anatomical considerations
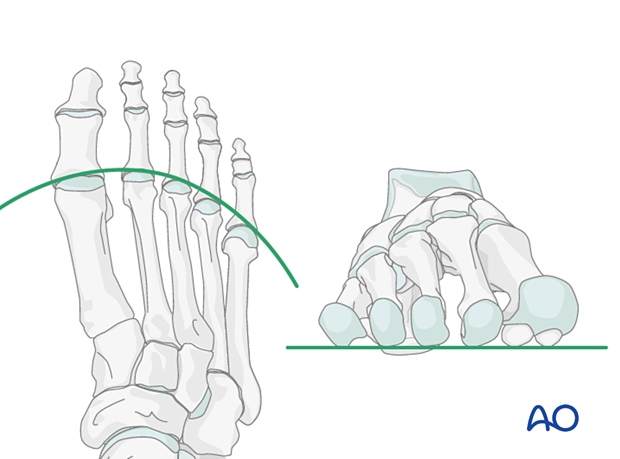
Proper alignment of the metatarsal heads is a critical goal in restoring the forefoot mechanics.
A normal curved “cascade” (Lelièvre’s parabola) appearance, which is symmetric with the other foot, is mandatory on the AP view. See illustration. This symmetry ensures that the normal length of the metatarsal is restored.
It is also critical to restore the metatarsals in their axial or horizontal plane so that all the metatarsal heads are on the same level in the axial view.
Any malalignment, particularly flexion, will recreate focally high pressure during the stance phase and toe-off, resulting in pain and subsequent callus formation.
The sesamoids, rather than the first metatarsal head, bear weight in the first row. Therefore, one must look at the sesamoid level in establishing the alignment in the axial or horizontal plane of the first metatarsal.
Any malreduction of the medial metatarsals will have a deleterious effect on the medial arch of the foot and foot mechanics.
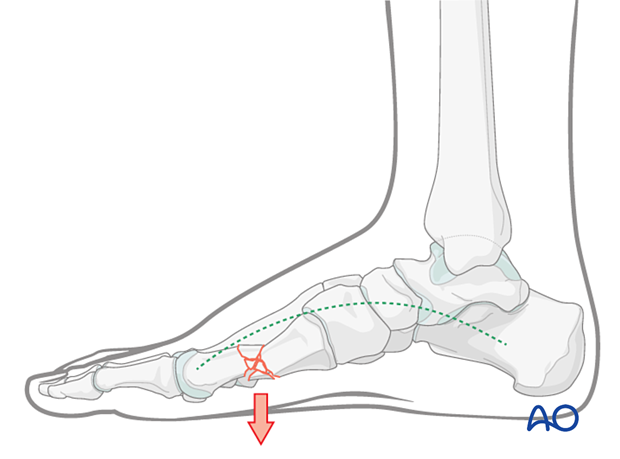
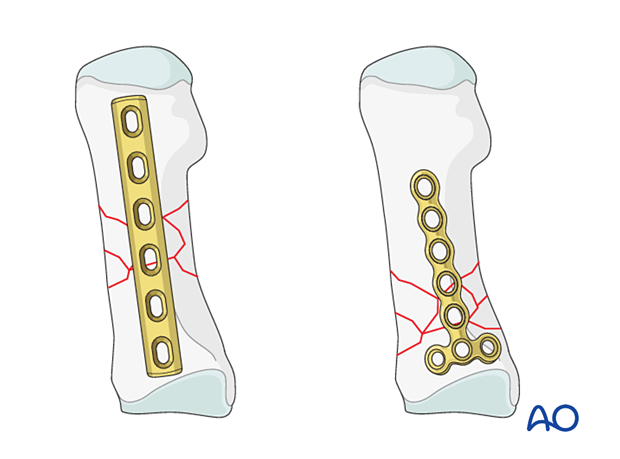
Plate selection
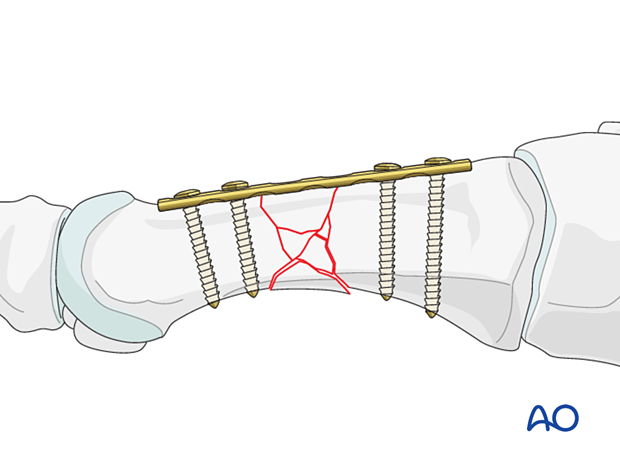
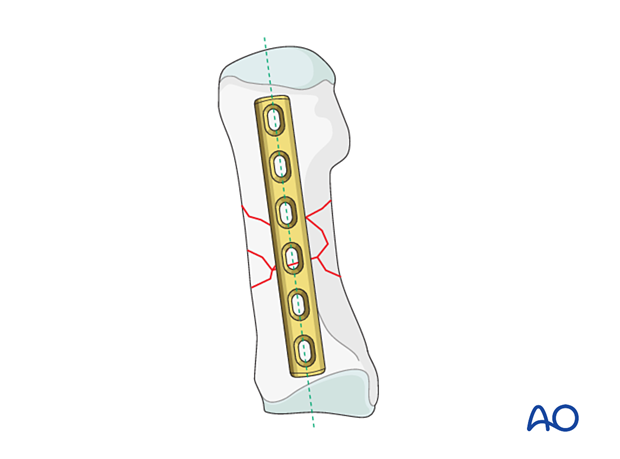
The plate should be long enough to allow two screws to be inserted in each main fragment.
For the first metatarsal, a 3.5 mm plate can be used, which allows for a minimum of two screws to be inserted in the distal and proximal segments.
For the second through fourth metatarsals, a 2.7 mm plate can be used, which allows for a minimum of two screws to be inserted in the distal and proximal segments.
A T-plate may be indicated if the fracture zone extends far proximally.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

2. Patient preparation
This procedure is typically performed with the patient placed supine with the knee flexed at 90°.

3. Approaches
For this procedure, the following approaches may be used:
4. Reduction
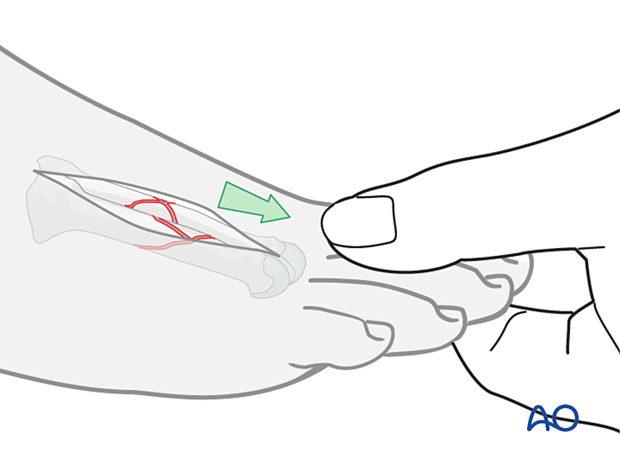
Manual traction
Manual traction on the toe, as illustrated, will usually regain the correct length, rotation, and alignment of the distal metatarsal segment.
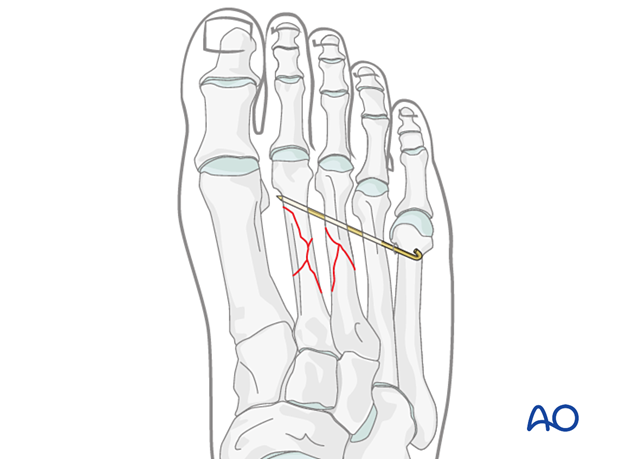
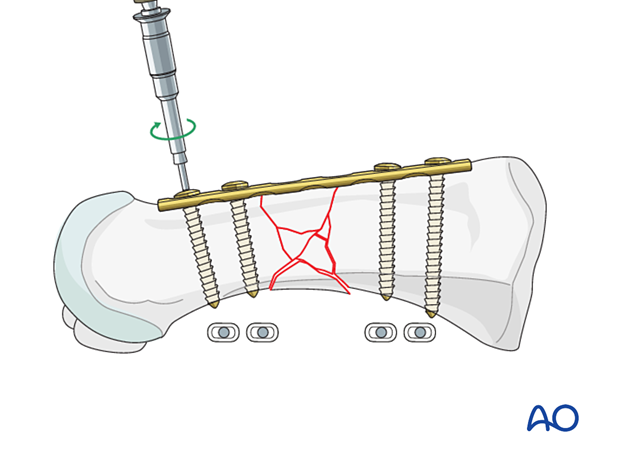
Temporary fixation
Temporary K-wires may be inserted into the adjacent metatarsals to hold the fracture out to length. The K-wire should be inserted bicortically for added stability.
As the K-wire insertion in diaphyseal bone generates significant heat, proper cooling is required to prevent bone necrosis.
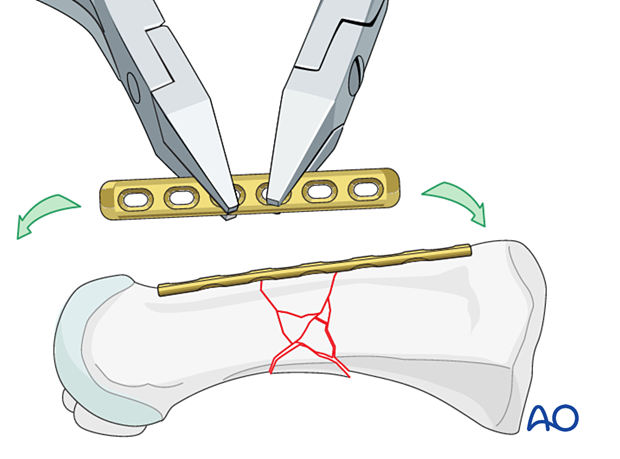
5. Plate preparation
The plate is placed dorsally onto the metatarsal.
Contour the plate to fit the surface of the metatarsal.
6. Plate fixation
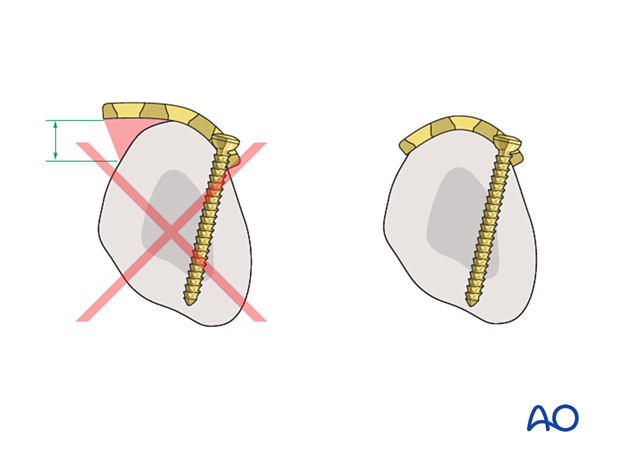
Apply the plate dorsally onto the metatarsal on its long axis. Correct rotational alignment of the distal main fragment may be challenging but is essential.
The plate is fixed by inserting screws in neutral mode.
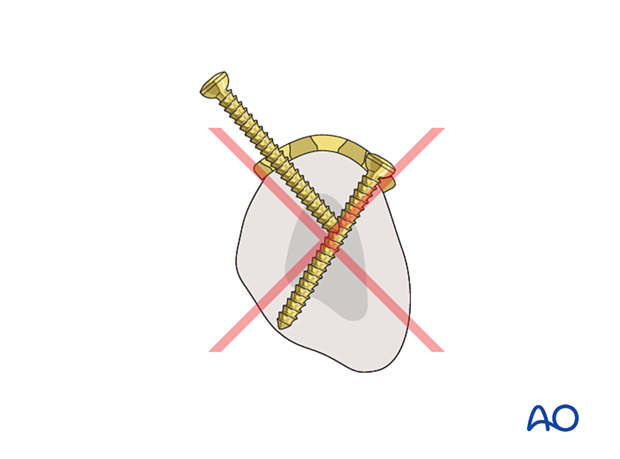
- Convergent screws inserted in the transverse portion of the plate may block each other
- Joint penetration must be avoided
7. Aftercare
An appropriate well-padded dressing should be applied to protect the surgical incision. Compression will help control swelling.
If present, the skin-pin interface should be similarly well-padded but with dressings that can be readily removed to inspect for pin site infection.
Immediate postoperative treatment is rest, ice, and elevation.
The patient should restrict weight-bearing for six weeks until signs of radiographic healing are present. After this, patients can be weight-bearing as tolerated.
Patients must exercise their ankle and subtalar joints out of the orthosis to prevent stiffness (eg, by stretching their Achilles).
X-ray the metatarsals at six weeks to confirm satisfactory union and remove K-wires if present. Once the fracture is united, the orthosis may be gradually discontinued.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid- and hindfoot.
If the gastrocnemius muscle has been released, a splint or cam walker can be used to protect the surgical site.
8. Case 1
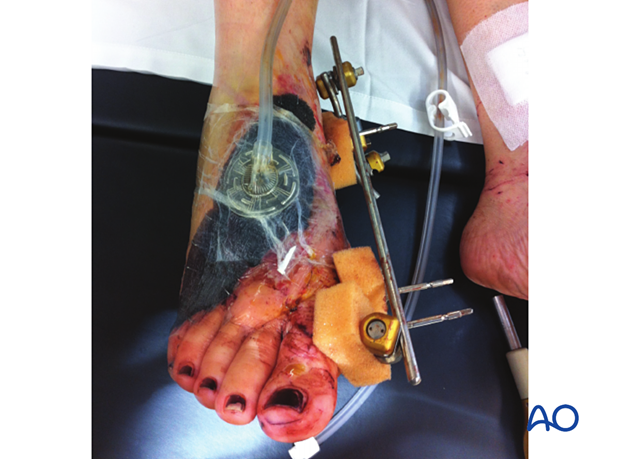
This case shows a patient who had his foot run over by a car. There are injuries to the 1st through 4th metatarsals, with an open dorsal soft tissue wound.

Lateral view

The open wound was debrided, and a spanning external fixator was applied for temporizing during the first two days.

Debridement and plating of the first metatarsal were performed in the second operation.
The 2nd–4th metatarsals aligned appropriately and did not require plating.

The soft tissue was then treated with negative pressure wound therapy and subsequent skin grafting.
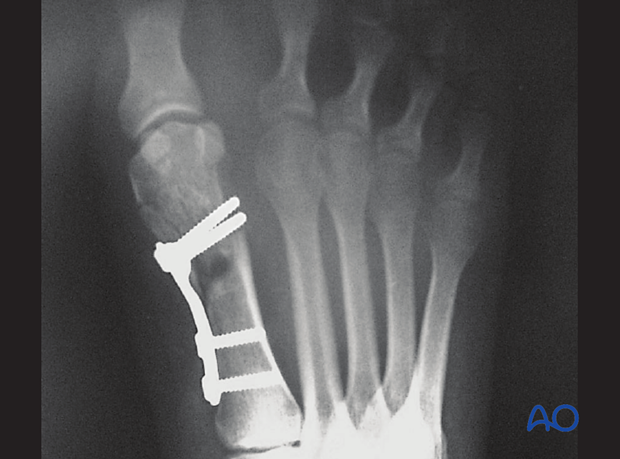
This AP X-ray shows double plating of the first metatarsal with satisfactory reduction of the 2nd–4th rays, which were treated nonoperatively.
At 6 weeks, the bone deficit of the 1st metatarsals diaphysis was grafted.

9. Case 2
This case shows an extraarticular fracture of the distal end segment of the first metatarsal.

Final fixation using a T-plate