Circular cast
1. General considerations
Preliminary remarks
Nonoperative treatment of 44B ankle injuries is usually only indicated for minimally displaced, stable fractures.
However, if the facilities and the skill for safe operative treatment are not available, nonoperative treatment is safer, and if performed correctly and skillfully, it may lead to acceptable results.
In any situation, a displaced ankle fracture should be reduced as soon as possible, even if surgery is planned for the near future as this decreases pain and swelling.
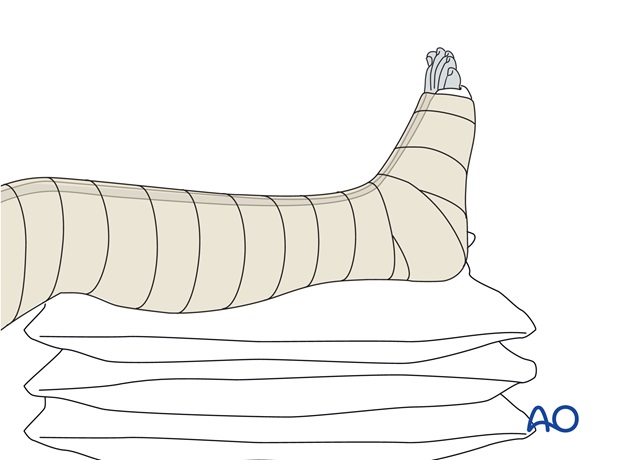
If severe swelling is present, the reduced ankle fracture should be immobilized temporarily with a plaster of Paris (POP) back-slab, and elevated on several pillows.
Anesthesia
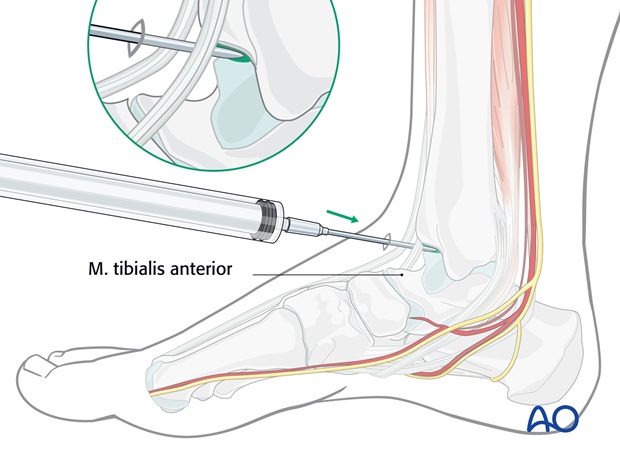
In the absence of the facility for general anesthesia, reduction can be achieved under sedation (e.g., Pethidine plus Diazepam), and/or intraarticular local anesthesia (Lignocaine 2% 15ml).
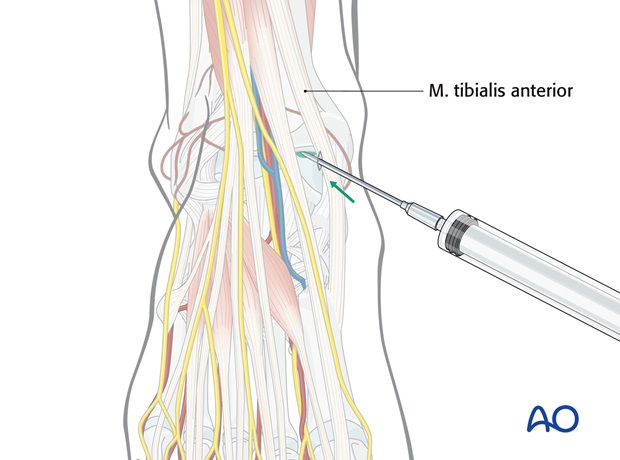
The intraarticular injection of local anesthetic is introduced anteromedially, between the tendons of tibialis anterior and extensor hallucis longus, medial to the anterior tibial neurovascular bundle.
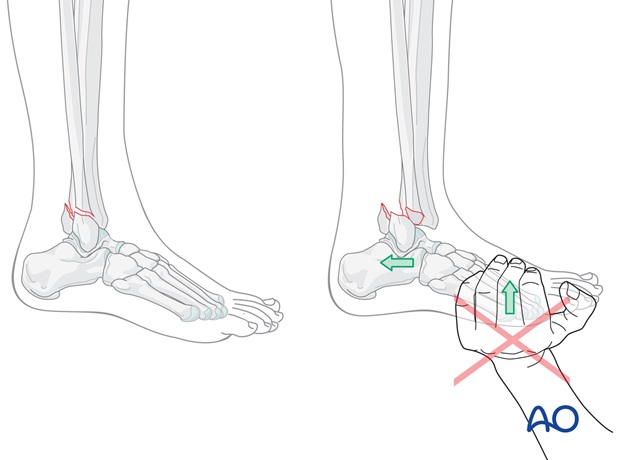
Typical displacement
The typical mechanism of injury in transsyndesmotic fractures is external rotation of the talus in the ankle mortise with the foot in supination (Lauge-Hansen supination external rotation injury), producing first a transsyndesmotic, oblique fibular fracture from distal anterior to proximal posterior. The talus then dislocates posteriorly, sometimes producing a posterior tibial fracture (Volkmann’s fragment). Finally, the medial side fails (either a deltoid rupture or a medial malleolar fracture).
Less commonly these fractures are cause by an abduction force (Lauge-Hansen abduction injury). The fracture of the lateral malleolus may be transverse or complex with some buckling of the lateral cortex.
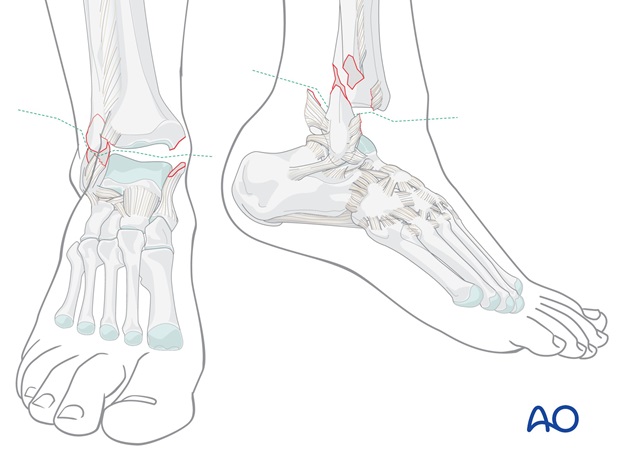
The typical clinical displacement in transsyndesmotic fractures is posterior and lateral, usually with the foot lying externally rotated.
Careful review of the x-ray images is essential for a full understanding of the injury.
Regard the injury as a two-part fracture between the lower leg (tibia and fibula) proximally, and the foot distally. The task will be to get place the foot into correct alignment with the leg.
If x-rays are not available, it is safer to correct the deformity clinically, rather than to leave it unreduced.

2. Reduction
Treatment of patients presenting early
The aim of any reduction (early or late) is to correct the displacement.
Treat the patient as soon as possible, when the deformity is typical, late swelling has not yet appeared and adequate anesthesia can be administered.
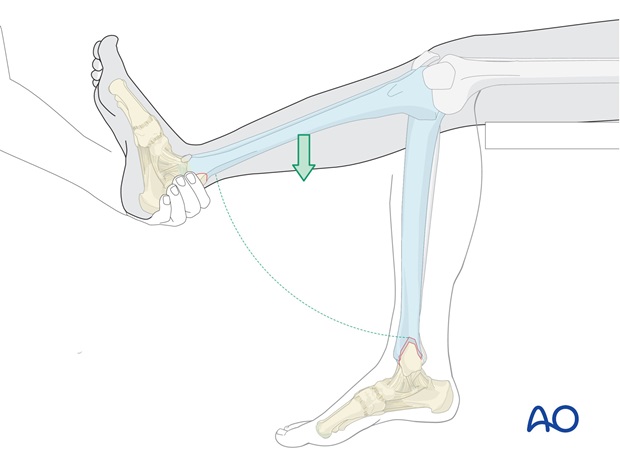
Use gravity to help to reduce the fracture.
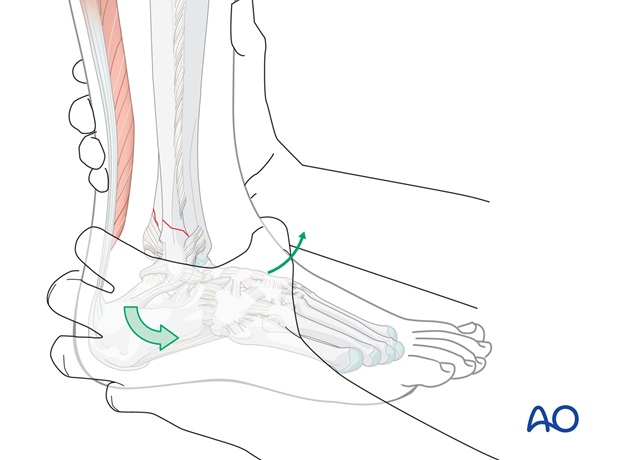
The patient lies supine on the table, with the lower leg hanging over the end of the table.
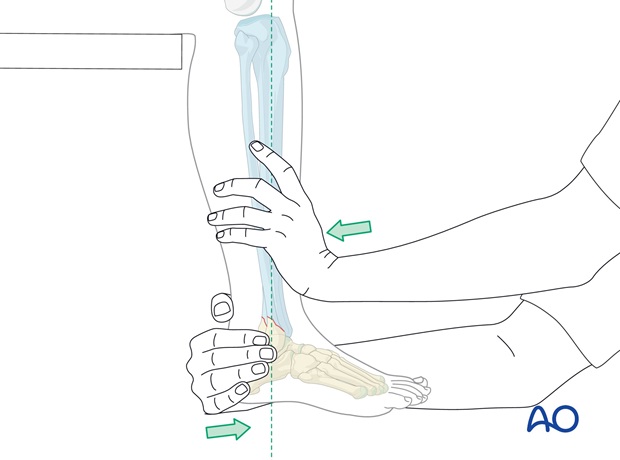
Hold the heel of the injured foot with the forefoot pointing upwards as shown and lift the externally rotated leg. In this procedure the weight of the leg will, in many cases, reduce the posterior and the lateral displacement automatically. If the mechanism of injury was external rotation of the foot relative to the leg, internally rotating the foot relative to the leg should reduce the fracture. Further pressure against lateral malleolus is usually unnecessary.
If the mechanism of injury was abduction, adducting the foot should reduce the fracture.
Treatment of patients presenting late
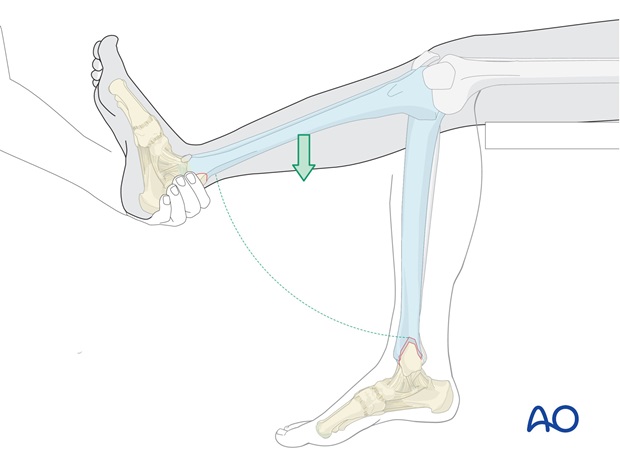
If the patient presents late and there is no possibility to administer general anesthesia, so that the patient is not fully relaxed, but merely sedated, or has only local intraarticular analgesia, reduction will not be achieved by gravity alone.
Manual reduction is performed on the hanging leg, with the knee flexed to reduce the pull of the Achilles tendon.
Correct alignment
The aim is to bring the foot into correct alignment with the lower leg.
If x-rays are not available, this is the only alignment reference available.
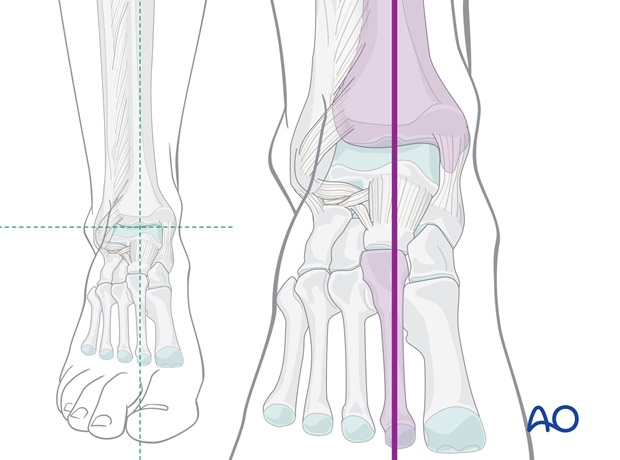
Patterns of fracture morphology
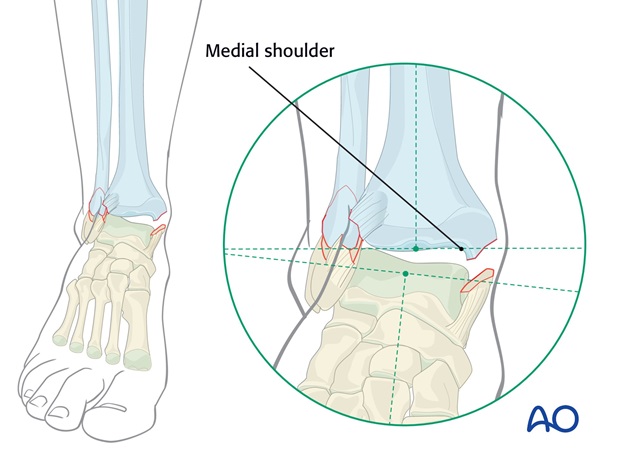
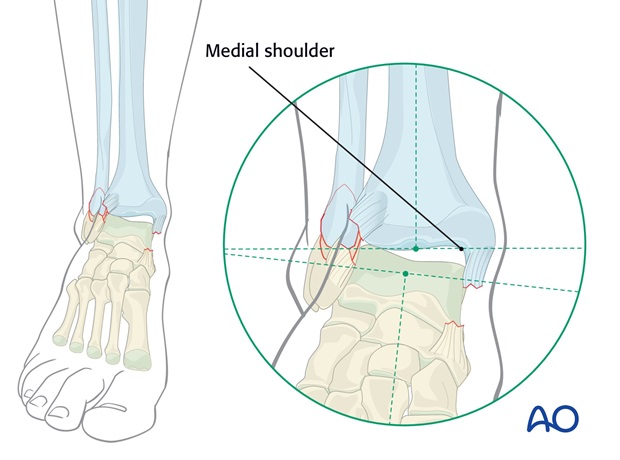
In some transsyndesmotic fractures there will be a medial shoulder.
Either the fracture of the medial malleolus has left a shoulder (or beak) on the tibia...
..., or the medial failure is a deltoid ligament rupture.
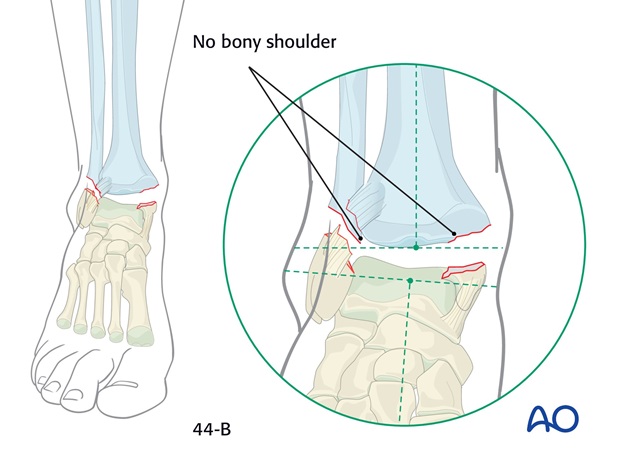
In some patterns of transyndesmotic fractures the medial malleolar fracture is flush with, or above, the joint level, and no medial shoulder remains against which to reduce the talus.
In these injuries, there is rarely a lateral (fibular) shoulder.
Reduction of fracture with a medial shoulder present
Firstly, the posterior displacement is corrected.
A plantigrade position of the foot is important, but needs to be achieved by manipulation of the hindfoot downwards, forwards and correcting any external rotation, rather than pushing upwards on the forefoot.
Avoid pushing the forefoot into dorsiflexion, as this tends to displace the talus posteriorly in the mortise. This is especially important when the fracture complex includes a posterior tibial marginal fracture (Volkmann’s fragment).
After the AP correction, the talus can be pressed against the medial shoulder, if present, by pushing the mid - and hindfoot (heel) from lateral to medial against the counterpressure of the other hand on the lower end of the tibia as shown. At the same time any external rotation deformity is corrected.
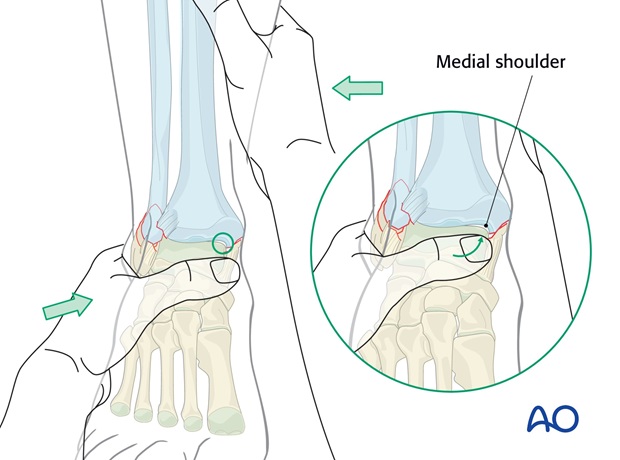
By exploiting the resistance of the medial shoulder, over-reduction should be avoided.
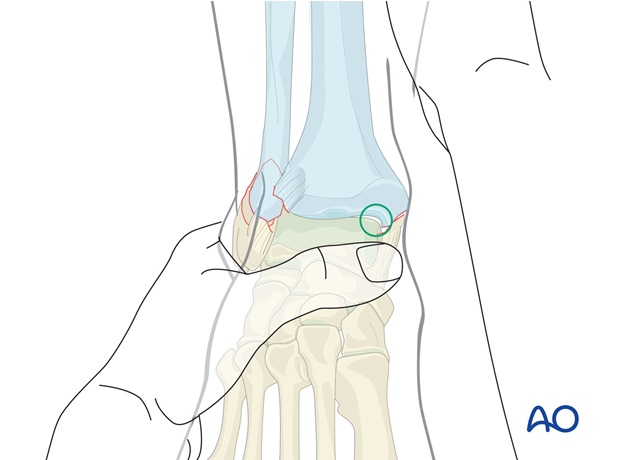
Reduction of fracture without medial or lateral shoulder
There is a danger of overcorrection of the ankle medially, although the reduced distal fibula will tend to minimize this risk. In such cases, the AP displacement is corrected, and the foot orientated in alignment with the lower leg, avoiding any undue medial pressure, and correcting any malrotation.

3. Holding the reduced position
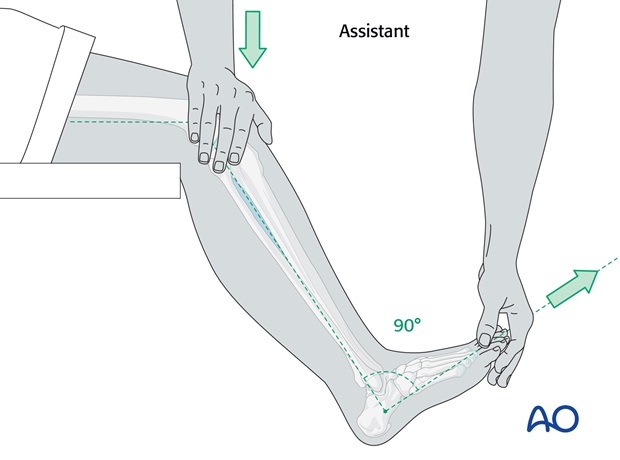
With an assistant:
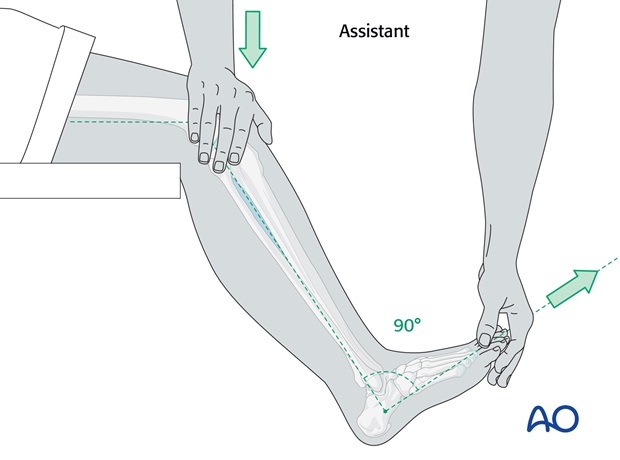
The assistant stands on the medial side of the injured leg and maintains some flexion of the knee and the right angle position of the ankle, pressing gently on the knee and holding the big toe forwards in line with the patella.
This usually holds the reduction that has been achieved and allows the operator to apply the padding and the plaster cast.
Tip: Avoid strong dorsiflexion of the foot as this can cause posterior displacement of the talus, as previously discussed.
Without an assistant:
Apply the plaster padding.
Then, apply around the ankle one roll of POP (dipped in cold water to give more time until hardening), reduce the fracture and maintain it reduced until the POP skim is hard enough to hold the reduction.
Then complete the below-knee portion of the cast.
4. Preparation for cast application
Two-person team
- Operator and assistant
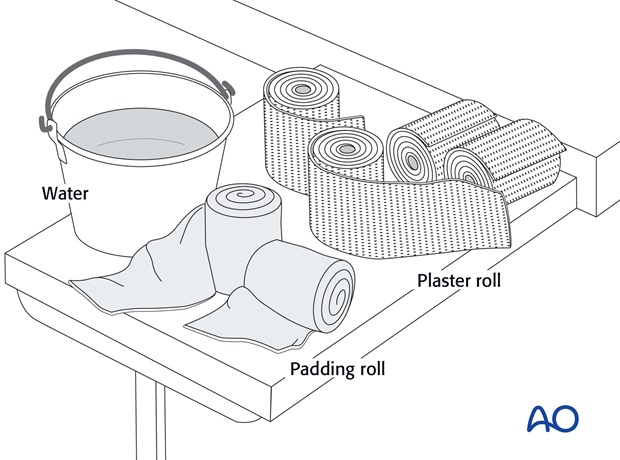
Materials (prepared before the procedure)
- 3-4 rolls 100 mm padding
- 8-9 plaster of Paris rolls, 100 mm wide
- Bucket with cold, or lukewarm, water
- Low stool
- Examination couch, or table
- Aprons to protect team members and patient
- Paper to cover the floor
5. Application of the cast
Positioning in undisplaced fractures
Fractures with injuries to both medial and lateral sides are unstable in rotation and the reduction can only be controlled by an above-knee cast.
In minimally displaced isolated transsyndesmotic lateral fractures, reduction is not necessary, and a below-knee cast will suffice.
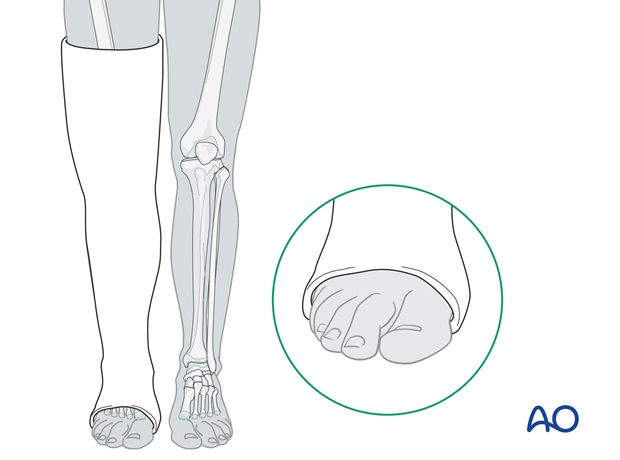
The below knee portion of the plaster cast will be applied on the hanging leg (knee flexed to 90 degrees and ankle held at 90 degrees).
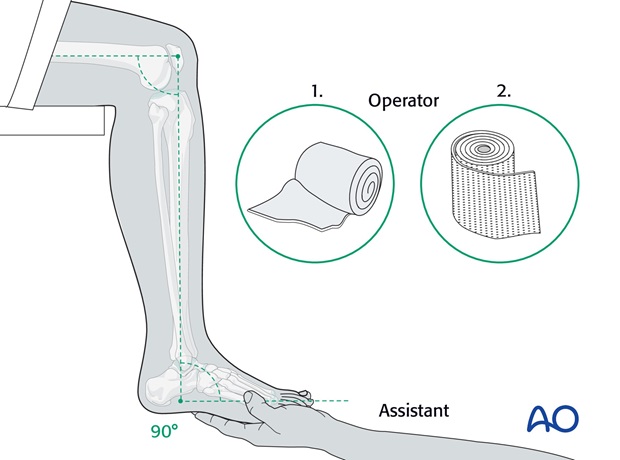
Application of the padding
First, apply the padding. This needs to be thicker over the malleoli and around the fibular head.
The cast should reach from the MTP joints of the toes to the upper thigh.
Handling of plaster bandages
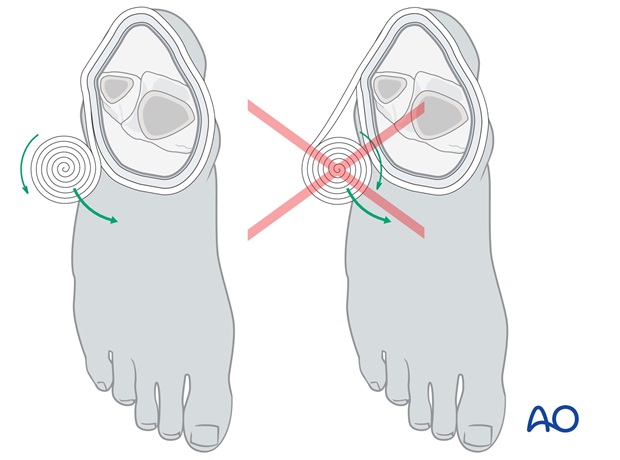
It is important to hold the plaster rolls correctly during application, so that they can be rolled on, rather than pulled on.
Application of plaster bandages
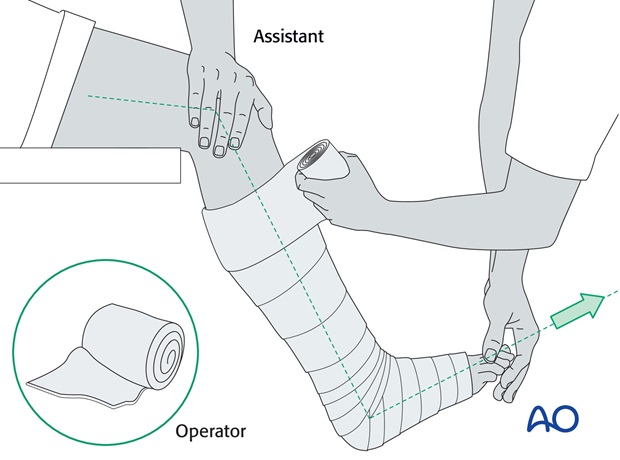
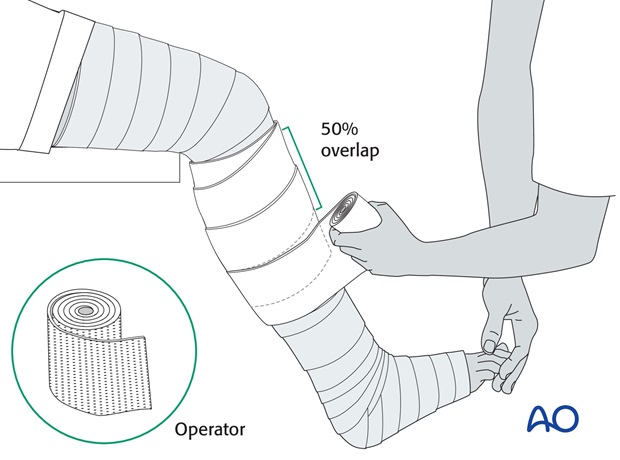
The below-knee portion of the cast is applied first.
It is easier to start proximally, overlapping by half the width of the roll and moving down the lower leg to around the ankle and foot.
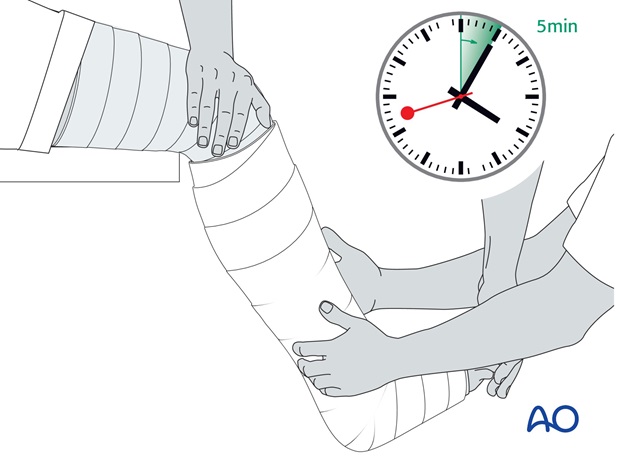
After the application of the second roll, whilst the plaster is still soft, final manipulation, with appropriate molding, is done and the reduction held until the plaster hardens. This may take 4 to 5 minutes, depending on the temperature of the water – colder water gives you more time.
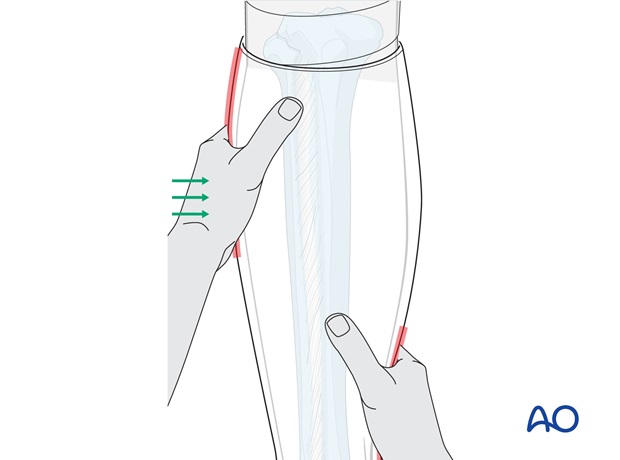
A further two rolls are then applied below the knee and further molding is performed to achieve the desired 3-point fixation.
Molding of the cast: 3-point cast fixation
When molding the cast, the same action as for reduction is repeated and held until the plaster is firm.
The principle of 3-point fixation within the cast needs to be applied. The two main molding points are created by gentle pressure over the medial hindfoot and above the lateral supramalleolar part of the lower leg.
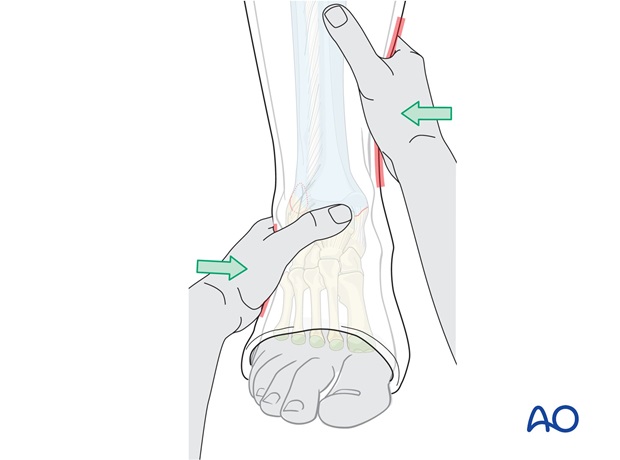
The third point is created by molding the upper end of the cast around the leg, over the medial aspect of the leg.
Application of the above-knee portion of the cast
The above-knee portion of the cast is then added. Care must be taken not to leave folds of plaster pressing into the back of the knee.
Whilst the plaster is setting the leg must be held still, if the knee moves whilst the cast is setting cracks will occur.
6. Aftercare
General guidelines
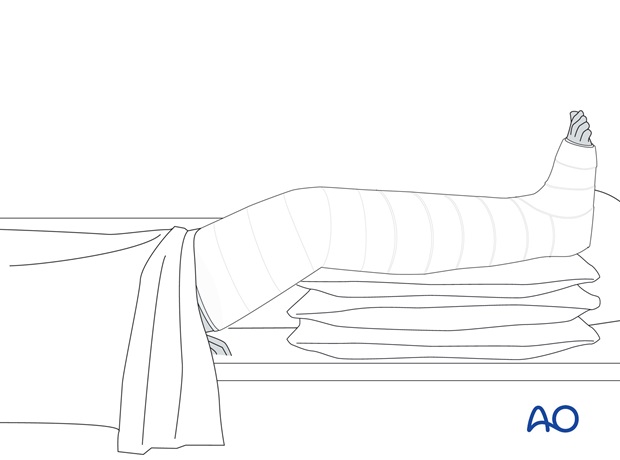
Elevate the lower leg on 2-3 pillows for 3-5 days.
X-ray control after reduction confirms the position, but must be repeated after 3-5 days. Redisplacement usually occurs during the early days, as the swelling subsides, and if diagnosed early enough, can often still be corrected non-operatively.
Analgesics and anti-inflammatory drugs should be prescribed, as necessary, during the first few weeks. If analgesia consumption is unexpectedly high, suspect redisplacement, or cast pressure on the skin.
If a cast becomes loose, it should be removed and replaced with a new one. If possible, wait until the fracture has become sticky (+/- 4 weeks) so that the reduction is not lost during the replacement procedure, but check regularly for redisplacement.
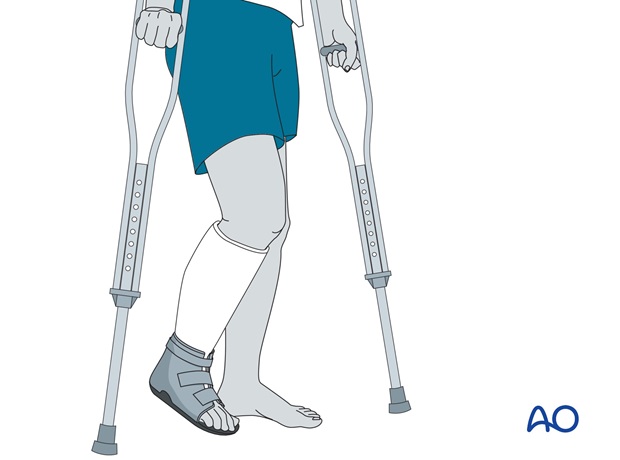
Non weight bearing should be maintained for 4-6 weeks. The above-knee cast is maintained for the first 4-6 weeks.
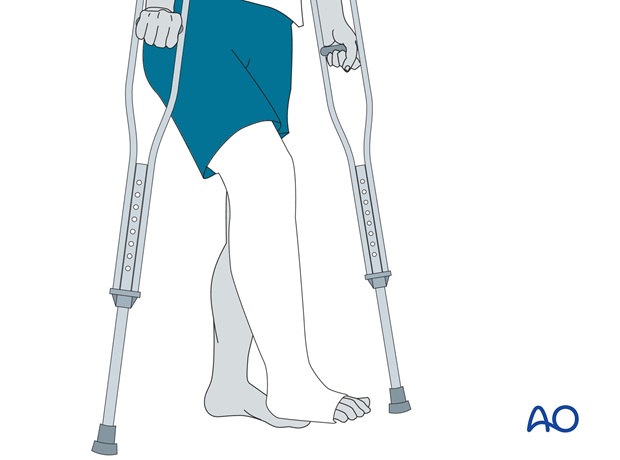
Thereafter, the cast may be changed to a below-knee cast for the remaining period of casting, as determined by the surgical decision-maker. Knee mobilization can be started.
Graduated weight bearing can begin, reaching full weight bearing by 8-9 weeks.
In fractures that required reduction, the plaster cast should not be removed before 9-12 weeks, or before the patient manages to walk pain-free with the cast. In fractures that did not require reduction, the period in the cast can be reduced at the discretion of the surgical decision-maker.
After removal of the cast, rehabilitation should involve dedicated ankle and foot mobilization for a prolonged period. At this stage, it is also advisable to give a non-steroidal anti-inflammatory preparation for several weeks.
7. Postoperative treatment of ankle fractures treated with a cast/brace
If the patient complains of severe or increasing pain, the possibility of compartment syndrome or other circulatory disorders should be considered. The cast should be split or the brace loosened. If this does not result in a rapid improvement, the cast or brace should be removed.
Mobilize the patient as soon as possible. Weight bearing is allowed in stable fractures.
Remove the plaster if the patient feels pain, and check the soft tissues for pressure sores.
If the cast loosens, it should be changed and renewed. The cast is removed after 6 to 8 weeks.
Physiotherapy is then usually necessary for 2-4 weeks.
In some patients, additional swelling occurs after removal of the cast. This can be treated with an elastic bandage, or a compression stocking.
At 3 months, if there are symptoms of lateral instability, either inversion stress x-rays or MRI can be used to investigate lateral ligament integrity.













