Long-leg circular cast
1. General considerations
Preliminary remarks
Definitive treatment of suprasyndesmotic ankle injuries with a cast is rarely indicated .
However, if the facilities and the skill for safe operative treatment are not available, nonoperative treatment is safer, and if performed correctly and skillfully, it may lead to acceptable results.
In any situation, a displaced ankle fracture should be reduced as soon as possible, even if surgery is planned for the near future as this reduced pain and swelling.
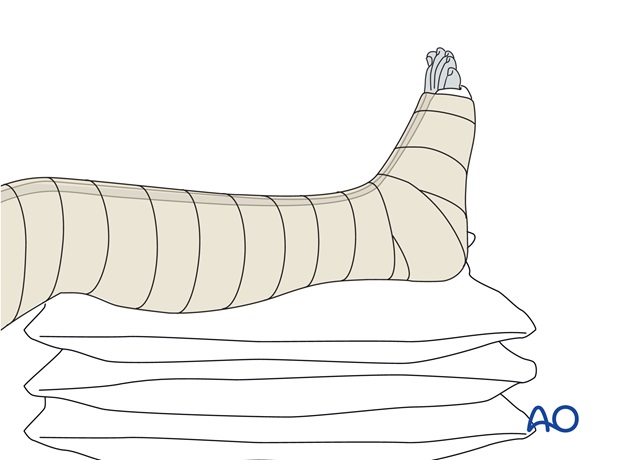
If severe swelling is present, the reduced ankle fracture should be immobilized temporarily with a plaster of Paris (POP) back-slab, and elevated on several pillows.
Anesthesia
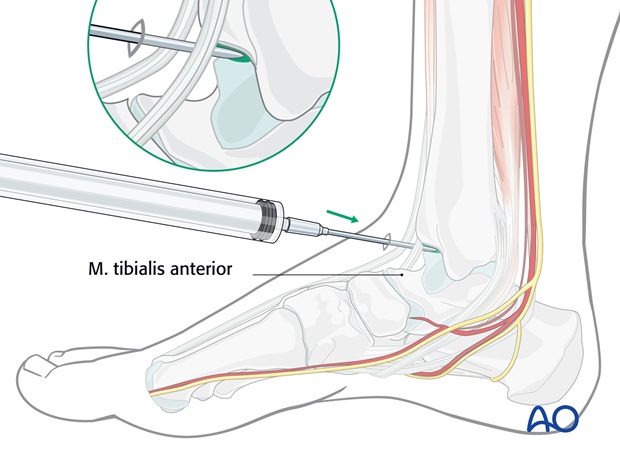
In the absence of the facility for general anesthesia, reduction can be achieved under sedation (e.g., Pethidine plus Diazepam), and/or intraarticular local anesthesia (Lignocaine 2% 15ml).
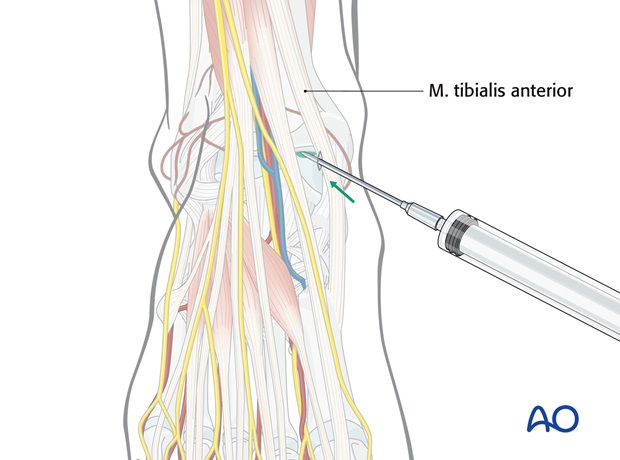
The intraarticular injection of local anesthetic is introduced anteromedially, between the tendons of tibialis anterior and extensor hallucis longus, medial to the anterior tibial neurovascular bundle.
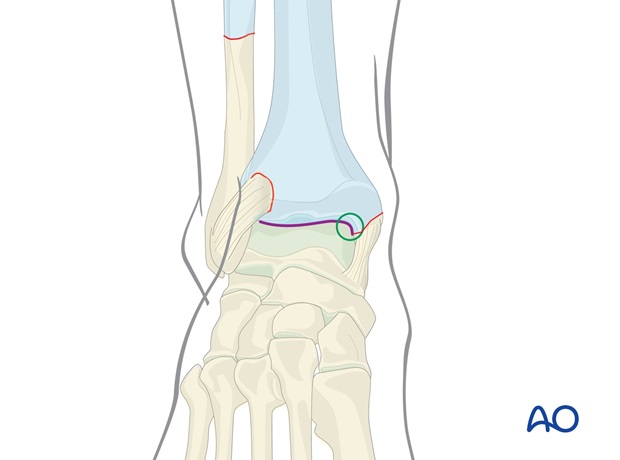
Typical displacement
Suprasyndesmotic fractures result from external rotation of the talus in the ankle mortise with the foot in pronation (Lauge-Hansen pronation external rotation injuries) causing first a failure on the medial side (malleolar fracture or deltoid rupture). The talus then rotates forwards out of the mortise, disrupting the syndesmosis and applying a twisting force to the fibula which then fractures above the level of the syndesmosis.
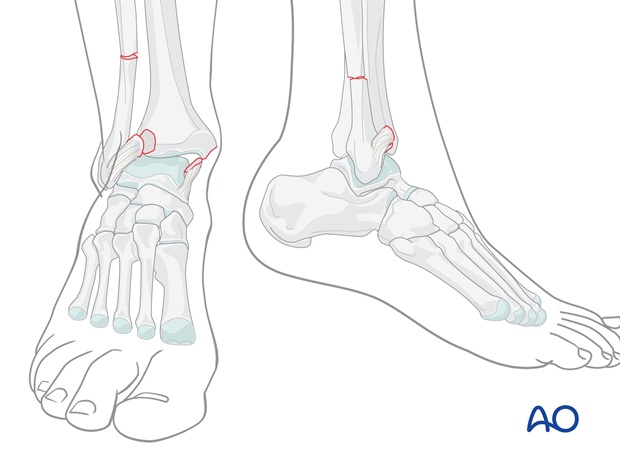
The typical displacement in suprasyndesmotic fractures is lateral, usually with the foot externally rotated. Occasionally the foot displaces secondarily into a posterior displacement.
Careful review of the x-ray images is essential for a full understanding of the mechanism of injury.
Regard the injury as a two-part fracture between the lower leg (tibia and fibula) proximally, and the foot distally. The task will be to place the foot in correct alignment with the leg.
If x-rays are not available, it is safer to correct the deformity clinically, rather than to leave it unreduced.
2. Reduction
Treatment of patients presenting early
The aim of any reduction (early or late) is to correct the displacement.
Treat the patient as soon as possible, when the deformity is typical, late swelling has not yet appeared and adequate anesthesia can be administered.
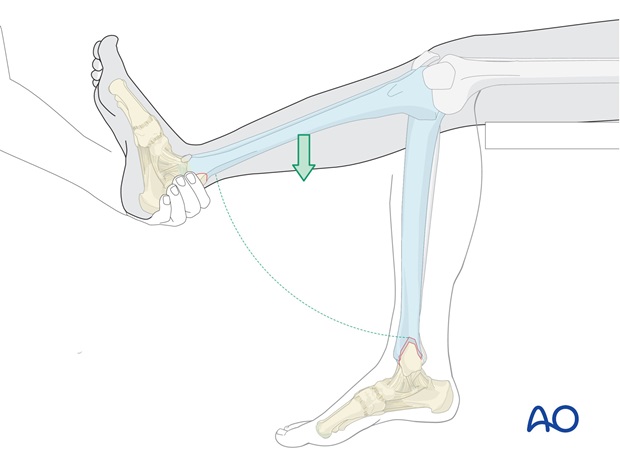
Use gravity to help to reduce the fracture.
The patient lies supine on the table, with the lower leg hanging over the end of the table.
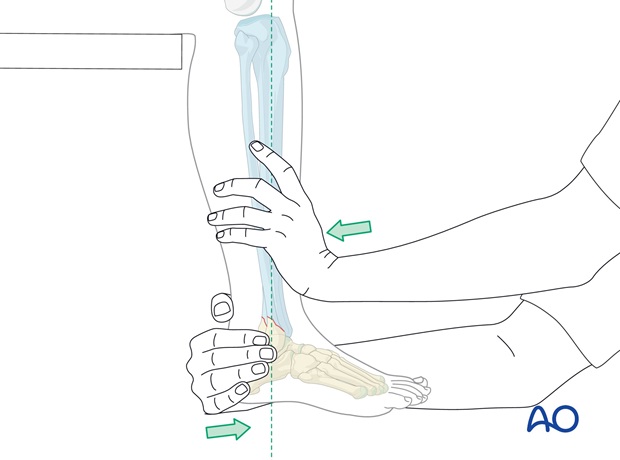
Hold the heel of the injured foot with the forefoot pointing upwards as shown and lift the externally rotated leg. In this procedure the weight of the leg will, in many cases, reduce the posterior and the lateral displacement automatically. If the mechanism of injury was external rotation of the foot relative to the leg, internally rotating the foot relative to the leg should reduce the fracture. Further pressure against lateral malleolus is usually unnecessary.
Treatment of patients presenting late
If the patient presents late and there is no possibility to administer general anesthesia, so that the patient is not fully relaxed, but merely sedated, or has only local intraarticular analgesia, reduction will not be achieved by gravity alone.
Manual reduction is performed on the hanging leg, with the knee flexed to reduce the pull of the Achilles tendon.
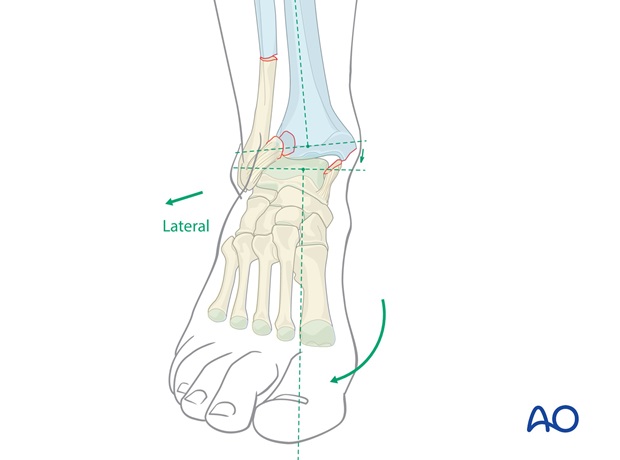
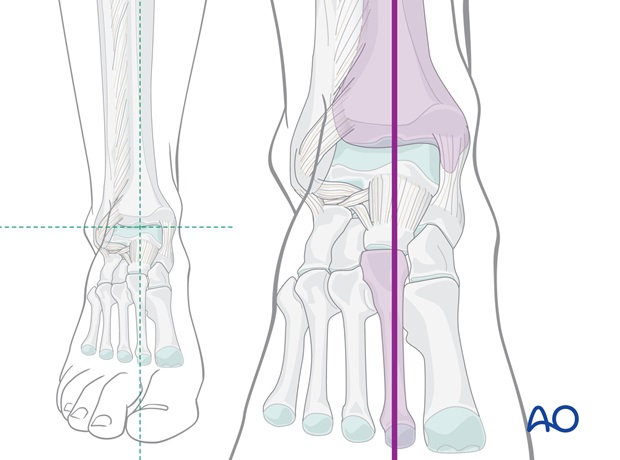
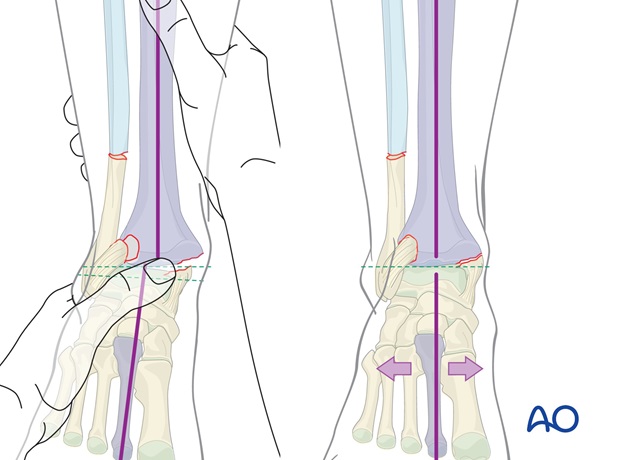
Correct alignment
The aim is to bring the foot into correct alignment with the lower leg, as shown.
If x-rays are not available, this is the only alignment reference available.
Patterns of fracture morphology
In suprasyndesmotic fractures associated with fracture of the medial malleolus, a shoulder (or beak) on the tibia usually remains, which will tend to prevent medial over-reduction.
In cases with a deltoid ligament rupture, there is a substantial medial buttress against which the talus can be reduced.
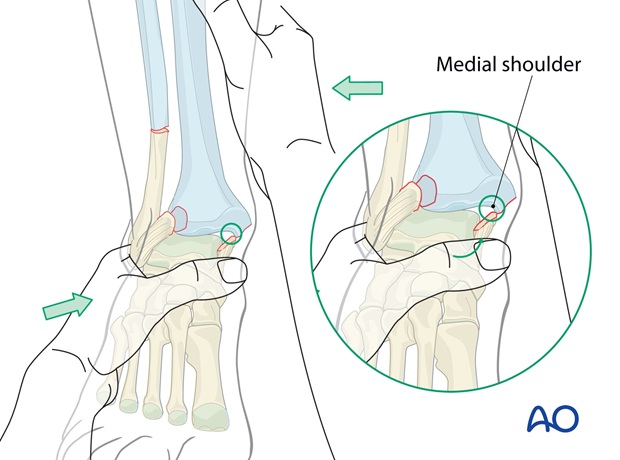
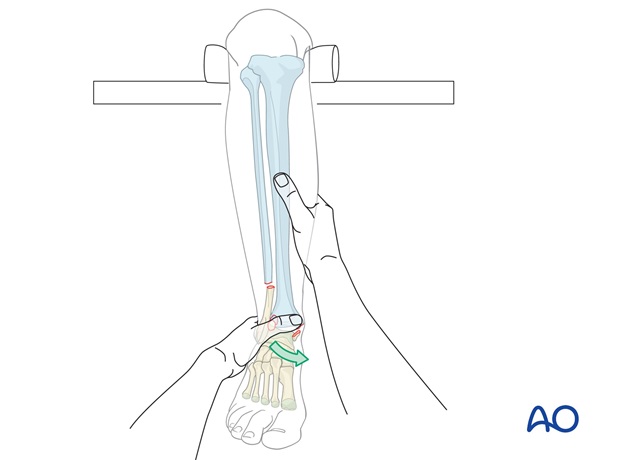
Reduction of fracture with a medial shoulder present
Any anteroposterior (AP) displacement is corrected.
Hold the hindfoot firmly and pull both distally and forwards to correct any posterior displacement.
At the same time, any external rotation displacement is reduced.

Avoid pushing the forefoot into dorsiflexion, as this may displace the talus posteriorly in the mortise, if secondary posterior displacement had occurred.
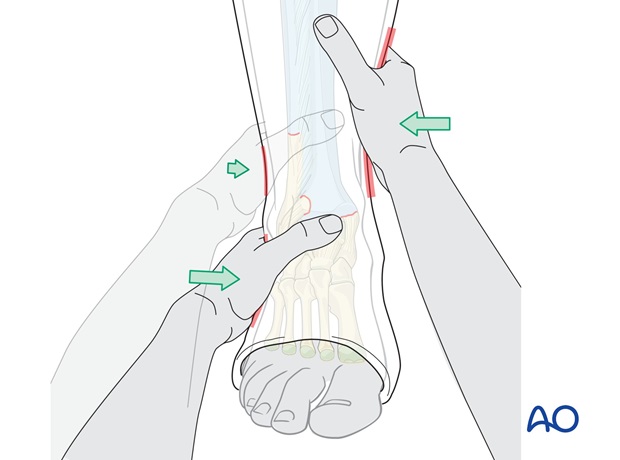
After the AP correction, the talus can be pressed against the medial shoulder, if present, by pushing the mid - and hindfoot (heel) from lateral to medial against the counter pressure of the other hand on the lower end of the tibia as shown. At the same time any external rotation deformity is corrected.
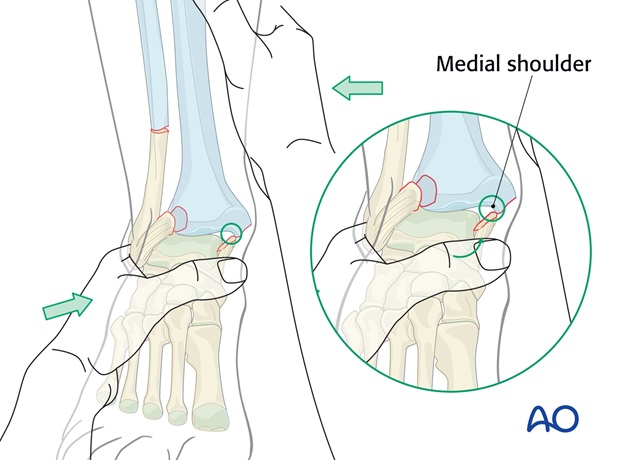
By exploiting the resistance of the medial shoulder, over-reduction should be avoided.
Reduction of fracture without a medial shoulder
In some suprasyndesmotic fractures, the medial malleolar fracture is flush with, or above, the joint level, and no medial shoulder remains, against which to reduce the talus.
The surgeon must therefore guard against medial over-reduction.
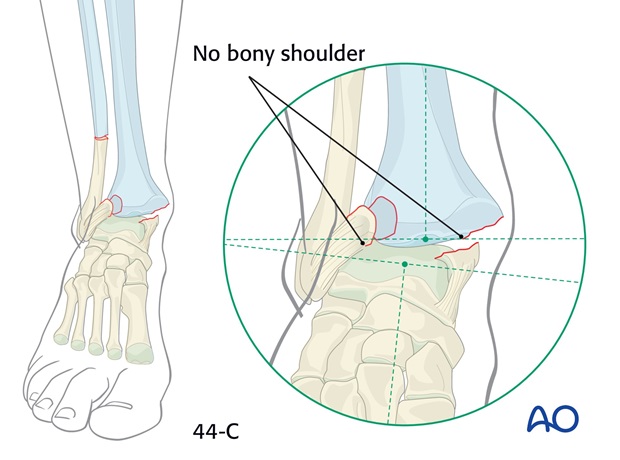
Without a medial shoulder, there is a risk of overcorrection of the ankle medially, although the reduced distal fibula will tend to minimize this possibility. In such cases, the AP displacement is corrected, and the foot then orientated in alignment with the lower leg, avoiding any undue medial pressure, and correcting any malrotation.
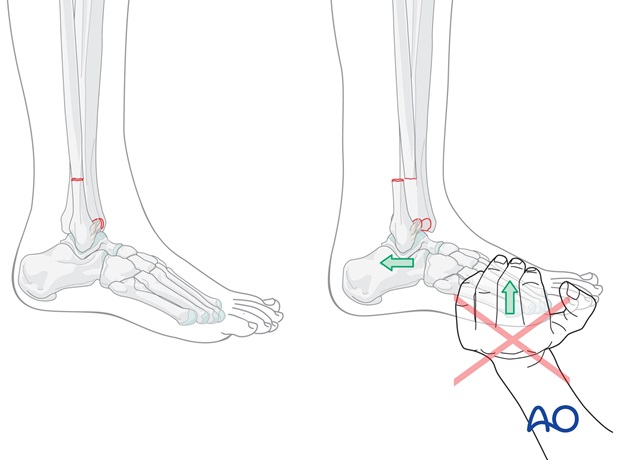
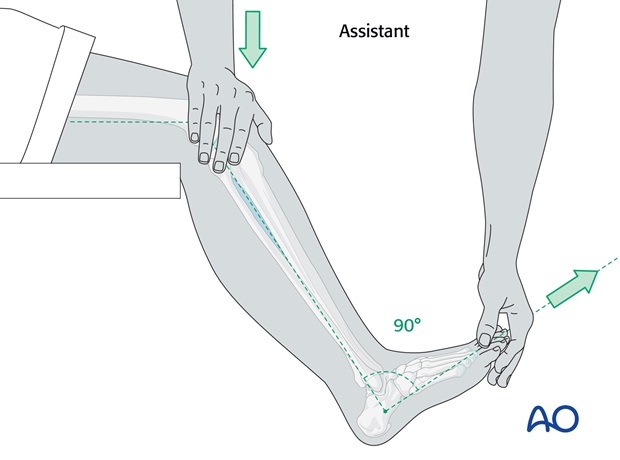
3. Holding the reduced position
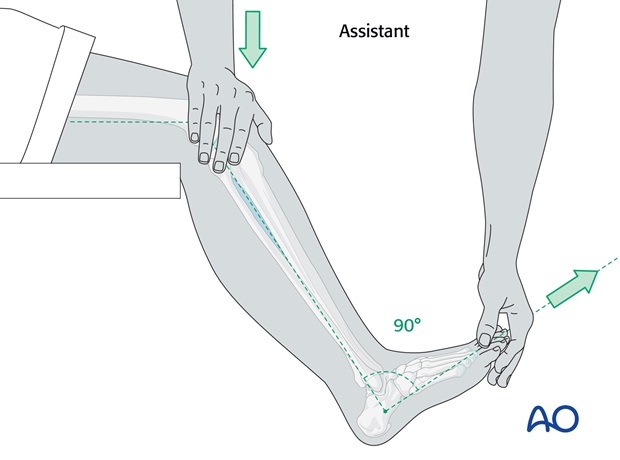
With an assistant:
The assistant stands on the medial side of the injured leg and maintains some flexion of the knee and the right angle position of the ankle, pressing gently on the knee and holding the big toe forwards in line with the patella.
This usually holds the reduction that has been achieved and allows the operator to apply the padding and the plaster cast.
Tip
Avoid strong dorsiflexion of the foot as this can cause posterior displacement of the talus, as previously discussed.
Without an assistant:
Apply the plaster padding.
Then, apply around the ankle one roll of POP (dipped in cold water to give more time until hardening), reduce the fracture and maintain it reduced until the POP skim is hard enough to hold the reduction.
Then complete the below-knee portion of the cast.
4. Preparation for cast application
Two-person team
- Operator and assistant
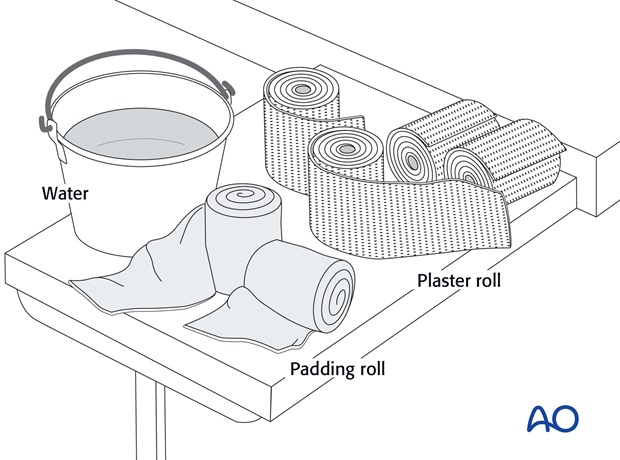
Materials (prepared before the procedure)
- 3-4 rolls 100 mm padding
- 8-9 plaster of Paris rolls, 100 mm wide
- Bucket with cold, or lukewarm, water
- Low stool
- Examination couch, or table
- Aprons to protect team members and patient
- Paper to cover the floor
5. Application of the cast
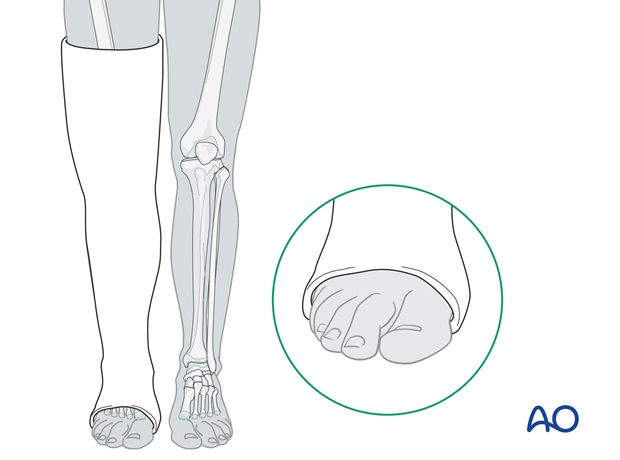
Suprasyndesmotic fractures are unstable in rotation and the reduction can only be controlled by an above-knee cast.
The below knee portion of the plaster cast will be applied on the hanging leg (knee flexed to 90 degrees and ankle held at 90 degrees).
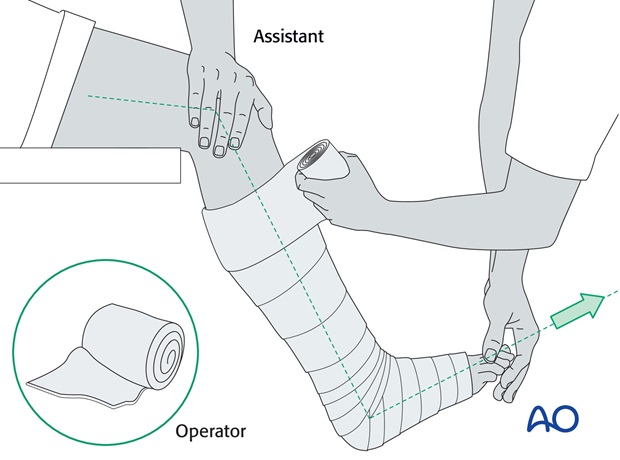
Application of the padding
First, apply the padding. This needs to be thicker over the malleoli and around the fibular head.
The cast should reach from the MTP joints of the toes to the upper thigh.
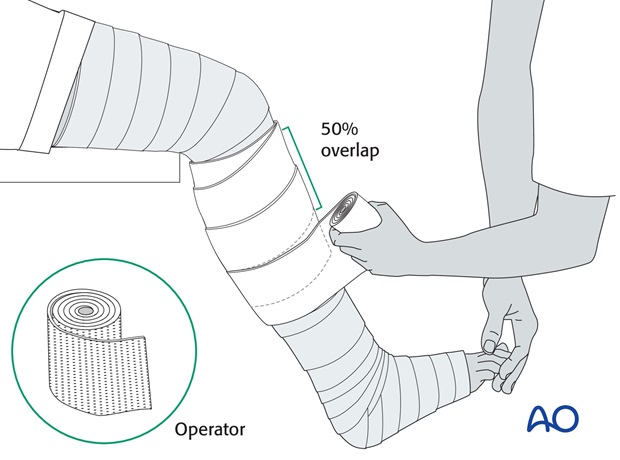
Handling of plaster bandages
It is important to hold the plaster rolls correctly during application, so that they can be rolled on, rather than pulled on.
Application of plaster bandages
The below-knee portion of the cast is applied first.
It is easier to start proximally, overlapping by half the width of the roll and moving down the lower leg to around the ankle and foot.
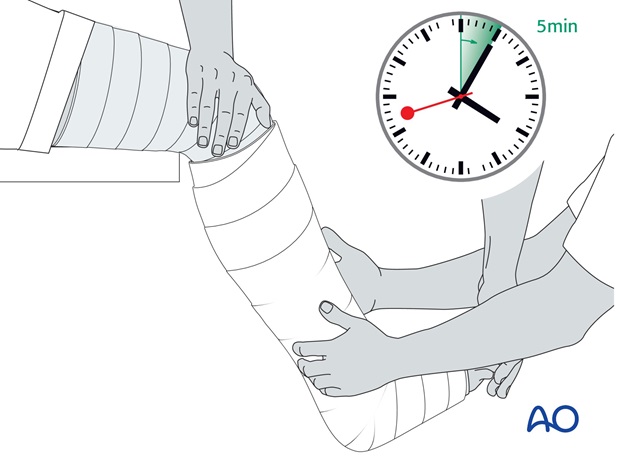
After the application of the second roll, whilst the plaster is still soft, final manipulation, with appropriate molding, is done and the reduction held until the plaster hardens. This may take 4 to 5 minutes, depending on the temperature of the water – colder water gives you more time.
A further two rolls are then applied below the knee and further molding is performed to achieve the desired 3-point fixation.
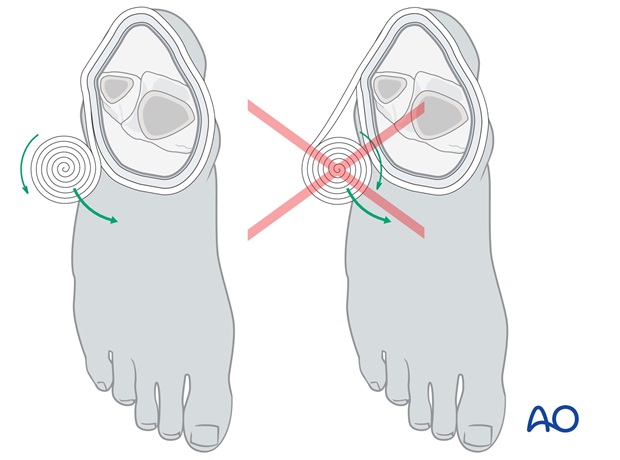
Molding of the cast: 3-point cast fixation
When molding the cast, the same action as for reduction is repeated and held until the plaster is firm.
The principle of 3-point fixation within the cast needs to be applied. The two main molding points are created by gentle pressure over the medial hindfoot and above the lateral supramalleolar part of the lower leg.
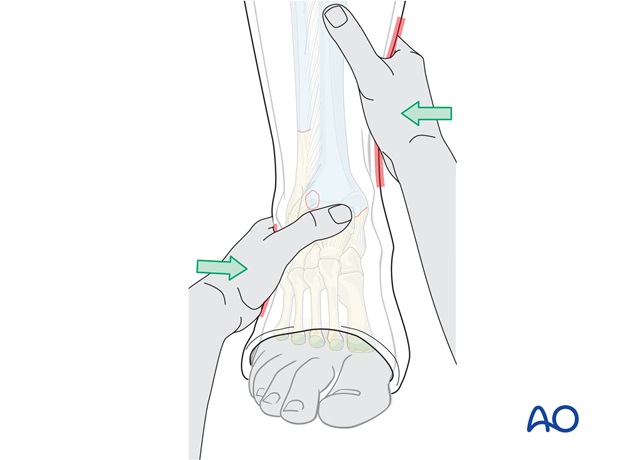
The third point is created by molding the upper end of the cast around the leg, over the medial aspect of the leg.
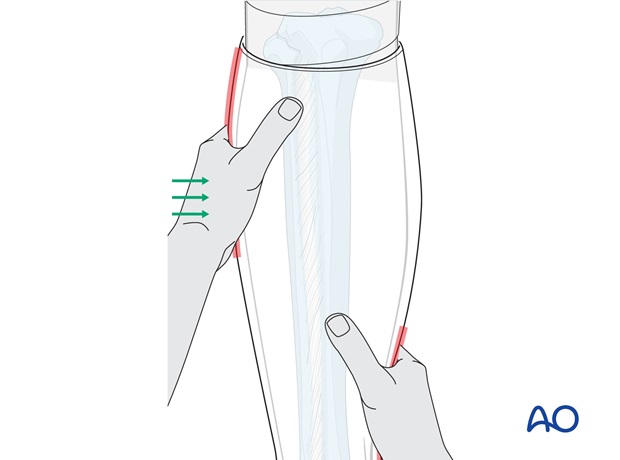
Firm molding around and even over the lateral malleolus helps to close the diastasis and allows the syndesmosis to heal.
Application of the above-knee portion of the cast
The above-knee portion of the cast is then added. Care must be taken not to leave folds of plaster pressing into the back of the knee.
Whilst the plaster is setting the leg must be held still, if the knee moves whilst the cast is setting cracks will occur.
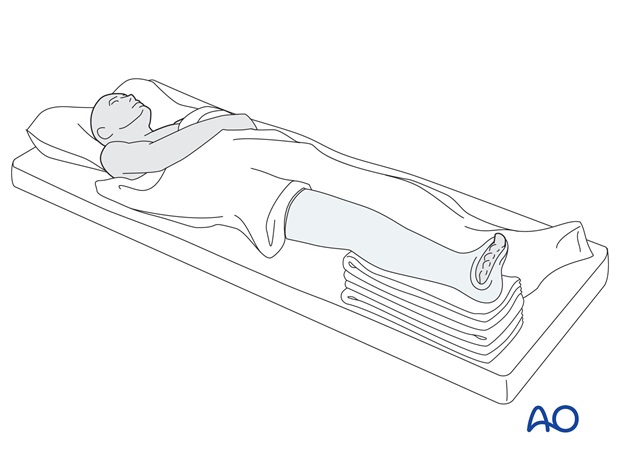
6. Evaporation period
The patient should be warned that the leg in the plaster will feel cool and moist. This is due to the evaporation of water from the plaster. Once the cast is dry, the moist, cold feeling will disappear.
During the evaporation period, the casted limb should remain exposed and not fully covered by blankets.
Tip
Remember that the plaster requires over 24 hours to reach full strength.
Compartment syndrome
Any plaster, especially one without adequate padding, carries a risk of causing obstruction of circulation and compartment syndrome.
In case of inappropriate pain, especially on passive dorsiflexion or plantarflexion of the toes, the plaster and padding should be split immediately down to skin, over its whole length, and the leg watched carefully for rapid recovery. It is better to lose the reduction than to risk muscle necrosis.
If the slightest suspicion of compartment syndrome remains, the plaster needs to be removed and urgent dermatofasciotomy considered.
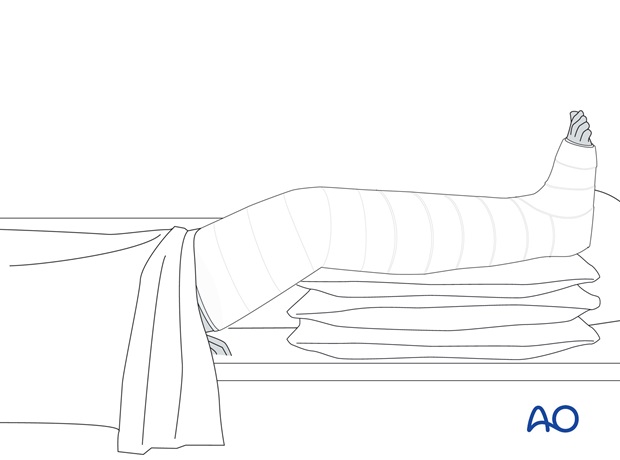
7. Aftercare
General guidelines
Elevate the lower leg on 2-3 pillows for 3-5 days.
X-ray control after reduction confirms the position, but must be repeated after 3-5 days. Redisplacement usually occurs during the early days, as the swelling subsides, and if diagnosed early enough, can often still be corrected non-operatively.
Analgesics and anti-inflammatory drugs should be prescribed, as necessary, during the first few weeks. If analgesia consumption is unexpectedly high, suspect redisplacement, or cast pressure on the skin.
If a cast becomes loose, it should be removed and replaced with a new one. If possible, wait until the fracture has become sticky (+/- 4 weeks) so that the reduction is not lost during the replacement procedure, but check regularly for redisplacement.
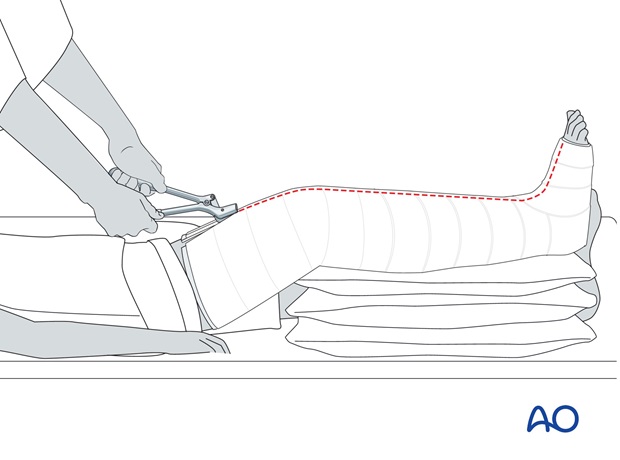
The above-knee cast is maintained for the first 4-6 weeks.
Thereafter, the cast may be changed to a below-knee cast for the remaining period of casting, as determined by the surgical decision-maker. Knee mobilization can now be started.
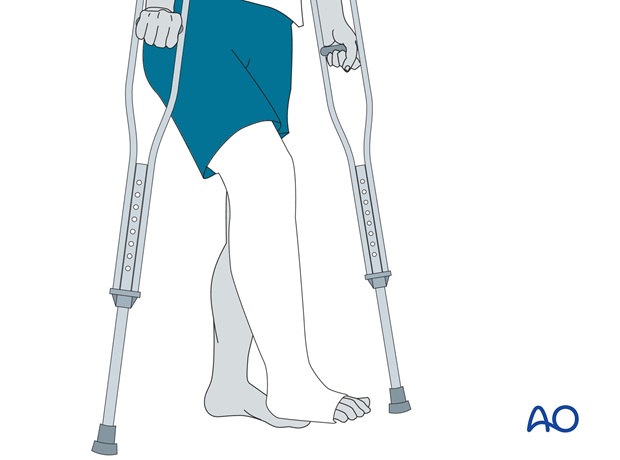
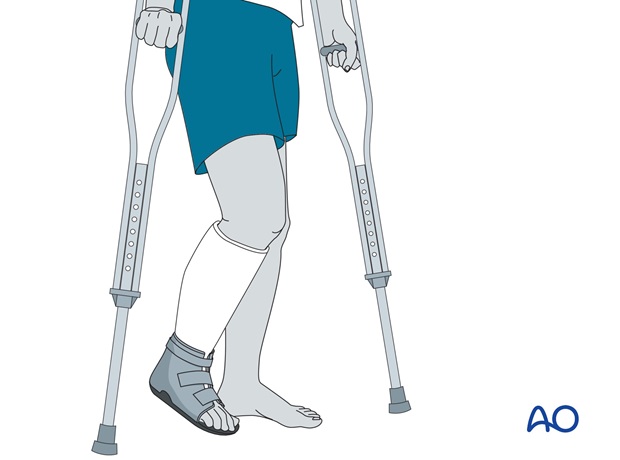
Non weight bearing should be maintained for 4-6 weeks. Thereafter, graduated weight bearing can be started, reaching full weight bearing by 8-10 weeks.
The plaster cast should not be removed before 10-12 weeks, or before the patient manages to walk pain-free with the cast.
After removal of the cast, rehabilitation should involve dedicated ankle and foot mobilization for a prolonged period. At this stage, it is also advisable to give a non-steroidal anti-inflammatory preparation for several weeks.
8. Postoperative treatment of ankle fractures treated with a cast/brace
If the patient complains of severe or increasing pain, the possibility of compartment syndrome or other circulatory disorders should be considered. The cast should be split or the brace loosened. If this does not result in a rapid improvement, the cast or brace should be removed.
Mobilize the patient as soon as possible. Weight bearing is allowed in stable fractures.
Remove the plaster if the patient feels pain, and check the soft tissues for pressure sores.
If the cast loosens, it should be changed and renewed. The cast is removed after 6 to 8 weeks.
Physiotherapy is then usually necessary for 2-4 weeks.
In some patients, additional swelling occurs after removal of the cast. This can be treated with an elastic bandage, or a compression stocking.
At 3 months, if there are symptoms of lateral instability, either inversion stress x-rays or MRI can be used to investigate lateral ligament integrity.













