Collateral ligament reattachment
1. General considerations
Suture anchors or bone tunneling
Two alternative techniques are available for collateral ligament reattachment: suture anchors or bone tunneling.
The advantage of suture anchors is the relative ease of the procedure. It is also a time-saving technique.
Tunneling is the more demanding procedure, but it is significantly less expensive.
This fracture type may be associated with metacarpophalangeal (MCP) joint dislocation. In this case, the dislocation must be manipulated, and any interposed soft-tissue structures removed.
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.

3. Approach
For this procedure, a dorsal approach to the metacarpophalangeal joint is typically used.
4. Reduction of dislocation
Closed reduction
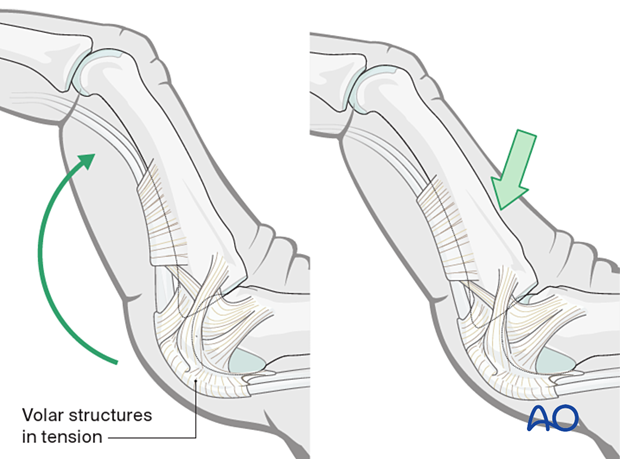
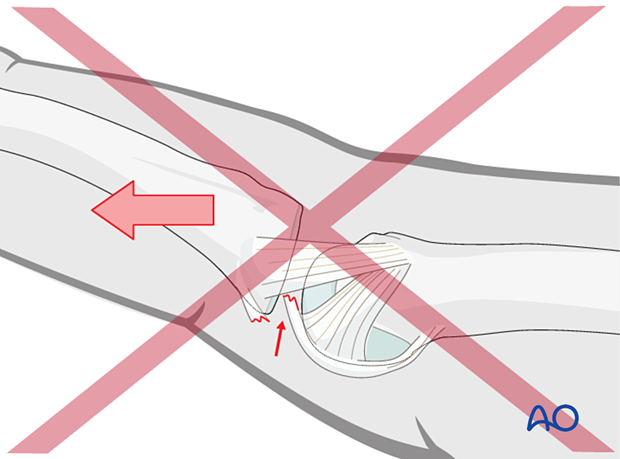
Dislocation usually occurs as an extension deformity.
This can be reduced by increasing the deformity with some dorsally applied pressure on the proximal phalanges to reduce the joint. This keeps the volar structures in tension and reduced the risk of soft-tissue interposition.
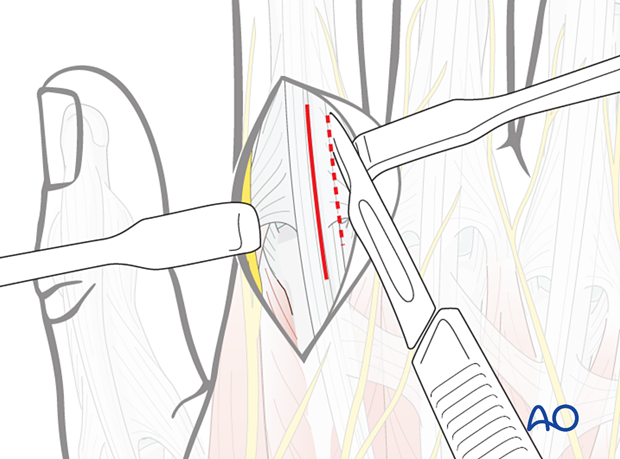
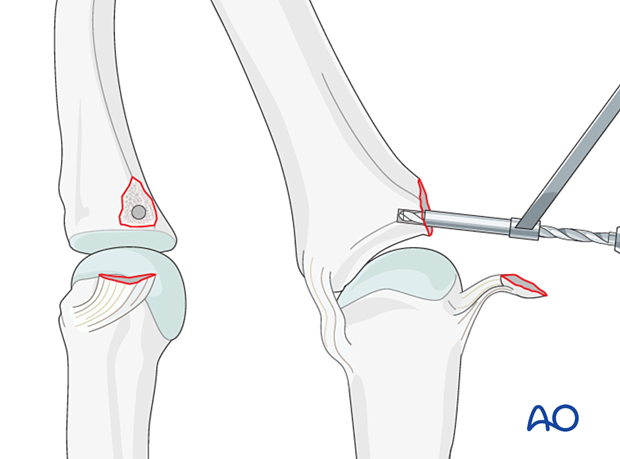
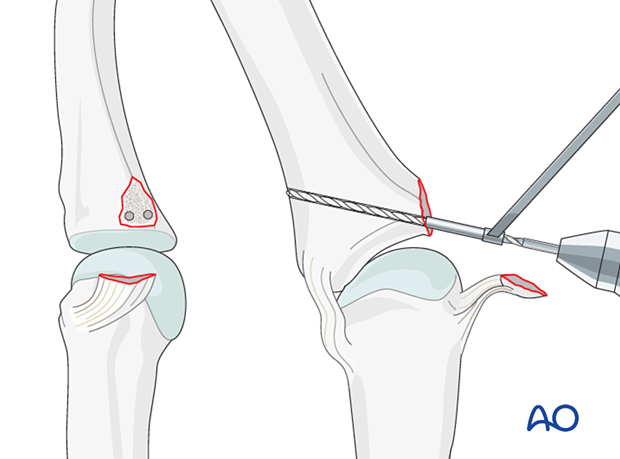
5. Visualizing the joint
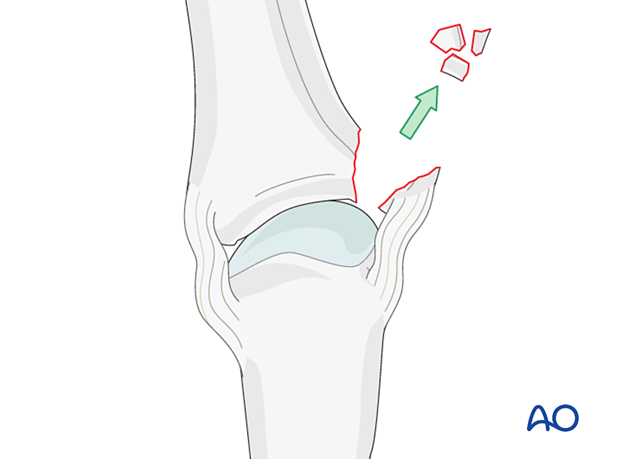
All free fragments need to be removed to prevent obstruction of joint movement.
Fragments remaining attached to the ligament should be maintained.
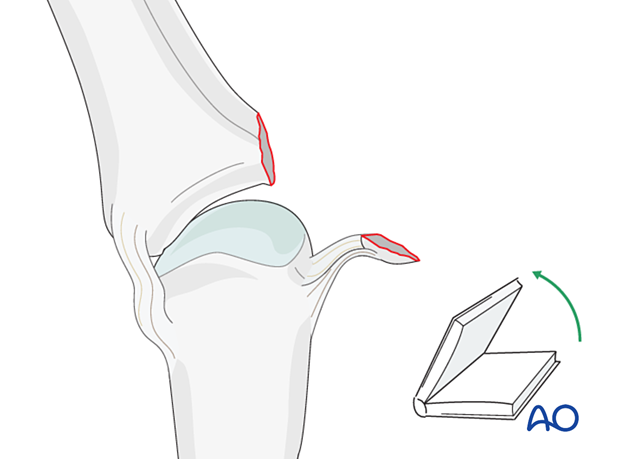
Laterally deviate the phalanx in the opposite direction to gain maximal visualization of the joint (“open the book”). Remove all loose bony fragments.
6. Option 1 – Suture anchor fixation
Drilling an anchor hole
Keep the phalanx laterally deviated to visualize maximally the area of the fracture at the base of the proximal phalanx.
Insert the anchor according to the manufacturer’s instructions as close as possible to the subchondral bone.
Insertion of the anchor
Insert the anchor.
Ensure that the whole anchor is completely buried in the bone.
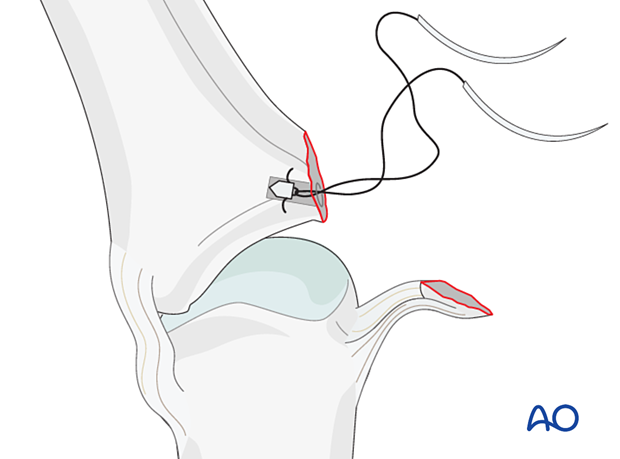
Insertion of sutures
Transfix the ligament and associated bone fragments with the anchor sutures.
Reapproximate the ligament to the phalanx and make a loop in each end of the thread as an anchoring pass. Tie a knot to secure the ligament to the phalanx.
Reattaching the ligament close to the subchondral bone will ensure a smooth surface for ideal mobility.
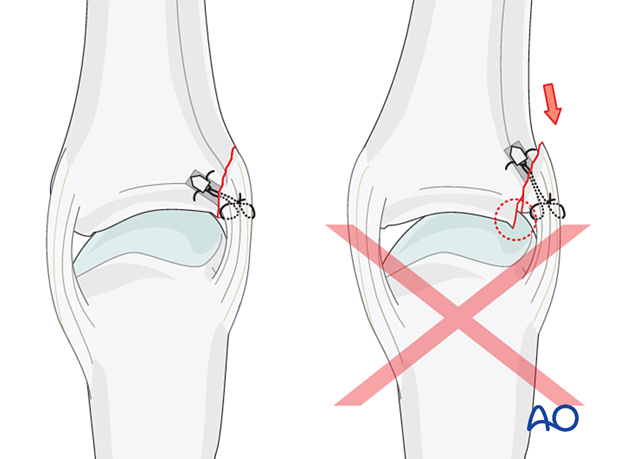
Pitfall
- Articular surface damage
- Joint instability
- Joint stiffness
- Progressive arthritis
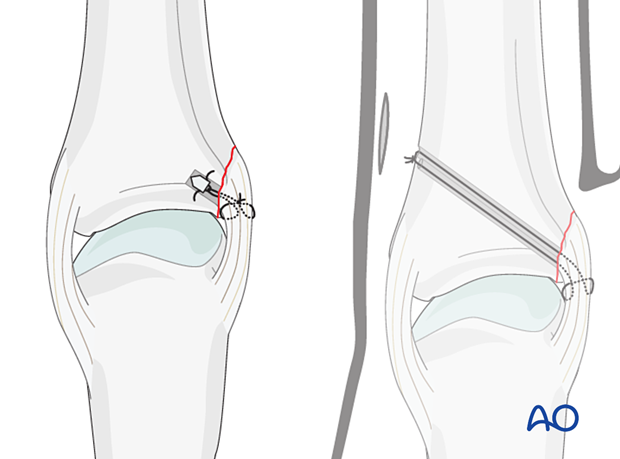
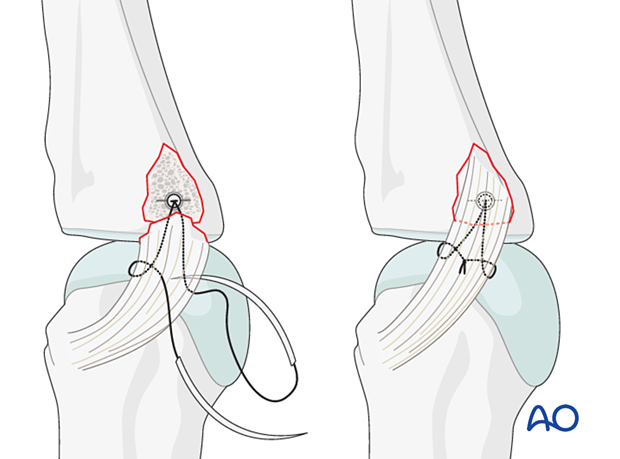
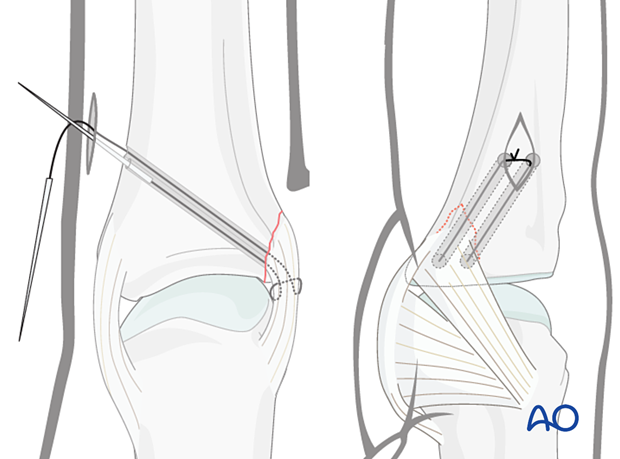
7. Option 2 – Bone tunneling
Drilling holes
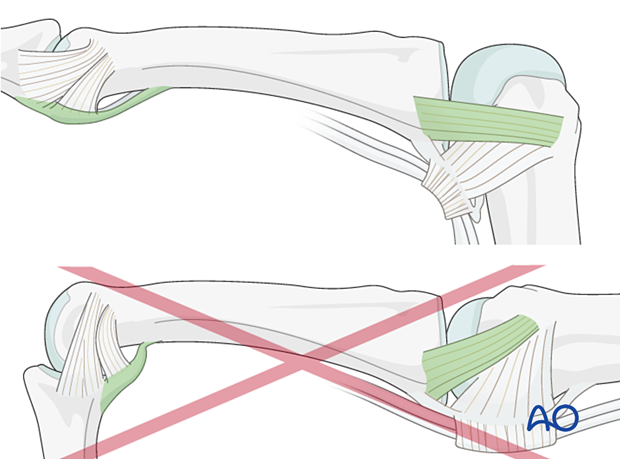
A pair of parallel perforations, using a 1.0 mm drill or a K-wire, can be made as close as possible to the subchondral bone, angled from proximal to distal, penetrating the opposite cortex.
A drill sleeve for soft-tissue protection is mandatory.
Insertion of sutures
4.0 nonresorbable, braided sutures, with straight needles, are used.
Insert the sutures obliquely through the end of the ligament, make a loop in each end of the thread as an anchoring pass, and thread each needle through a drill hole.
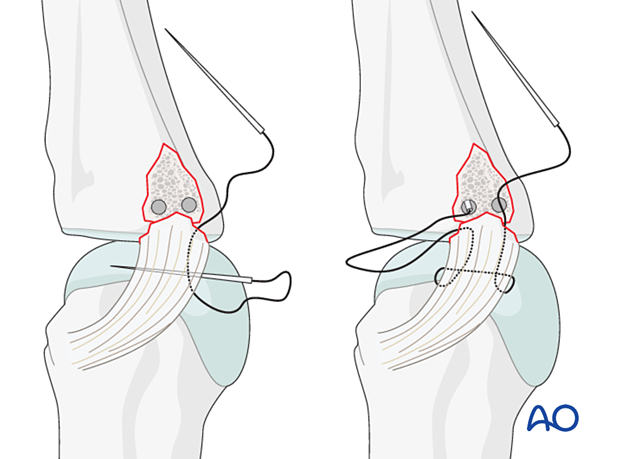
Make a small incision in the opposite side of the finger to retrieve the sutures. Cut off the needles, pull the sutures to approximate the ligament, and tie a knot over the cortical bone.
8. Final assessment
Confirm anatomical reduction and fixation with an image intensifier.
9. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
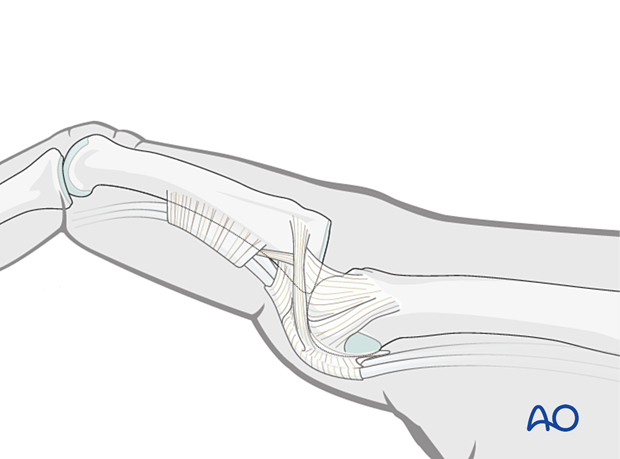
Postoperative treatment
The hand is supported with a dorsal splint for at least 3 weeks. This would allow for finger movement and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
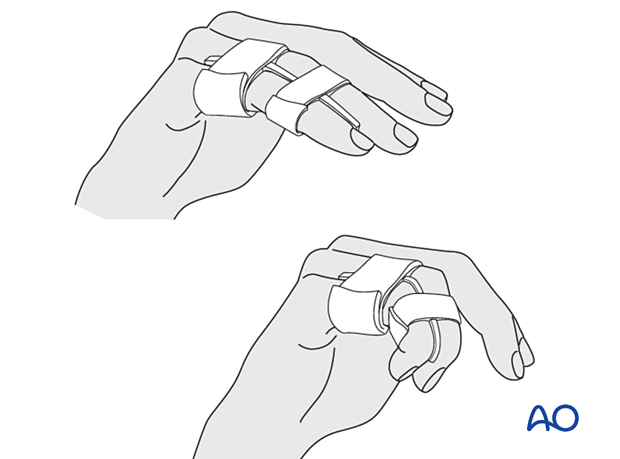
The hand should be splinted in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- MCP joint in 90° flexion
- PIP joint in extension
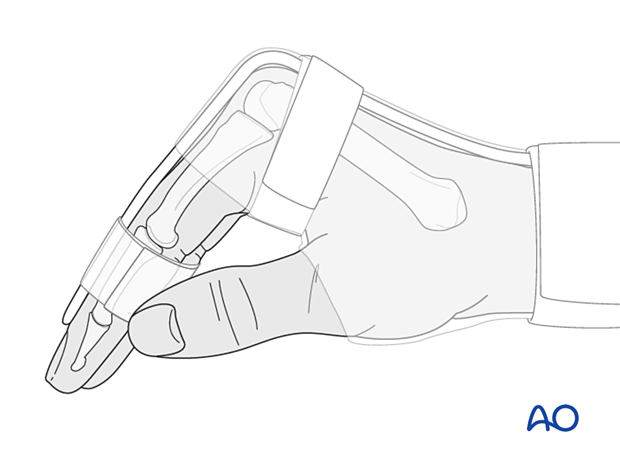
The reason for splinting the MCP joint in flexion is to maintain its collateral ligament at maximal length, avoiding scar contraction.
PIP joint extension in this position also maintains the length of the volar plate.
Follow-up
See the patient 5 days after surgery to check the wound, and clean and change the dressing.
After 10 days, remove the sutures. Check x-rays.
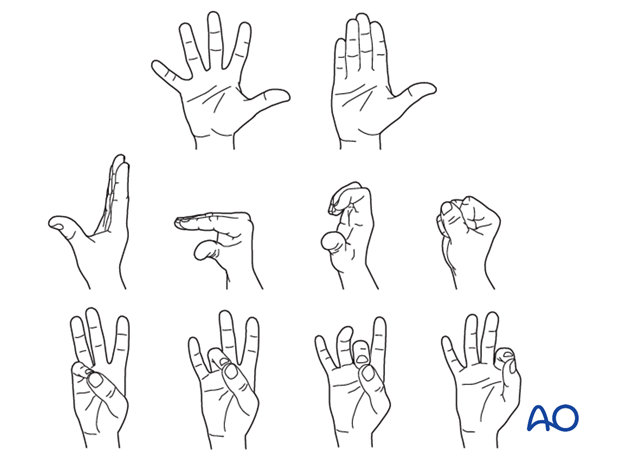
Functional exercises
The healing process is slower than in bone-to-bone repair and will take 3–4 weeks.
At this stage, remove the splint, and apply buddy strapping.
To prevent joint stiffness, the patient should be instructed to begin active motion (flexion and extension) immediately after surgery.