Cerclage compression wiring
1. General considerations
Introduction
A partial articular fracture of the proximal phalangeal base without comminution may be stabilized with cerclage compression wiring.
A disadvantage of this fixation is the need to remove the wires as the construct is very bulky.
This fracture type may be associated with metacarpophalangeal (MCP) joint dislocation. In this case, the dislocation must be manipulated, and any interposed soft-tissue structures removed.
The tension band converts tensile forces into compression forces.
In a case such as the illustrated fracture, the tension band will be applied in static mode.
Compared to cerclage compression constructs in other anatomical regions, in the proximal phalanx only one K-wire is used.
This form of fixation was referred to as a “Tension band fixation”. We now prefer the term “Cerclage compression wire fixation” because the tension band mechanism cannot be applied consistently to each component of the fracture fixation. An explanation of the limits of the tension band mechanism/principle can be found here.
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.

3. Approach
For this procedure, a dorsal approach to the metacarpophalangeal joint is typically used.
4. Reduction of dislocation
Closed reduction
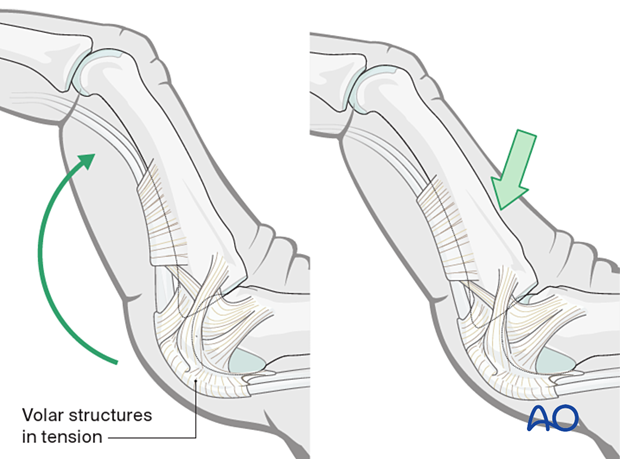
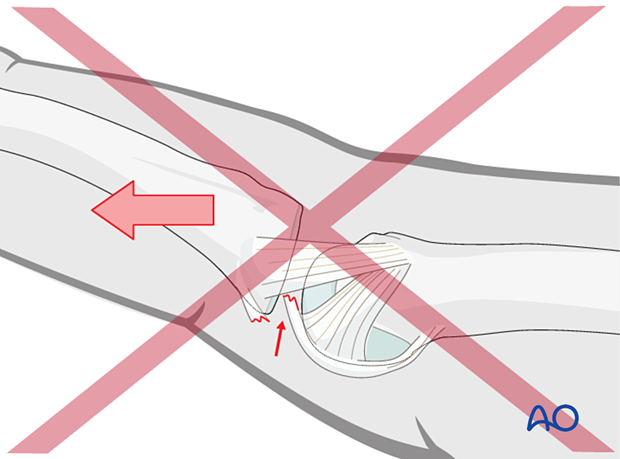
Dislocation usually occurs as an extension deformity.
This can be reduced by increasing the deformity with some dorsally applied pressure on the proximal phalanges to reduce the joint. This keeps the volar structures in tension and reduced the risk of soft-tissue interposition.
5. Fracture reduction
Direct reduction
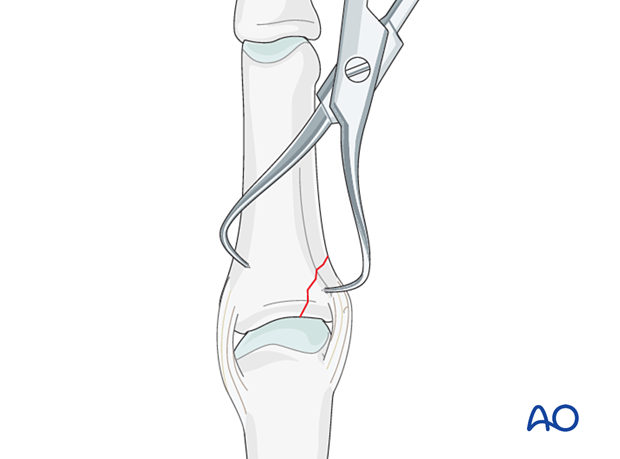
In displaced fractures, open reduction is often necessary.
Use small pointed reduction forceps gently to reduce the fracture from palmar to dorsal and from proximal to distal. Application of excessive force can result in fragmentation. Do not use forceps in tiny fragments.
Stability evaluation
Confirm reduction with an image intensifier and check the joint stability by flexion and extension. This should show congruent movement compared with the adjacent joints.
6. Wire fixation
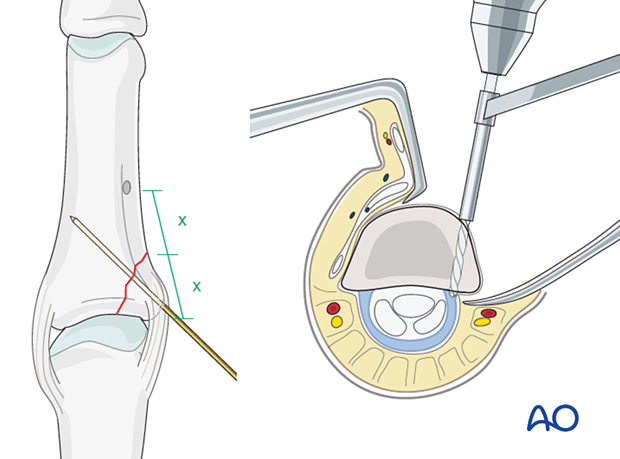
K-wire insertion
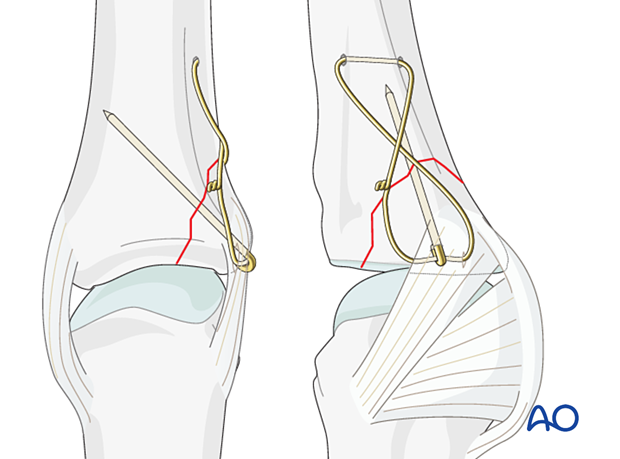
Hold the reduction by inserting the K-wire through the center of the fracture surface. Make sure not to cross the far cortex.
Check reduction using image intensification.
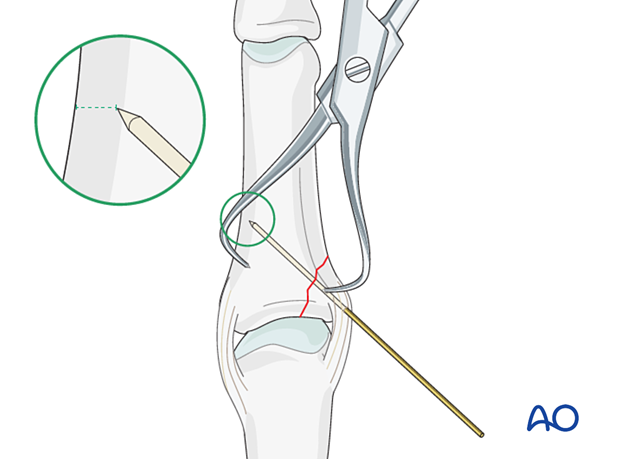
Drilling a hole
Drill a hole in the proximal phalanx, from dorsal to palmar.
The location of the drill hole should be the same distance from the fracture line as the avulsed fragment’s length.
Use a drill guide, for soft-tissue protection, and either a slow-spinning 1.5 mm drill, or a 1 mm K-wire.
Wire insertion
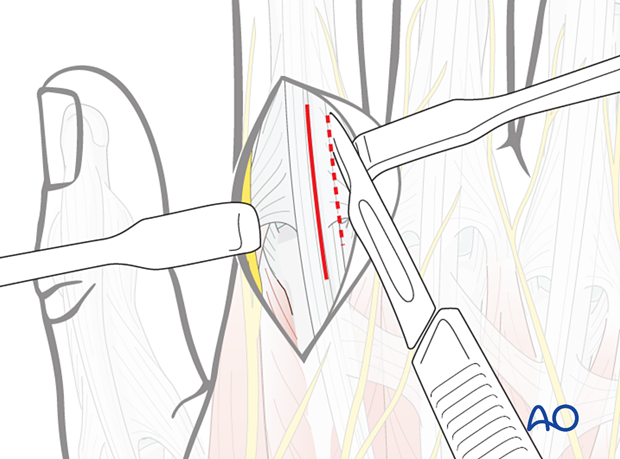
Thread a 26–28-gauge stainless steel monofilament 0.6 mm wire through the drill hole.
A curved hemostat can be used to retrieve the wire from the palmar surface, sliding it very closely to the cortical bone to avoid damage to the digital nerve and artery.
Periosteal elevators can be used for protection.
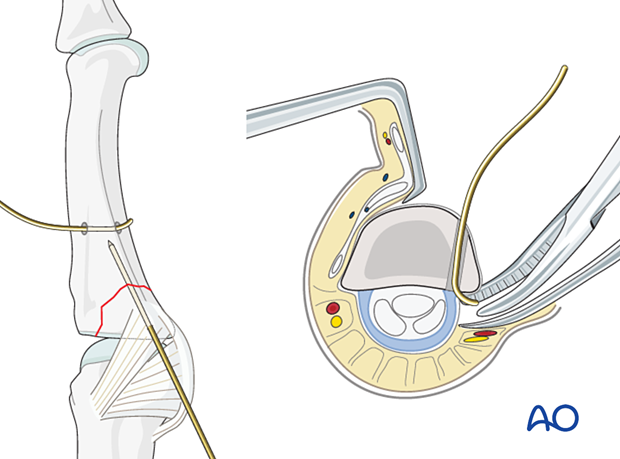
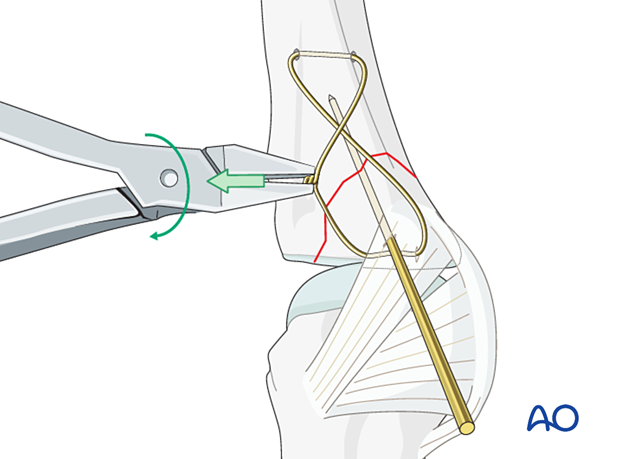
Wire application
The wire must pass close to the bone and through the ligament to protect vascularity.
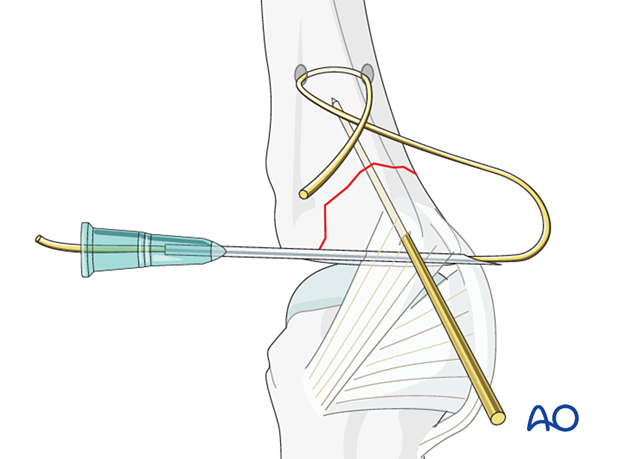
The wire is passed around the fragment and K-wire, and through the ligament attachment in a figure-of-eight mode.
This can be achieved by passing a syringe needle of appropriate diameter on the surface of the bone, deep to the ligament attachment, and then inserting one end of the wire into the tip of the needle. The needle and the wire are then carefully drawn through, guiding the wire along the correct track.
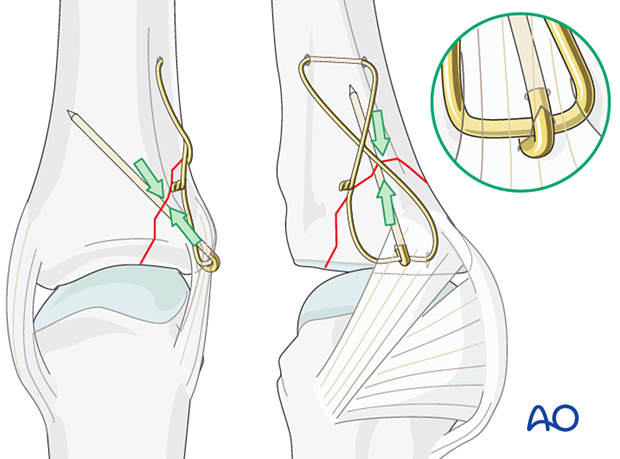
Anchoring the K-wire
Check position of the K-wires under image intensification. If the tip of the wire is in contact with the far cortex, then retract the K-wire by about 2 mm, bend it through 180°, cut the wire to form a small hook, and impact the bent tip into the bone.
Use image intensification finally to ensure anatomical reduction.
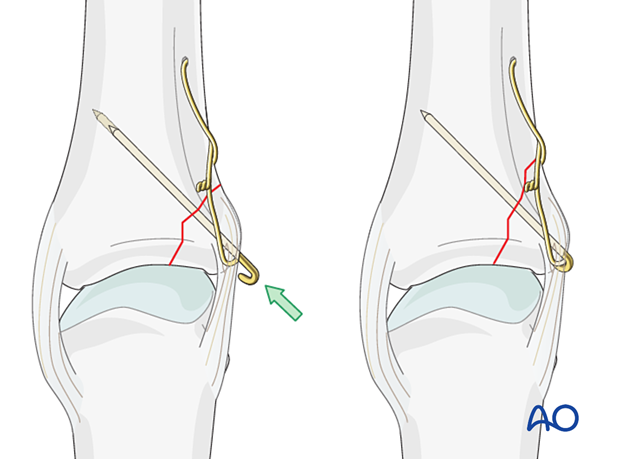
Tightening the wire
Once the fragment is reduced, the wire is tightened, cut short, and bent along the phalanx, to avoid soft-tissue irritation.
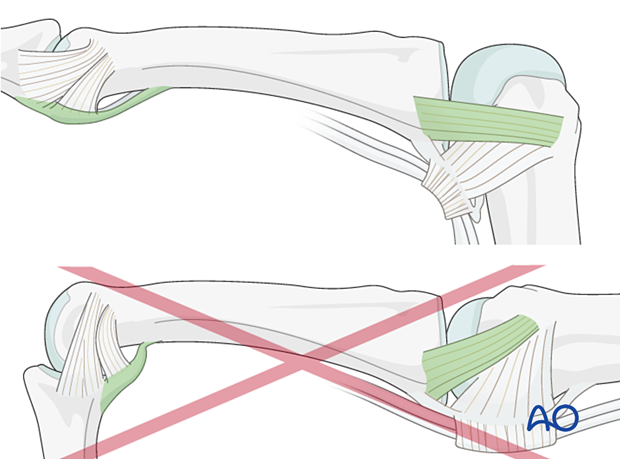
When tightening the wire, ensure that both ends are twisted into each other rather than twisting one end around the other straight end.
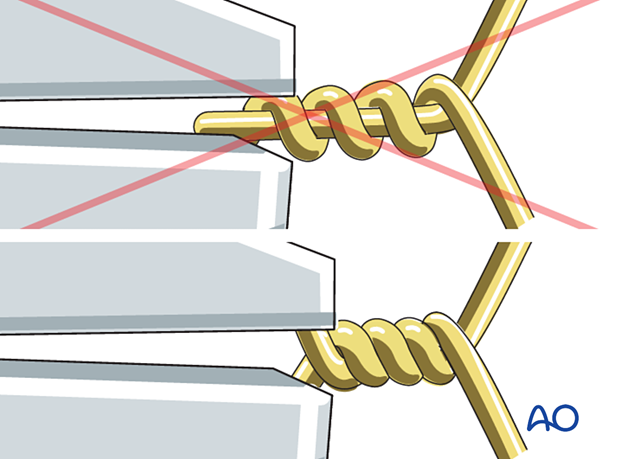
This is achieved by using traction with the pliers to tighten the loop and the twisting, still under tension, to take out the slack.
7. Alternative fixations
Anchor screw
An alternative way of anchoring the figure-of-eight wire distally in the phalanx is the use of a screw instead of a drill hole.
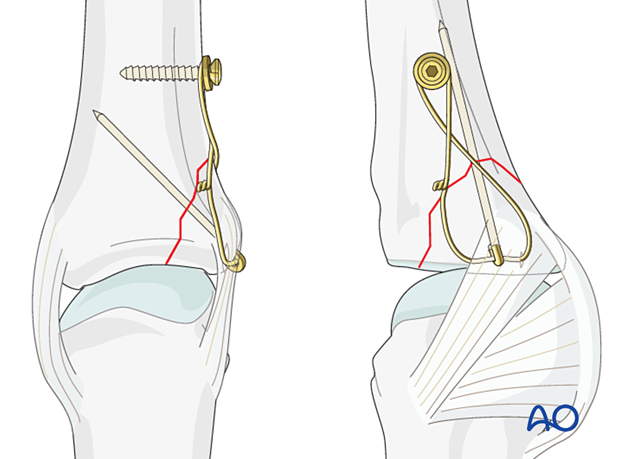
Small fragment
If the avulsed fragment is too small to risk further damage by passing a K-wire, a simple figure-of-eight cerclage wire is used.

8. Final assessment
Confirm anatomical reduction and fixation with an image intensifier.
9. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
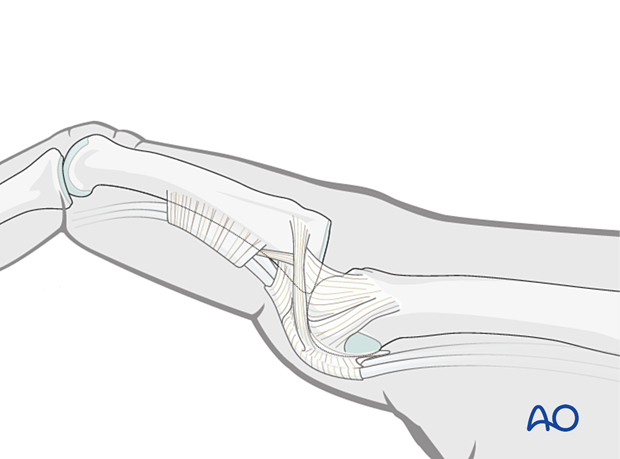
If there is swelling, the hand is supported with a dorsal splint for a week. This would allow for finger movement and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
The hand should be splinted in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- MCP joint in 90° flexion
- PIP joint in extension
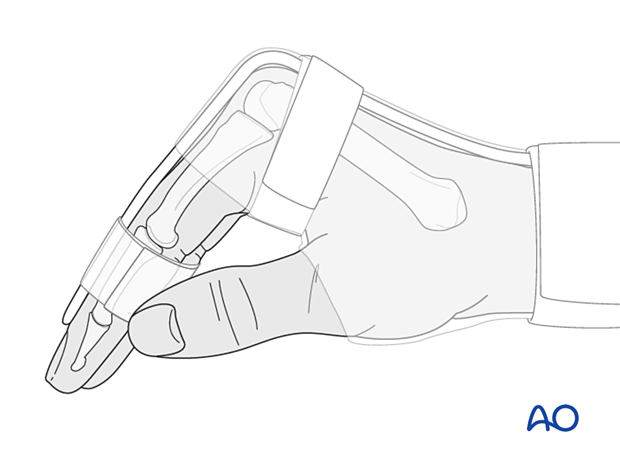
The reason for splinting the MCP joint in flexion is to maintain its collateral ligament at maximal length, avoiding scar contraction.
PIP joint extension in this position also maintains the length of the volar plate.
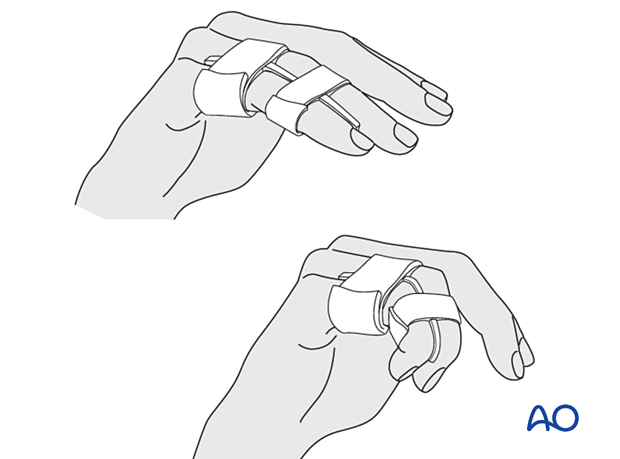
After subsided swelling, protect the digit with buddy strapping to a neighboring finger to neutralize lateral forces on the finger.
Functional exercises
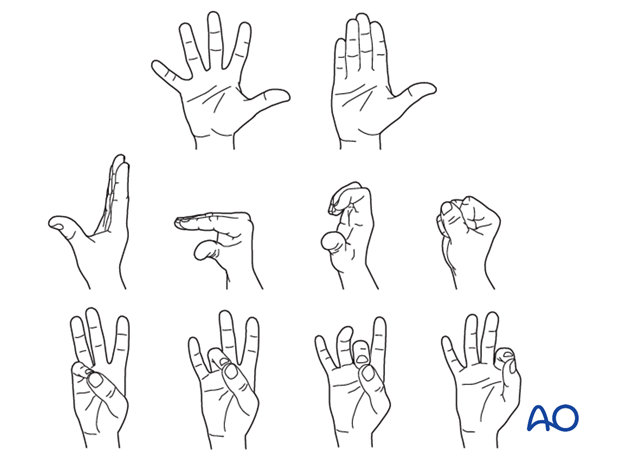
To prevent joint stiffness, the patient should be instructed to begin active motion (flexion and extension) immediately after surgery.
Follow-up
See the patient after 5 and 10 days of surgery.
Implant removal
The wires need to be removed in case of soft-tissue irritation, but not before fracture consolidation.













