K-wire fixation
1. General considerations
Introduction
K-wire fixation is optimal for fracture fixation in pediatric patients. In some cases, it can be used in adults with the disadvantage of not producing interfragmentary compression to reduce the articular surface gap. It also needs longer support with a splint to prevent fracture displacement.
Tiny and fragile fragments cannot be fixed with K-wires. Suture anchoring, cerclage wiring, and bone tunnel fixation alternatives should be considered.
At least two K-wires need to be inserted in a diverging or converging manner for optimal rotational stabilization.
Reduction can be achieved in a closed or open manner. Closed reduction is easier with acute fractures and has the advantage of sparing the hematoma. Anatomical reduction is key to avoiding posttraumatic arthrosis.
There is a high risk of non- or malunion and wire-track infection (osteitis).
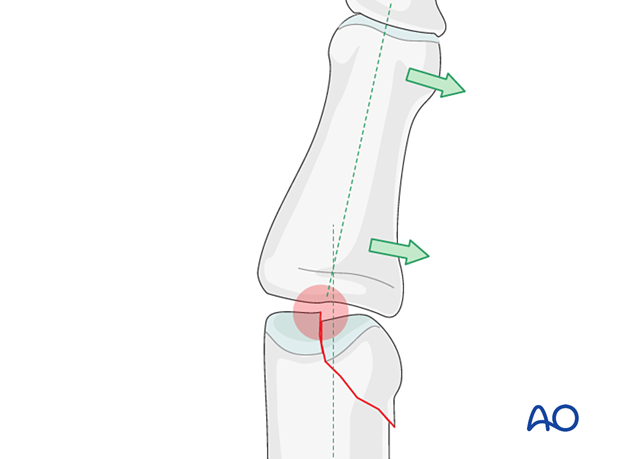
Anatomical reduction mandatory
Articular fractures must be reduced anatomically. Otherwise, the articular cartilage may be damaged, leading to painful degenerative joint disease and digital deformity.
This illustration shows how even slight unicondylar depression may lead to angulation of the finger.
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.

3. Reduction
Reduction by ligamentotaxis
Often, the fracture can be reduced by applying traction via finger traps.
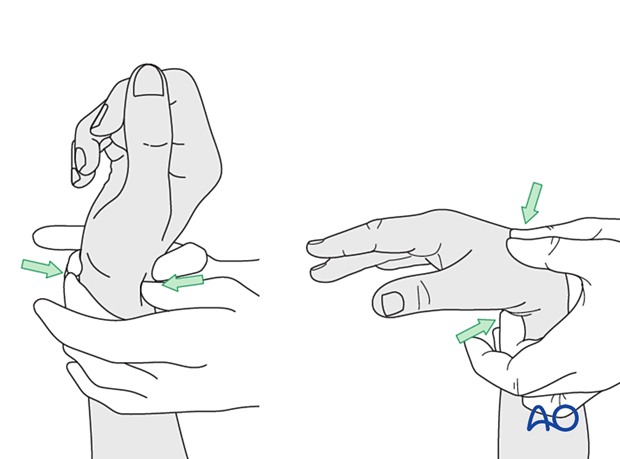
Indirect reduction
Reduction starts with traction to restore length.
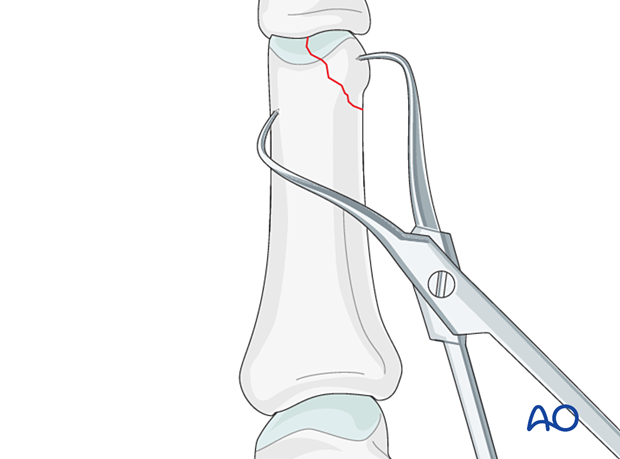
Exert lateral pressure with your thumb and index finger or with dedicated percutaneous reduction forceps to reduce the fracture.
Confirm reduction with an image intensifier.
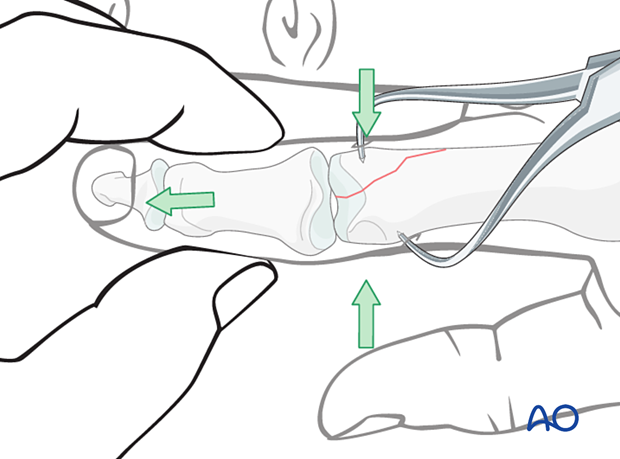
Open reduction
If closed reduction is not successful or in a nonacute case, proceed with an open reduction.
When indirect reduction is not possible, this is usually due to interposition of parts of the extensor apparatus.
4. K-wire fixation
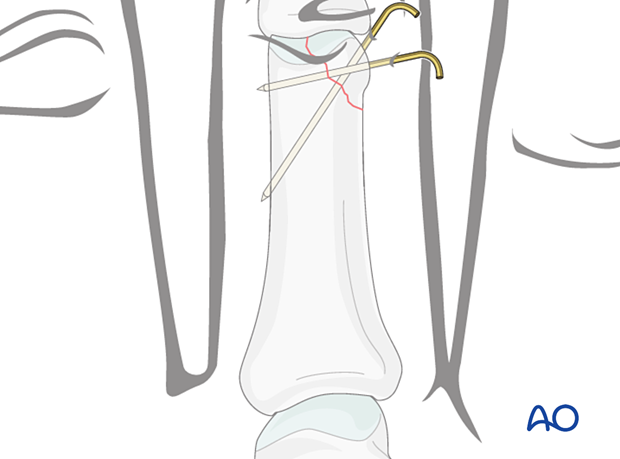
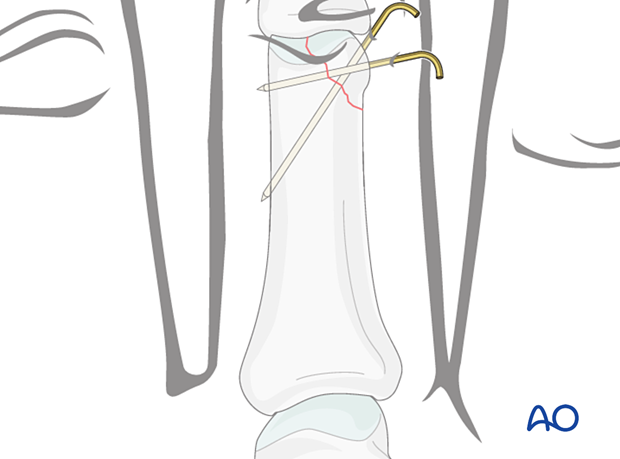
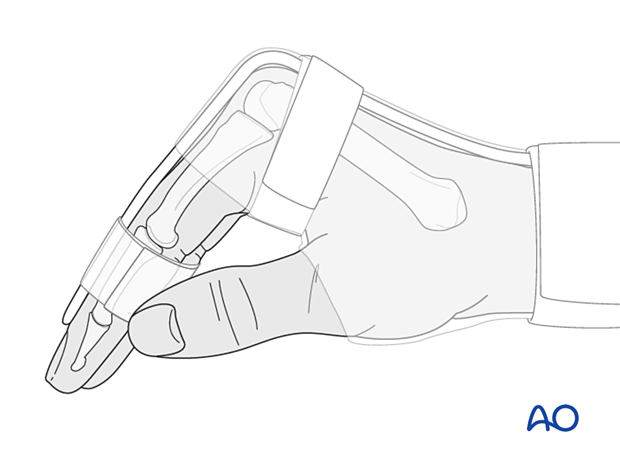
Insert two K-wires through the fracture plane in a crossing manner through both cortices. The K-wire tracks should not cross each other near the fracture plane.
Take care not to injure the extensor tendon.
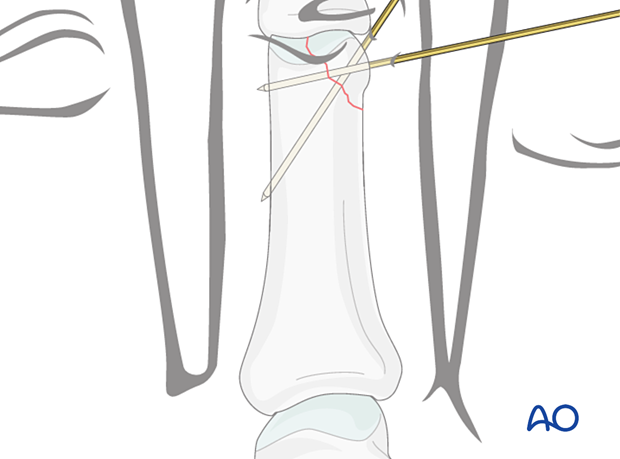
The ends of the K-wires may be left protruding the skin for later removal or buried under the skin.
To protect the skin, bend the K-wire ends with pliers in an L- or U-shape.
5. Checking alignment
Identifying malrotation
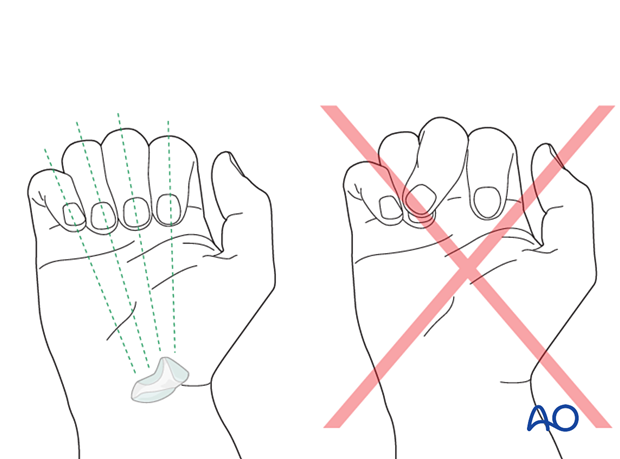
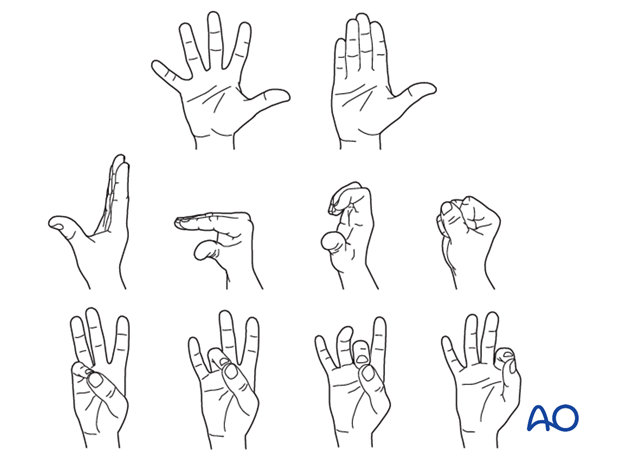
At this stage, it is advisable to check the alignment and rotational correction by moving the finger through a range of motion.
Rotational alignment can only be judged with flexed metacarpophalangeal (MCP) joints. The fingertips should all point to the scaphoid.
Malrotation may manifest by an overlap of the flexed finger over its neighbor. Subtle rotational malalignments can often be judged by a tilt of the leading edge of the fingernail when the fingers are viewed end-on.
If the patient is conscious and the regional anesthesia still allows active movement, the patient can be asked to extend and flex the finger.
Any malrotation is corrected by direct manipulation and later fixed.
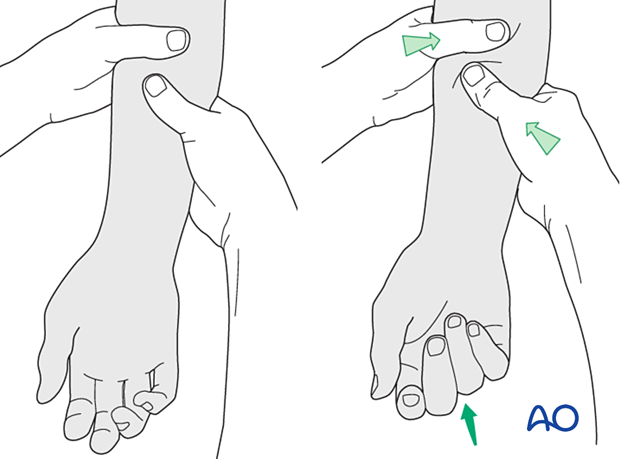
Using the tenodesis effect when under anesthesia
Under general anesthesia, the tenodesis effect is used, with the surgeon fully flexing the wrist to produce extension of the fingers and fully extending the wrist to cause flexion of the fingers.
Alternatively, the surgeon can exert pressure against the muscle bellies of the proximal forearm to cause passive flexion of the fingers.
6. Final assessment
Confirm fracture fixation and stability with an image intensifier.
7. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
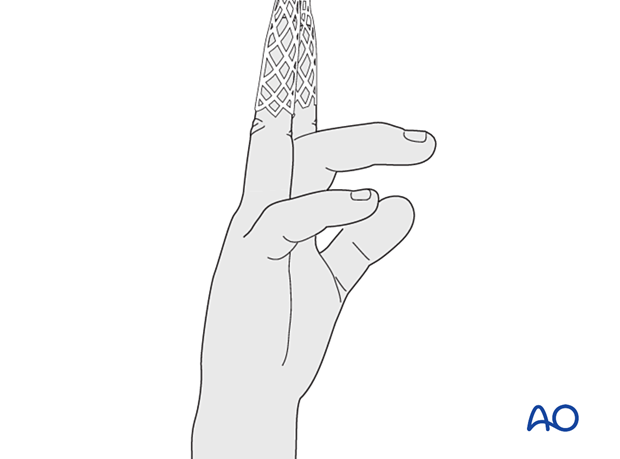
The hand is supported with a dorsal splint for 4 weeks. This would allow for finger movement and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
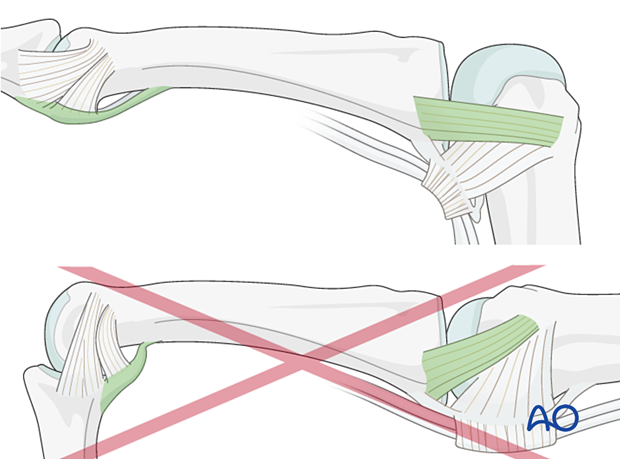
The hand should be splinted in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- MCP joint in 90° flexion
- PIP joint in extension
The reason for splinting the MCP joint in flexion is to maintain its collateral ligament at maximal length, avoiding scar contraction.
PIP joint extension in this position also maintains the length of the volar plate.
Functional exercises
To prevent joint stiffness, the patient should be instructed to begin active motion (flexion and extension) immediately after surgery.
Follow-up
See the patient after 5 and 10 days of surgery.
Implant removal
K-wires can be removed once consolidation of the fracture is visible.













