External fixation
1. General considerations
External fixation of the proximal phalanx may be used as a temporary treatment in complex fractures or polytrauma situations. After removal of the K-wires, definitive fixation can be performed without delay.
External fixation of a multifragmentary shaft fracture of the proximal phalanx may be performed with 1.2 or 1.4 mm K-wires, two inserted proximally and two distally, connected through a small rod.
Details of external fixation are described in the basic technique for application of modular external fixator.
Specific considerations for the proximal phalanx are given below.
AO teaching video
Mini external fixator
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.

3. Application of external fixator
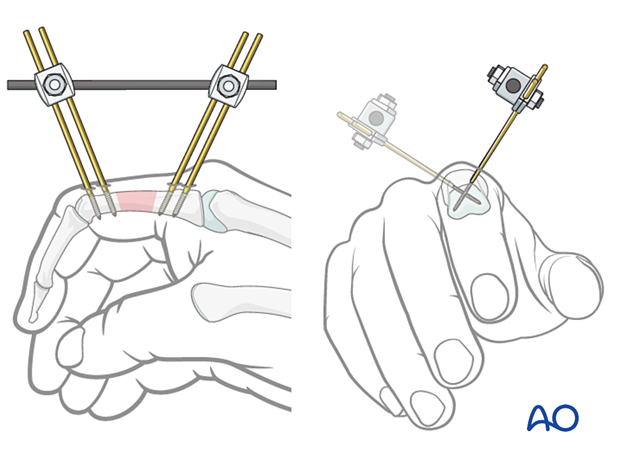
Principles for K-wire insertion into the proximal phalanx
The K-wires should be inserted proximal and distal to the fracture zone to gain optimal stabilization and keep the phalangeal length.
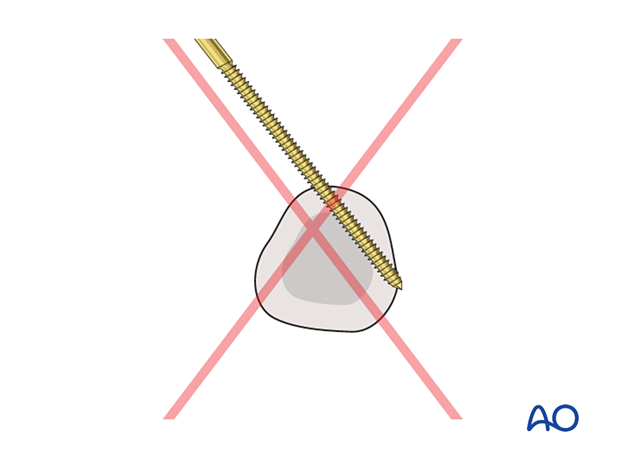
K-wires should be inserted dorsally in an angle of 45° to the sagittal plane. This avoids damage to the extensor tendon and conflict with the other fingers.
The K-wires should obtain a good hold in both cortices.

Assembly of external fixation construct
Assemble the external fixator with a rod, rod-to-wire clamps, and the four K-wires.

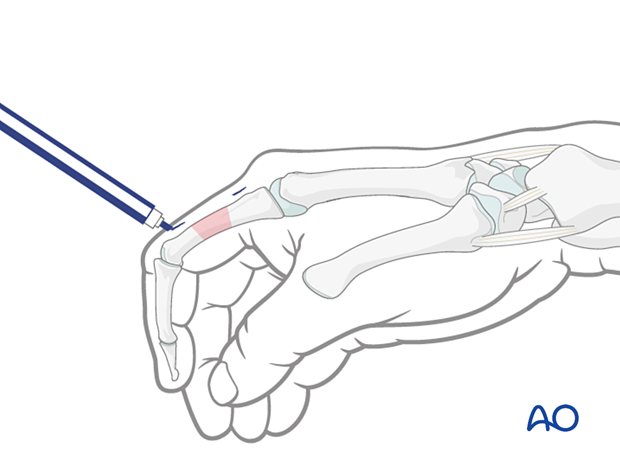
Insertion of K-wires
Mark the insertion points for the K-wires near to the fracture zone on the skin after checking with an image intensifier.
Adjust the fixator construct accordingly.
Confirm axial and rotational alignment of the two main fragments.
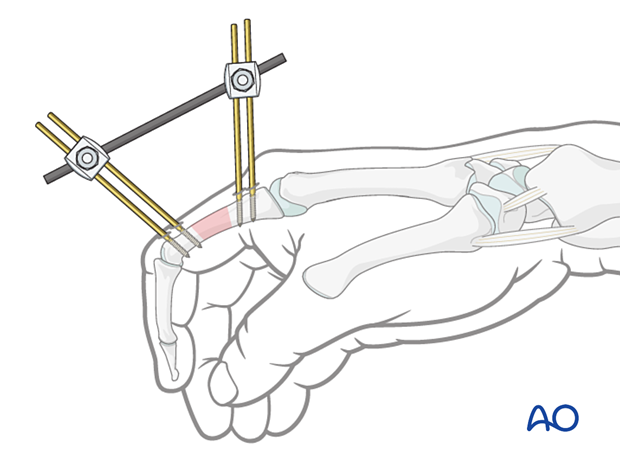
Insert the K-wires using the fixator construct as a guide.

Finalization of external fixation construct
Confirm alignment with an image intensifier. If necessary, adjust length.
Tighten the clamps.
4. Aftercare following external fixation
Pin-site care
Proper pin insertionTo prevent postoperative complications, pin-insertion technique is more important than any pin-care protocol:
- Correct placement of pins (see safe zones) avoiding ligaments and tendon
- Correct insertion of pins (eg, trajectory, depth) avoiding heat necrosis
- Extending skin incisions to release soft-tissue tension around the pin insertion (see inspection and treatment of skin incisions)
Various aftercare protocols to prevent pin-track infection have been established by experts worldwide. Therefore, no standard protocol for pin-site care can be stated here. Nevertheless, the following points are recommended:
- The aftercare should follow the same protocol until removal of the external fixator.
- The pin-insertion sites should be kept clean. Any crusts or exudates should be removed. The pins may be cleaned with saline and/or disinfectant solution/alcohol. The frequency of cleaning depends on the circumstances and varies from daily to weekly but should be done in moderation.
- No ointments or antibiotic solutions are recommended for routine pin-site care.
- Dressings are not usually necessary once wound drainage has ceased.
- Pin-insertion sites need not be protected for showering or bathing with clean water.
The patient or the carer should learn and apply the cleaning routine.
In case of pin loosening or pin-track infection, the following steps need to be taken:
- Remove all involved pins and place new pins in a healthy location.
- Debride the pin sites in the operating theater, using curettage and irrigation.
- Take specimens for a microbiological study to guide appropriate antibiotic treatment if necessary.
Before changing to a definitive internal fixation an infected pin track needs to heal. Otherwise, infection will result.
Functional exercises
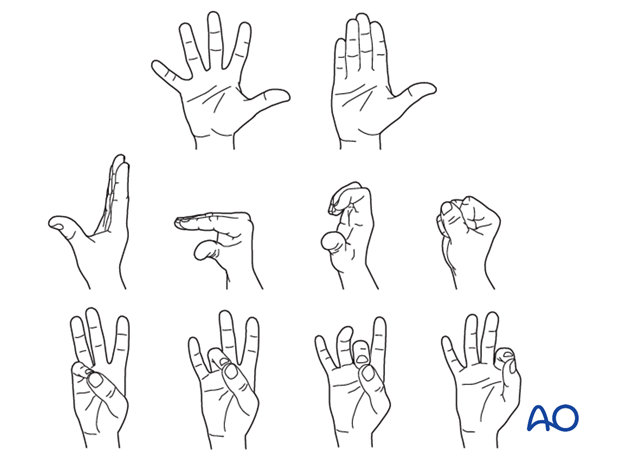
The patient should be instructed to begin active motion (flexion and extension) immediately after surgery to prevent joint stiffness.
If necessary, functional exercises can be under the supervision of a hand therapist.
Secondary treatment
As soon as the soft-tissue conditions allow, a definite procedure can be performed.













