Compression plate fixation
1. Principles
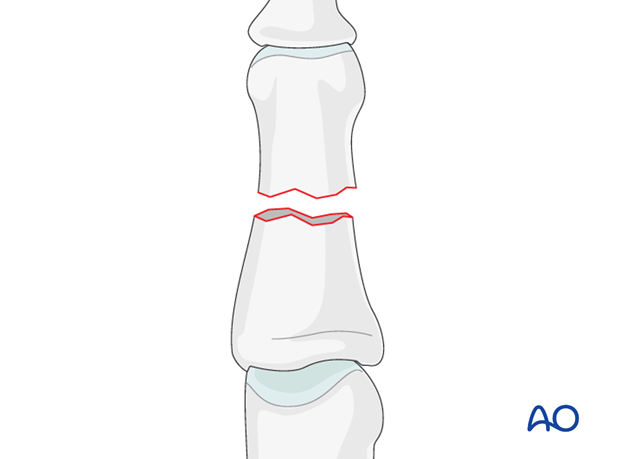
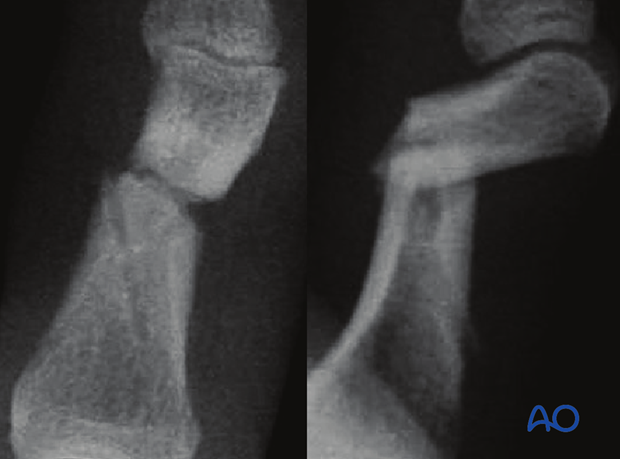
Fractures of the diaphysis can be transverse, oblique, spiral, or comminuted. Reduction is achieved by traction and digital manipulation. When the fracture is stable, it can be treated nonoperatively.
If the fracture is irreducible, ORIF is indicated.
Other indications for ORIF are open fractures, or soft-tissue lacerations.
Outcome of fractures of the middle phalanx is usually more favourable that in the proximal phalanx. This is largely due to the fact that limitations in DIP joint motion is not as great a problem as similar limitations in the PIP and MP joints.
However, since fragments in this segment are generally smaller than in the proximal phalanx, management and stabilization can be more of a challenge. Consequences of malunion (pain or deformity), or of degenerative joint disease, at the DIP joint can well be dealt with by arthrodesis, which is a procedure with very predictable outcome.
2. Approaches
For this procedure the following approaches may be used:
3. Reduction
Indirect reduction by traction
In many cases, the fracture is not significantly displaced.
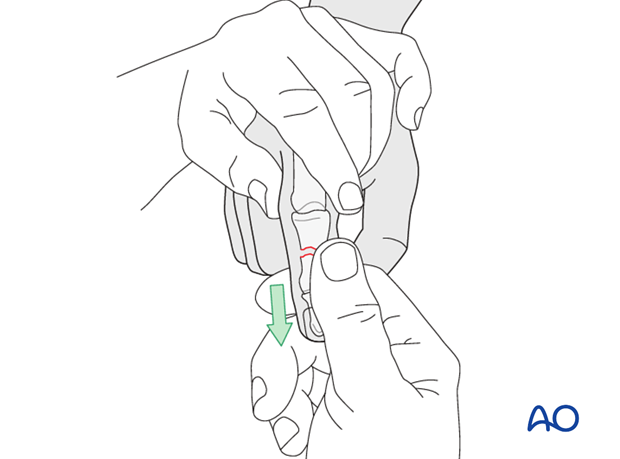
Reduction can be obtained by traction and flexion of the PIP joint exerted by the surgeon.
Confirm reduction using image intensification.
Often, these fractures are stable after reduction, in which case, nonoperative treatment is indicated.
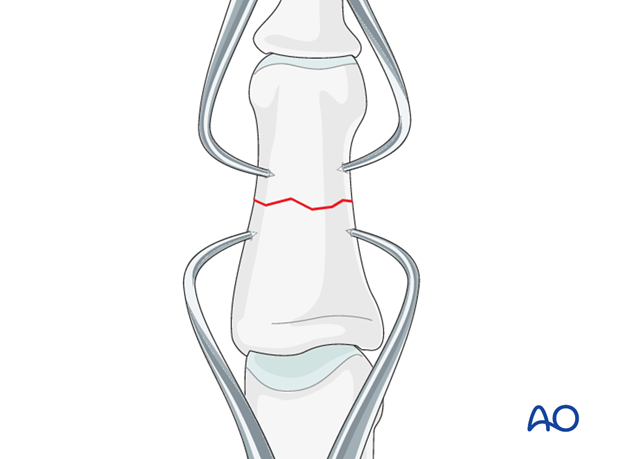
Direct reduction
Direct reduction is necessary when the fracture can not be reduced by traction and flexion, or is unstable.
When indirect reduction is not possible, this is usually due to interposition of parts of the extensor apparatus.
Use two pointed reduction forceps for direct reduction.
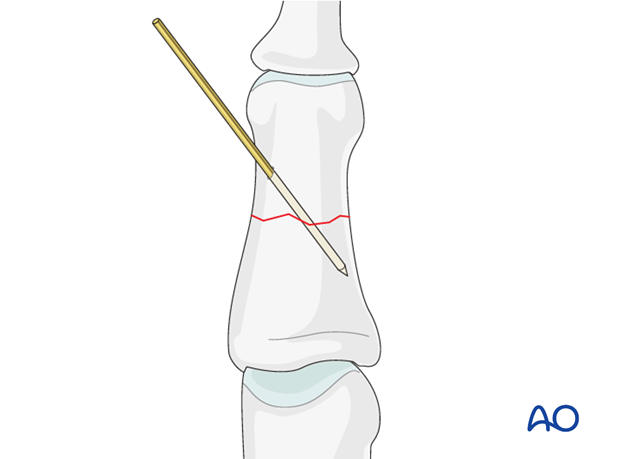
Preliminary fixation
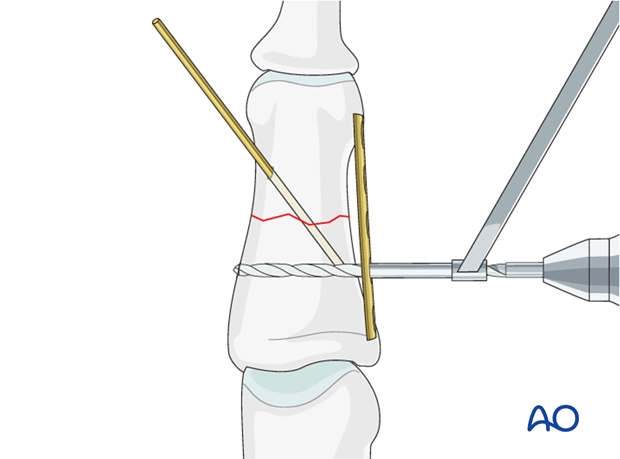
Insert a K-wire for provisional fixation.
4. Check alignment
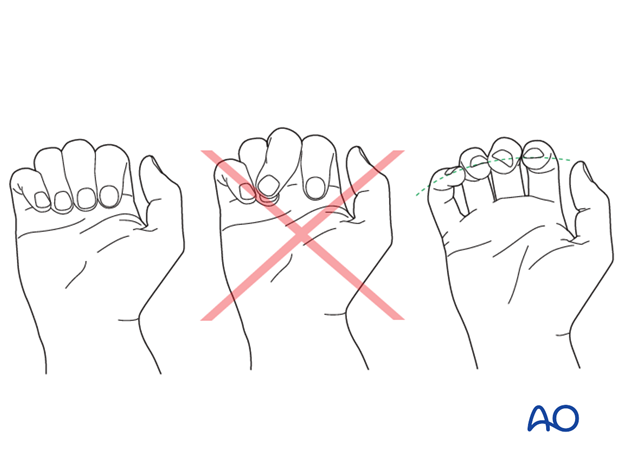
Identifying malrotation
At this stage, after provisional fixation, it is advisable to check the alignment and rotational correction by moving the finger through a range of motion.
Rotational alignment can only be judged with the fingers in a degree of flexion, and never in full extension. Malrotation may manifest itself by overlap of the flexed finger over its neighbor. Subtle rotational malalignments can often be judged by tilting of the leading edge of the fingernail, when the fingers are viewed end-on.
If the patient is conscious and the regional anesthesia still allows active movement, the patient can be asked to extend and flex the finger.
Any malrotation is corrected by direct manipulation and later fixed.
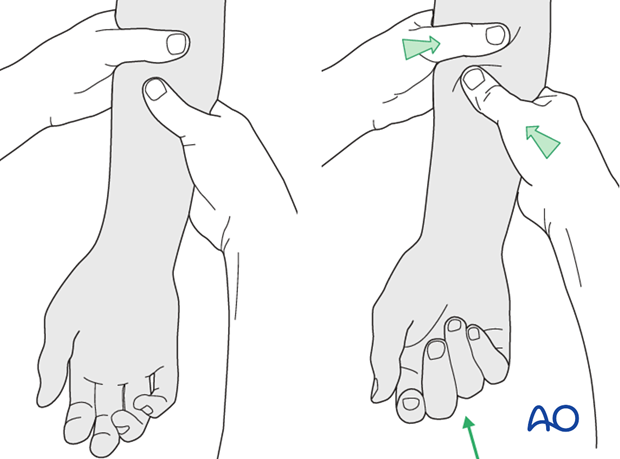
Using the tenodesis effect when under anesthesia
Under general anesthesia, the tenodesis effect is used, the surgeon fully flexing the wrist to produce extension of the fingers, and fully extending the wrist to cause flexion of the fingers.
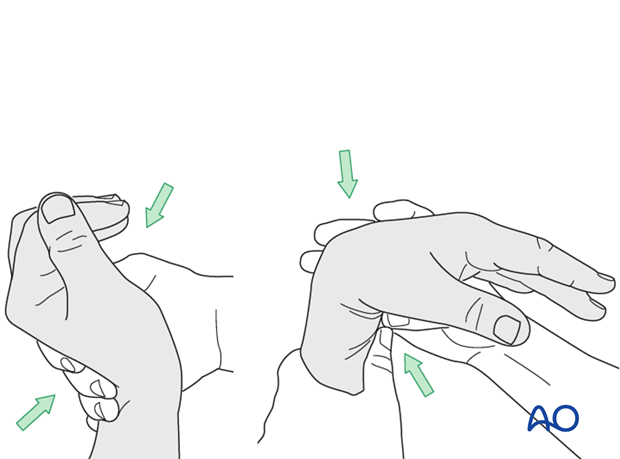
Alternatively, the surgeon can exert pressure against the muscle bellies of the proximal forearm to cause passive flexion of the fingers.
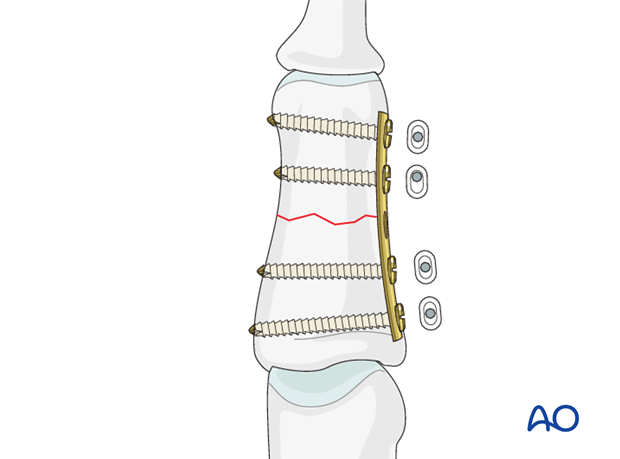
5. Fixation: Conventional plate
Bending and contouring the plate
If the plate is perfectly contoured to follow the geometry of the concavity of the phalanx, tightening the screws will result in a gap in the opposite cortex.
The solution to this is slightly to overbend the plate so that when axial compression is exerted by the plate, the compression occurs evenly over the whole fracture surface.
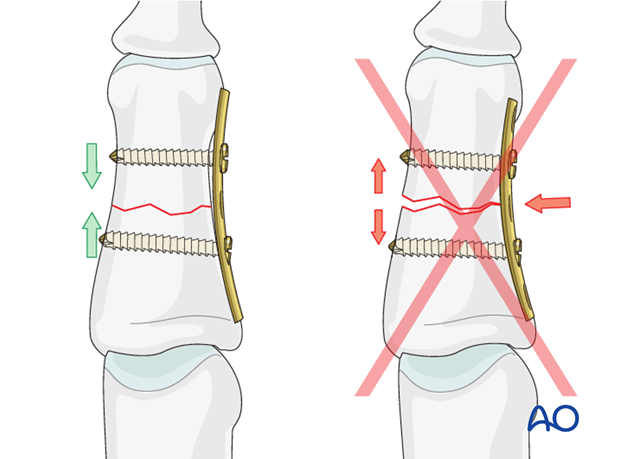
Plate application
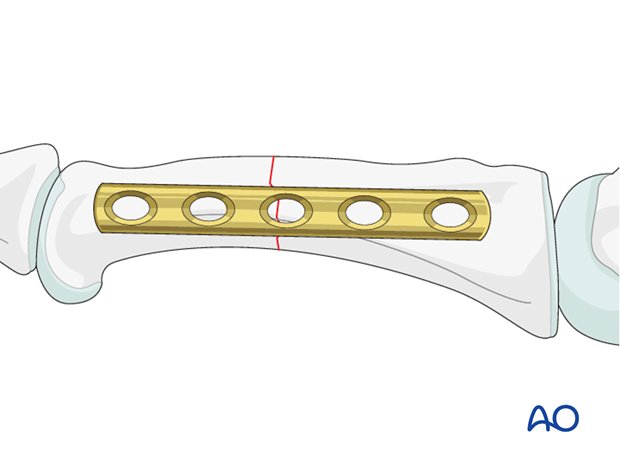
Select a plate with at least 4-5 holes, and center it over the fracture.
Ensure that the plate is centered on the long axis of the diaphysis in the lateral view.
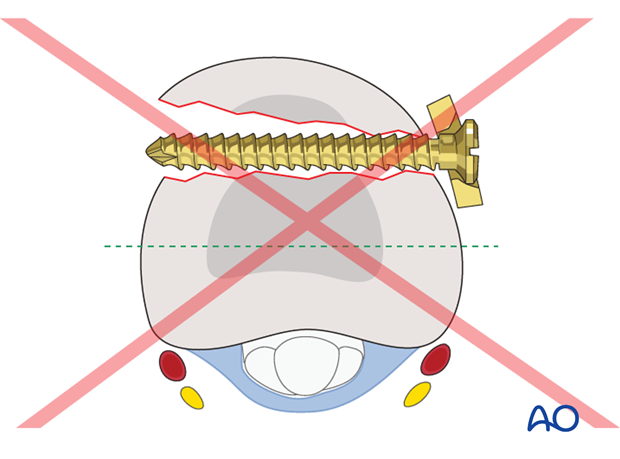
Pitfall
If the plate is not properly aligned in the lateral view, the screws may not cross the medullary canal and may not have sufficient purchase. Secondary fractures may result.
Drilling
Using a drill guide, carefully drill a first hole with a 1.1 mm drill bit.
Measurement
Use a depth gauge to determine screw length.
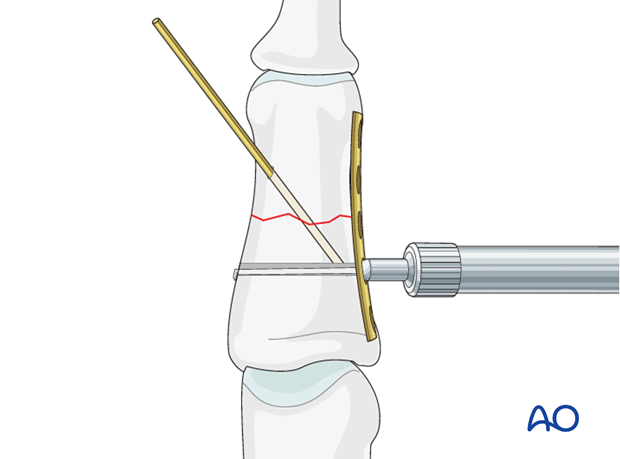
Screw insertion
Insert the first screw in a neutral position. Ensure that it engages the far cortex. Failure accurately to measure the required screw length risks failure to engage the far cortex properly, weakens the fixation, and incurs the risk of implant failure.
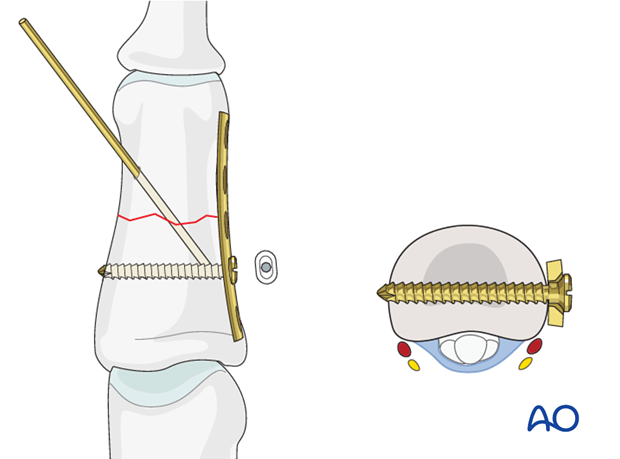
Insert second screw
Insert a second screw in a neutral position on the same side of the fracture after the same fashion as above.
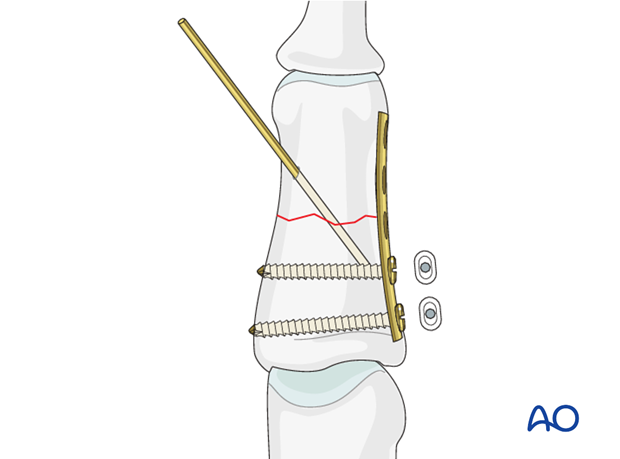
Insert third screw eccentrically
Drill eccentrically for the third screw, through the proximal hole on the other side of the fracture. Measure for screw length, and insert a screw.
Tightening this screw will compress the fracture axially.
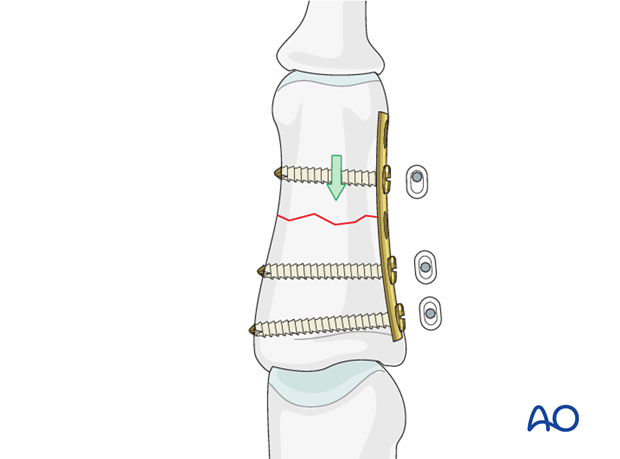
Complete fixation
Complete the fixation with the insertion of a neutral fourth screw, after the fashion of the first two screws.
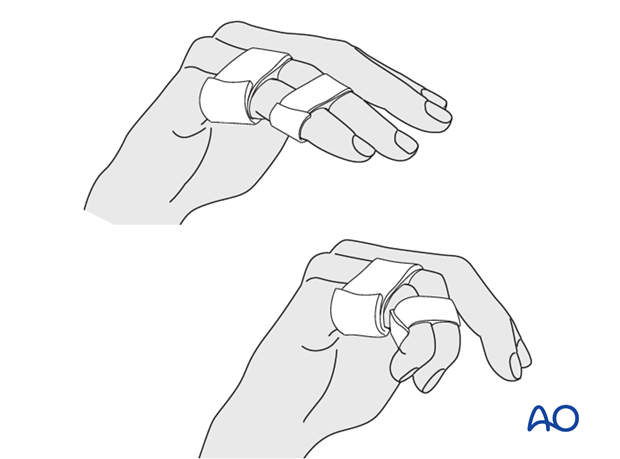
6. Aftertreatment
Postoperatively
Protect the digit with buddy strapping to the adjacent finger, to neutralize lateral forces on the finger.
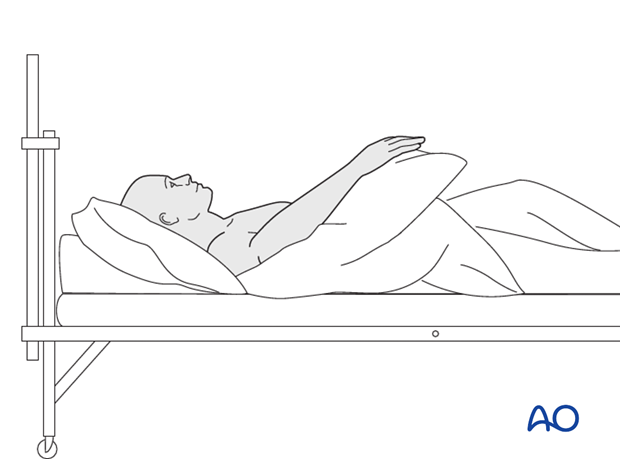
While the patient is in bed, use pillows to keep the hand elevated above the level of the heart to reduce swelling.
Follow up
See the patient 5 days and 10 days after surgery.
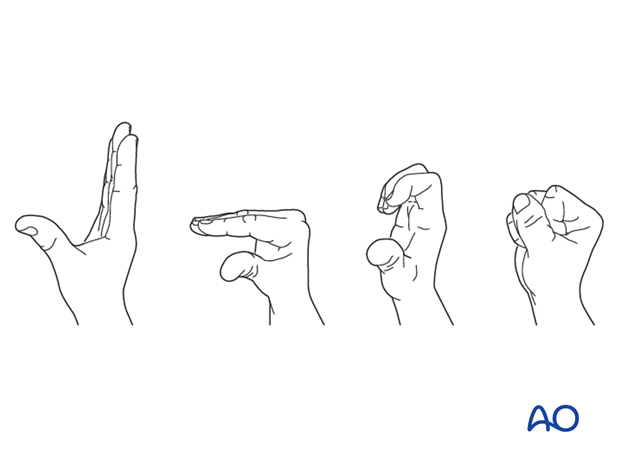
Functional exercises
The patient can begin active motion (flexion and extension) immediately after surgery.
For ambulant patients, put the arm in a sling and elevate to heart level.
Instruct the patient to lift the hand regularly overhead, in order to mobilize the shoulder and elbow joints.

Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness, or tendon adhesion’s restricting finger movement, tenolysis, or arthrolysis become necessary. In these circumstances, take the opportunity to remove the implants.












