Volar plate arthroplasty
1. Principles
Classification of avulsion fractures of the volar plate
Avulsion fractures of the volar plate are very common injuries, often resulting from sporting injuries and usually involving the middle and ring fingers. Several classification systems for them have been proposed. The Eaton classification is very useful for practical purposes. This classification is based on the premise that successful treatment must be based on the stability of the fracture, which in turn depends on:
- size of the fragment
- degree of impaction,
- presence of one or both collateral ligament ruptures
- direction of the dislocation (hyperextension, lateral dislocation, flexion).
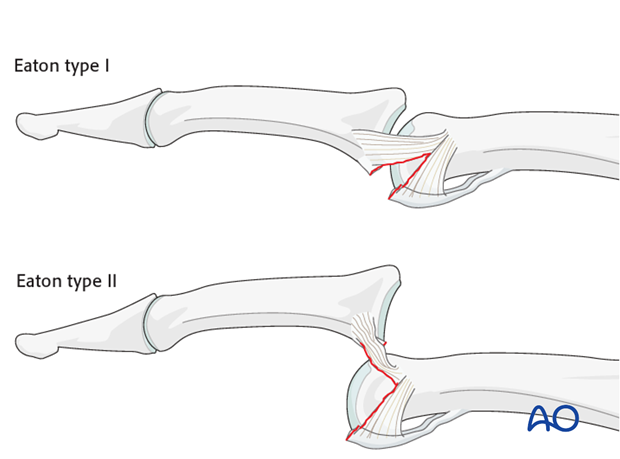
Eaton type I (hyperextension)
These are hyperextension injuries, with an avulsion of the volar plate without fracture, and a longitudinal split in the collateral ligaments.
Eaton type II (dorsal dislocation)
Complete dorsal dislocation of the PIP joint and volar plate avulsion without fracture. The base of the middle phalanx rests dorsally on the condyles of the proximal phalanx, with no contact between the articular surfaces.
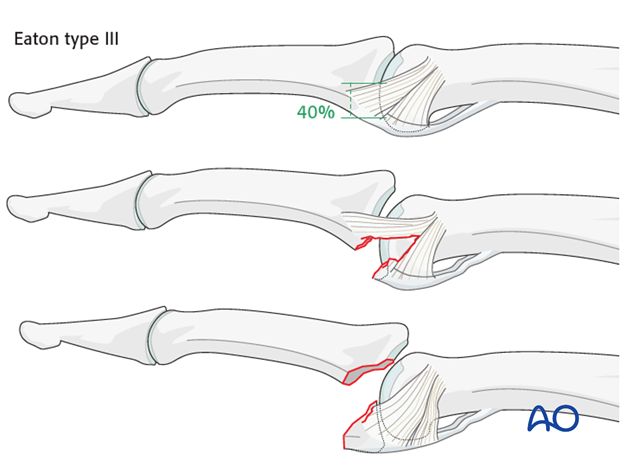
Eaton type III (fracture subluxation)
A fracture subluxation with a palmar marginal fragment of variable size.
Stability of fracture dislocations (Eaton type III)
Stability of the reduction depends on the size of the avulsed palmar marginal fragment and the amount of collateral ligament remaining attached to the middle phalanx.
If less than 40% of the joint surface is avulsed, the fracture is displaced dorsally, with the dorsal portion of the collateral ligament remaining attached to the middle phalanx. This helps to keep the reduction stable.
However, if more than 40% of the joint surface has been avulsed, very little or no ligament will remain attached to the base of the middle phalanx, rendering reduction unstable.
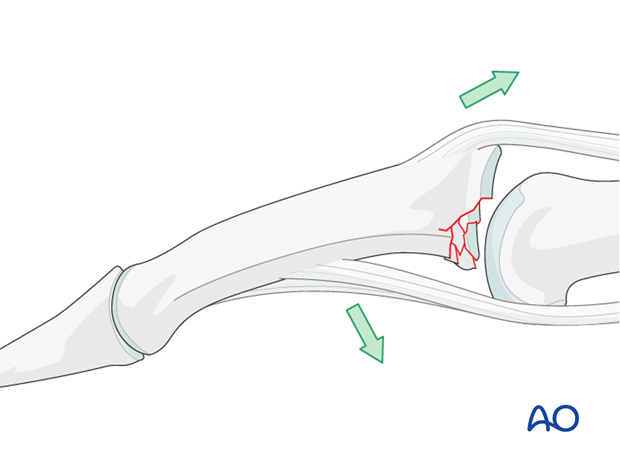
Mechanism of the injury
These digital hyperextension injuries are commonly caused by sporting accidents.
Typically, hyperextension of the proximal interphalangeal (PIP) joint causes an avulsion fracture of the volar plate.
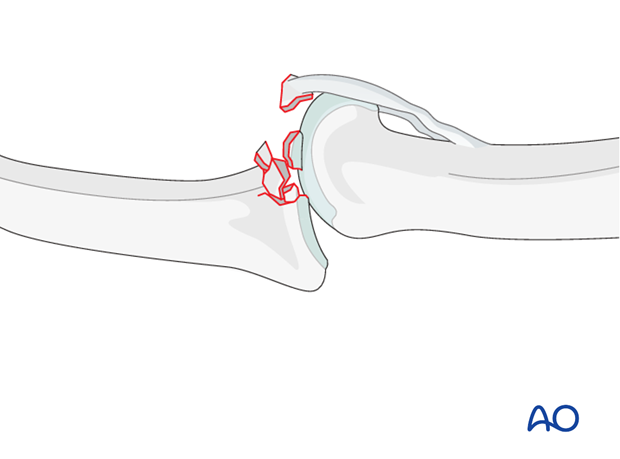
Often, in addition to hyperextension, there is axial load on the middle phalanx, causing compression forces across the PIP joint and leading to an additional impaction fracture.

Deforming forces
In the presence of palmar instability of the PIP joint, muscle forces (flexor digitorum superficialis and the central extensor slip) lead to palmar tilting and dorsal subluxation, depending on the degree of the impaction.
Recognizing subluxation
Diagnosis is based on:
- the clinical history and mechanism of injury
- the clinical examination of the patient
- the x-rays
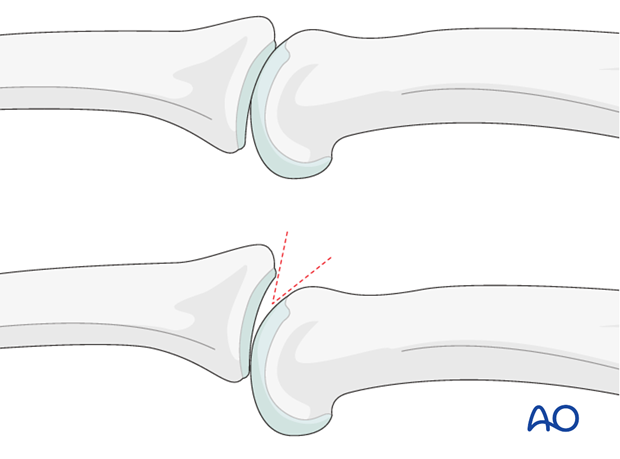
AP and true lateral x-rays are necessary for diagnosis. Be careful to avoid overlap of other fingers in the x-rays.
An AP view will help to detect impaction fractures.
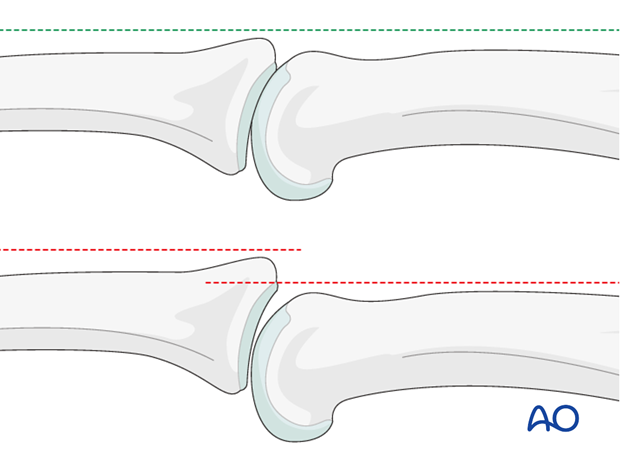
Often, a subluxation is not easily recognized in the lateral view. Look for the characteristic “V” sign of diverging joint surfaces, which indicates this injury.
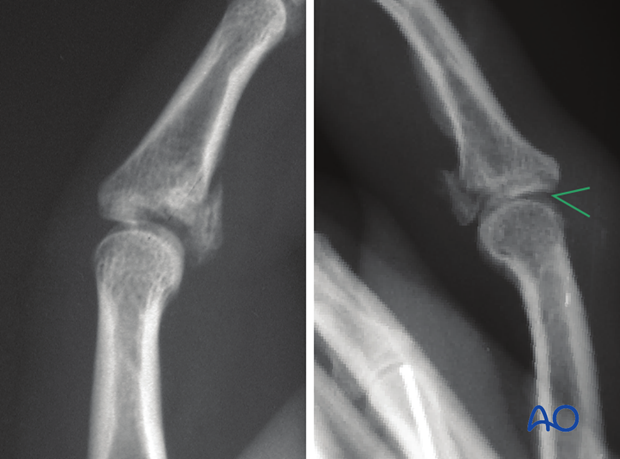
In the lateral view, the proximal and middle phalanges should be collinear. Any break in the dorsal line is a clear indication of subluxation.
Check for impaction injuries
Impaction is possible both in the sagittal and the coronal planes. Check both true AP and lateral views.
Volar plate arthroplasty
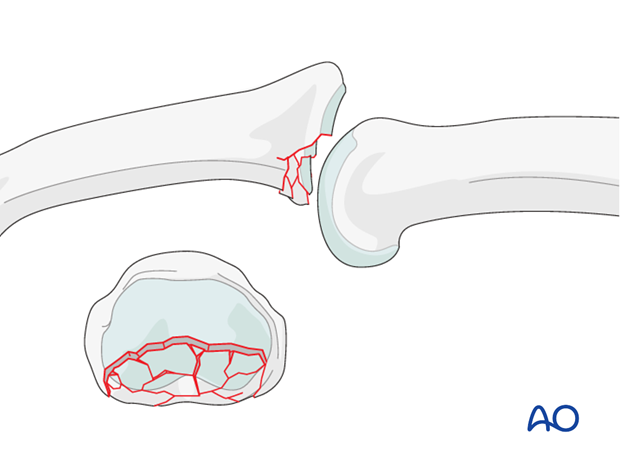
Extensive comminution of the palmar margin is the main indication for volar plate arthroplasty of the PIP joint.
The degree of comminution is often not apparent on the x-rays. These fractures are usually associated with impaction in the subchondral metaphysis.
The more impaction and comminution is present, the less stable is the joint.
These fractures can not be treated by internal fixation. Volar plate arthroplasty is a good option for these fractures.
In order for volar plate arthroplasty to be used, at least 60% of the dorsal articular surface needs to be intact. Loss of more than 40% of the articular cartilage is a contraindication for this procedure, and bone graft reconstruction becomes necessary.
Alternatively, a hinged external fixator may be used.
2. Approach
For this procedure a palmar approach to the PIP joint is normally used.
3. Resection
Visualize the joint
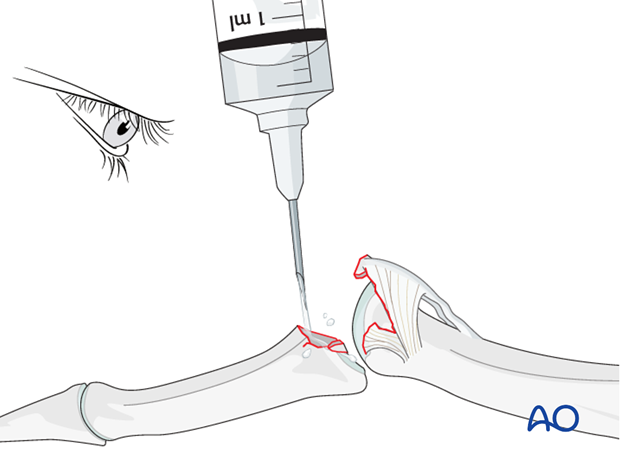
Hyperextend the middle phalanx to gain maximal visualization of the joint.
Use a syringe to clean out blood clots with a jet of Ringer lactate fluid.
Often the degree of comminution is not apparent from the x-rays, and can only be determined under direct vision.
Remove all loose bony fragments.
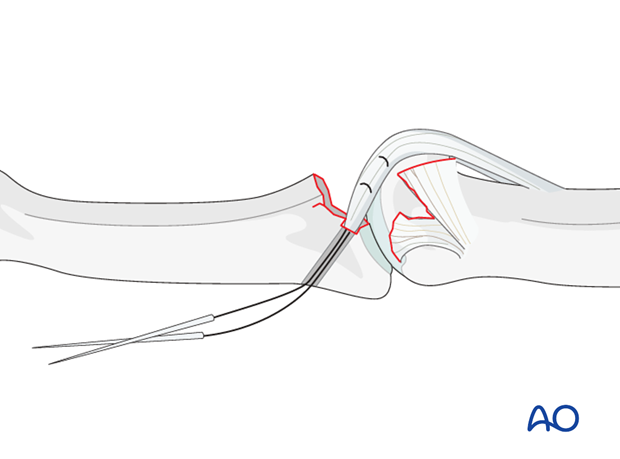
Incise collateral ligament
Incise the interval between the volar plate and the accessory collateral ligament.
This will allow mobilization (advancement) of the volar plate.
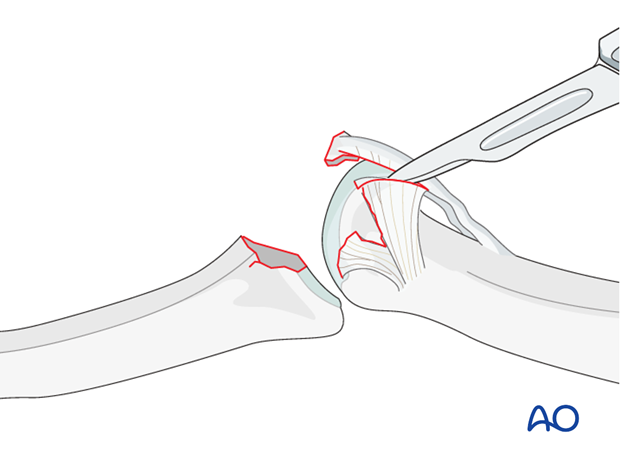
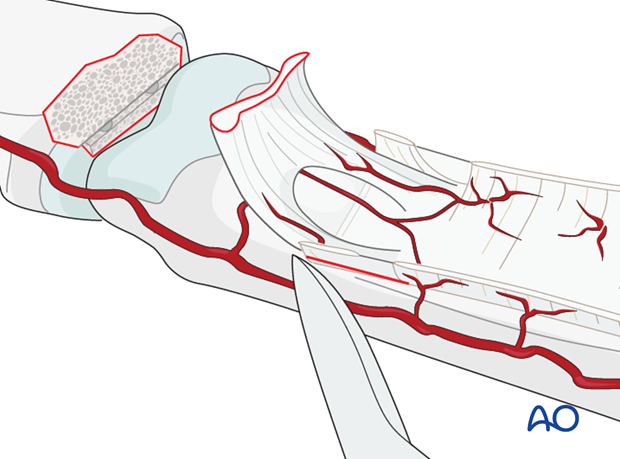
Removal of fragments
A scalpel is then used to dissect any sizable remaining fracture fragment from the volar plate. Preserve as much of the volar plate as possible.

4. Suture the volar plate
Make a transverse groove
Using a fine rongeur, shape a transverse groove in the subchondral bone at the base of the middle phalanx.
The groove must be perpendicular to the long axis of the middle phalanx in order to avoid lateral angulation.
This groove will later be used to reattach the distal edge of the volar plate.

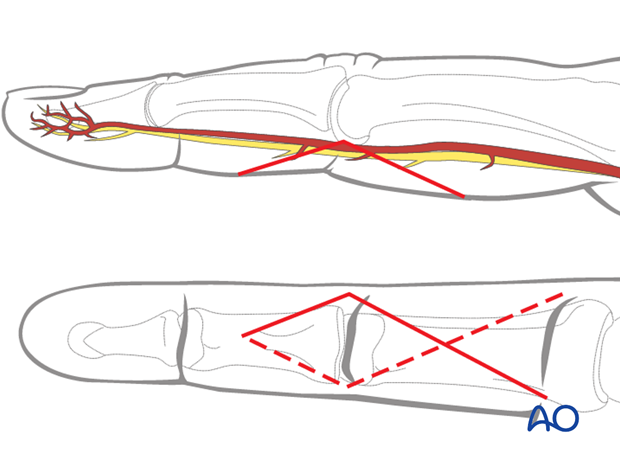
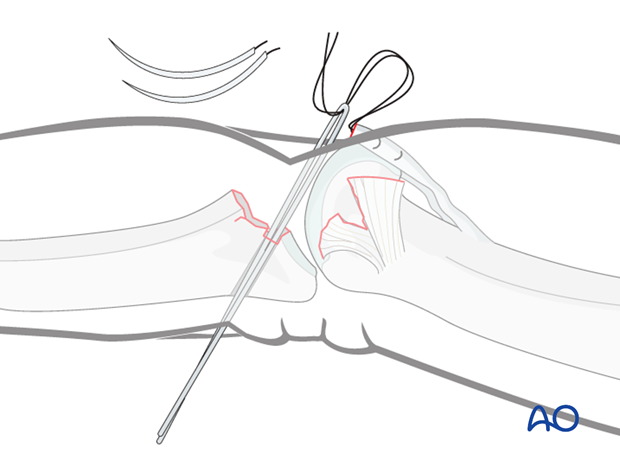
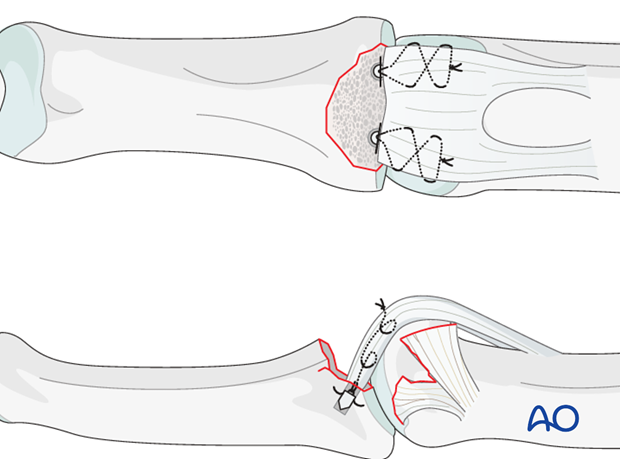
Bunnell-crisscross suture in the volar plate
Use fine multifilament sutures with double-mounted straight needles to insert a criss-cross stitch (Bunnell) in each side of the volar plate on both sides from distal to proximal and back.

Drilling
Keeping the phalanx hyperextended, drill holes for the needles in the ulnar and radial endsof the transverse groove. It is essential to use a drill guide in order to protect the cartilage of the condyles.
The drill holes must just perforate the dorsal cortex of the middle phalanx.
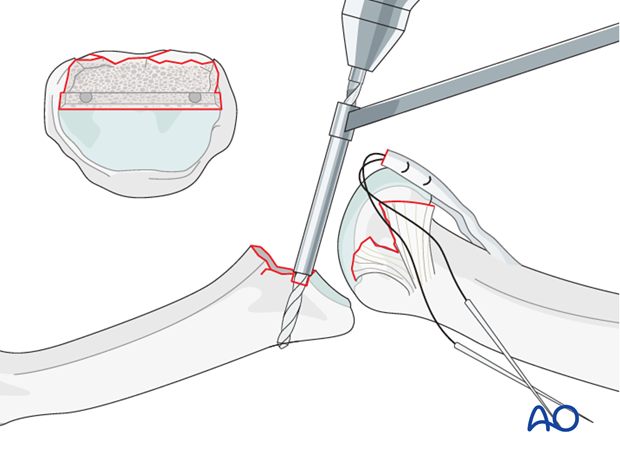
Remember that the drill holes must be positioned as close to the articular cartilage as possible in order to prevent later subluxation.
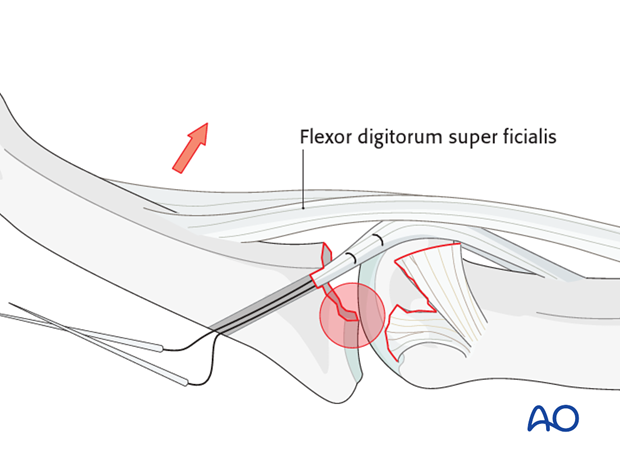
Pitfall: drill holes too far from cartilage
If the drill holes are not immediately adjacent to the articular cartilage, the pull of the flexor digitorum superficialis (FDS) will cause dorsal subluxation.
Degenerative joint disease may also develop as a later consequence.
Dorsal incision
Make a dorsal incision of about 1 cm distal to the insertion of the central extensor slip, incising the triangular ligament.
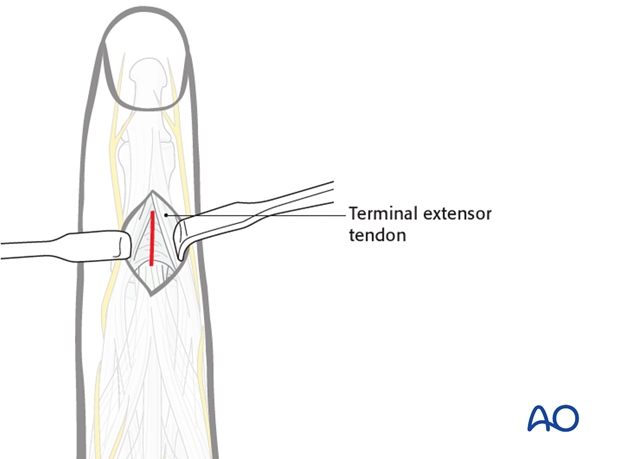
Insert needles
Now thread the needles through the holes so that they exit through the dorsal incision.
Alternative threading technique
If straight needles are not available, insert fine wire loops from the dorsal aspect through the drill holes. Cut off the curved needles and pass the suture threads through these wire loops on both sides. Pull the wire loops out dorsally, thereby drawing the suture threads through the holes.
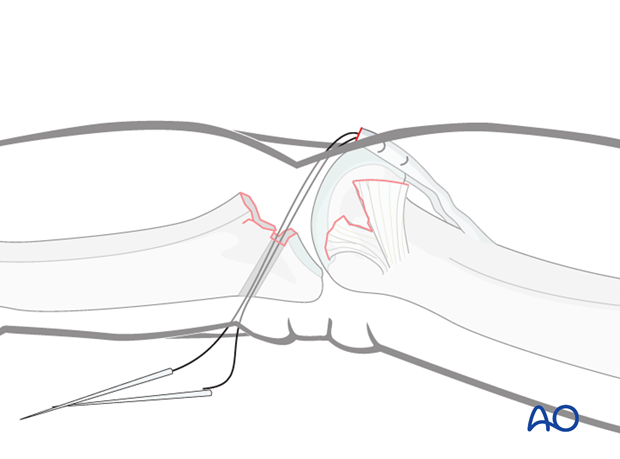
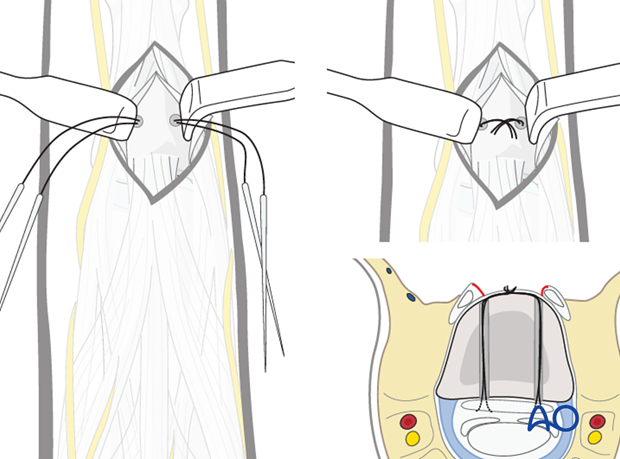
Secure volar plate to groove
Traction on the four suture threads will draw the volar plate securely into the groove.
Confirm that the volar plate has entered the prepared groove.
Confirm reduction and joint congruency using image intensification.
Tighten the sutures
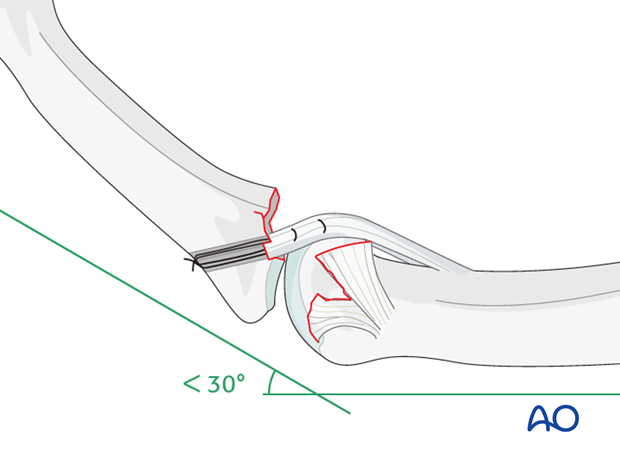
After confirming that the volar plate is not too short, and that fixed flexion does not exceed 30 degrees, tighten the sutures over the dorsal cortex of the middle phalanx.
Resuture the triangular ligament, if possible.
If the volar plate is shortened
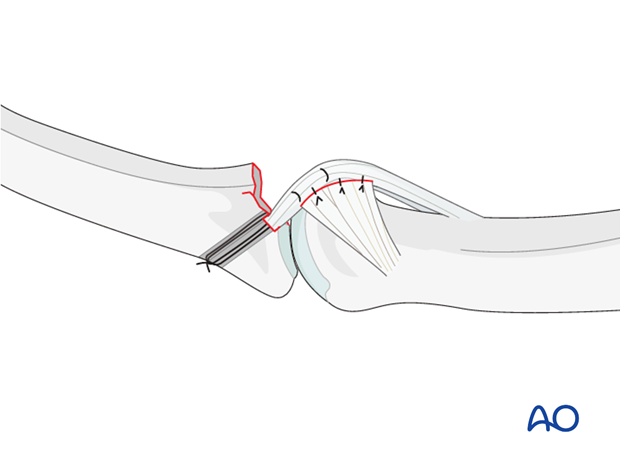
If treatment is delayed, the volar plate is often shortened and can not reach the groove. In such a case, the check-reins need to be mobilized, as illustrated.
Pitfall: too much flexion
If the volar plate is shortened, it is not acceptable to flex the finger by more than 30 degrees in order that it reach the groove. If the surgeon has to flex the finger further, then a flexion contractor is likely to develop.
The only options in this event would be the use of a hinged external fixator, or even primary arthrodesis.
Resuture the accessory collateral ligament
If there is lateral instability, resuturing of the accessory collateral ligament to the volar plate is recommended.
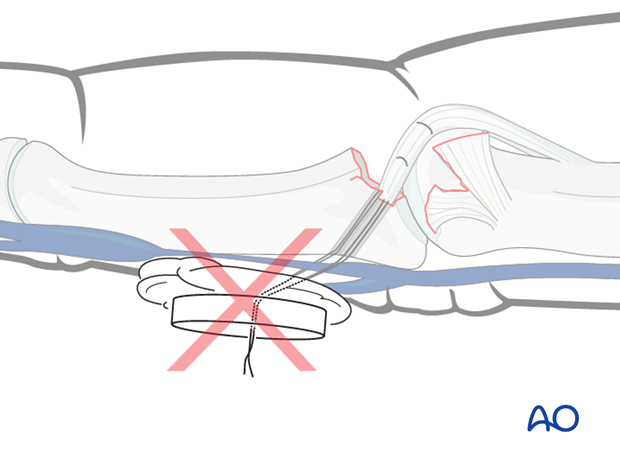
Pitfall: pull-out suture with button
Traditionally, a button has often been used for tying the pull-out sutures. However, the pressure the button exerts on the dorsal veins of the finger can lead to swelling. It is safer to omit the button, simply tying the suture over the bone.
Alternative: use suture anchors
As an alternative to the described method, suture anchors, inserted immediately adjacent to the articular cartilage on both sides, can also be used.
5. Maintaining joint congruency
Transfixation of the PIP joint
In case of persistent instability, obliquely insert a K-wire transfixing the PIP joint to keep the finger in 20-30 degrees of flexion.
This K-wire should be removed after 3-4 weeks.
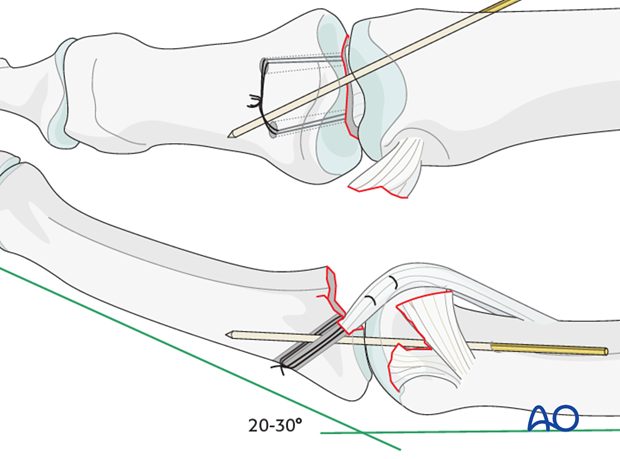
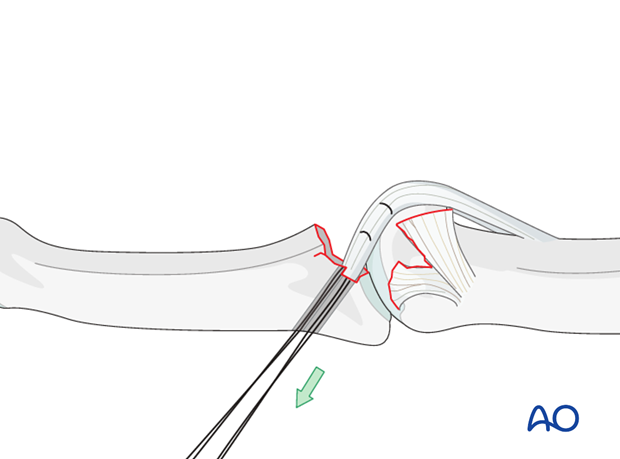
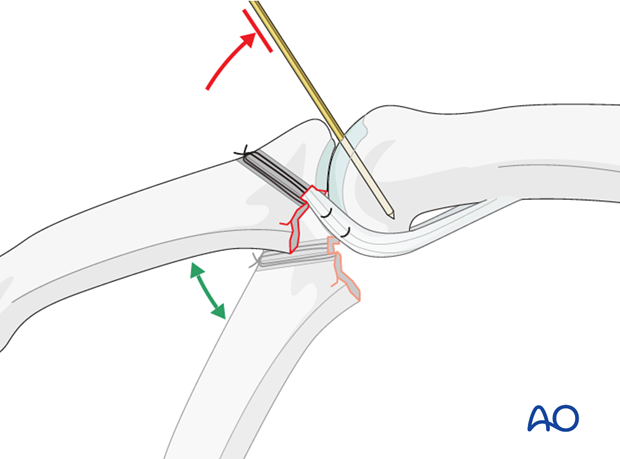
Extension block K-wire
A K-wire is introduced between the condyles of the proximal phalanx, in order to block the last 20-30 degrees of extension, but allowing full flexion.
This prevents dorsal subluxation and allows for immediate mobilization of the PIP joint.
This K-wire should be removed after 3-4 weeks.
6. Aftertreatment
Aftertreatment should be performed under supervision of a hand therapist.
DIP and MCP joint movement is encouraged immediately to avoid extensor tendon adhesion and joint stiffness. If there is no transfixation of the PIP joint, active flexion of the PIP joint is initiated immediately postoperatively. A dorsal extension block splint at 30 degrees of flexion is used for 4 weeks.
A Coban bandage to reduce swelling is recommended.
Dynamic extension splinting
If after 5 weeks there is no full active extension, dynamic extension splinting is recommended.
The recovery process after such injuries is slow. Reassure the patient to expect 8-12 months to achieve the final result.













