Suture fixation
1. Principles
Classification of avulsion fractures of the volar plate
Avulsion fractures of the volar plate are very common injuries, often resulting from sporting injuries and usually involving the middle and ring fingers. Several classification systems for them have been proposed. The Eaton classification is very useful for practical purposes. This classification is based on the premise that successful treatment must be based on the stability of the fracture, which in turn depends on
- size of the fragment
- degree of impaction,
- presence of one or both collateral ligament ruptures
- direction of the dislocation (hyperextension, lateral dislocation, flexion).
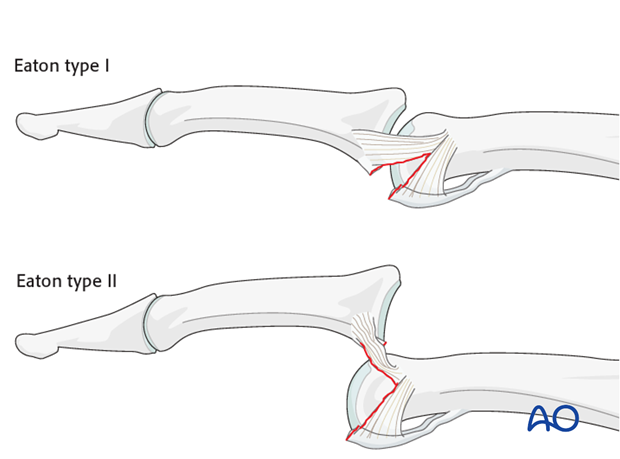
Eaton type I (hyperextension)
These are hyperextension injuries, with an avulsion of the volar plate and a longitudinal split in the collateral ligaments.
Eaton type II (dorsal dislocation)
Complete dorsal dislocation of the PIP joint and avulsion of the volar plate. The base of the middle phalanx rests dorsally on the condyles of the proximal phalanx, with no contact between the articular surfaces.
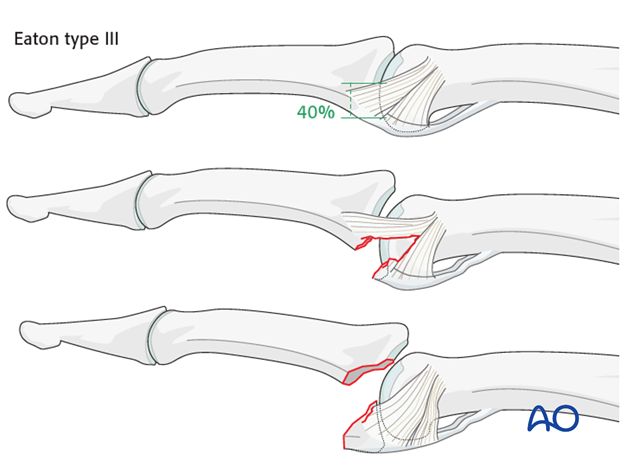
Eaton type III (fracture dislocation)
A fracture dislocation with a small fragment measuring less than 40% of the palmar arc will remain stable when reduced.
If a larger part (>40%) of the palmar articular segment is involved, ligamentous support will not suffice for a stable reduction.
Stability of fracture dislocations (Eaton type III)
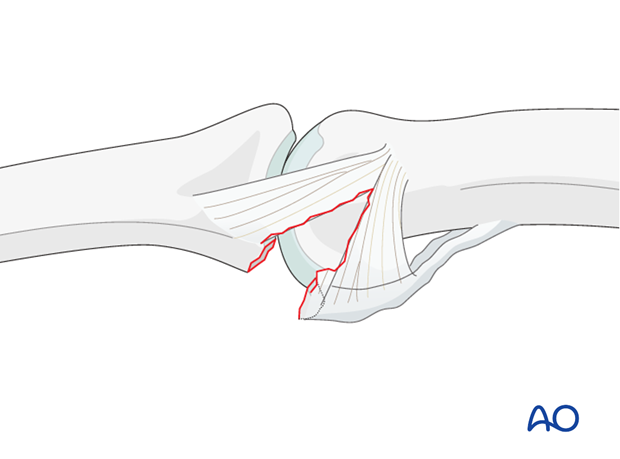
Stability of the reduction depends on the size of the avulsed fragment and the amount of ligament remaining attached to the middle phalanx.
If less than 40% of the articular segment is avulsed, the fracture is displaced dorsally, with the dorsal portion of the collateral ligament remaining attached to the middle phalanx. This helps to keep the reduction stable.
However, if more than 40% of the articular segment has avulsed, only very little or no ligament will remain attached to the base of the middle phalanx, rendering the reduction unstable.
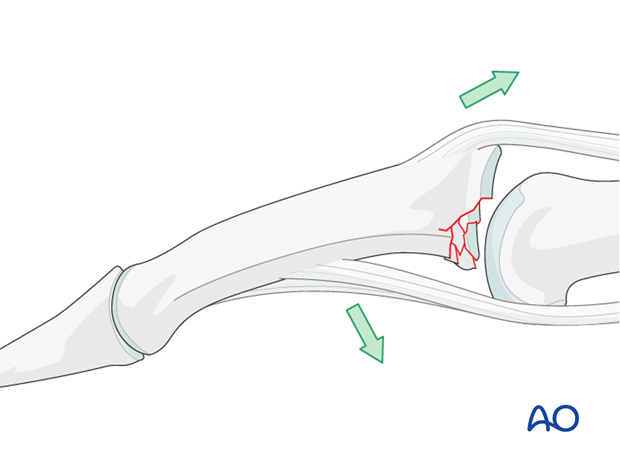
Mechanism of the injury
These injuries are commonly caused by sporting accidents.
Typically, hyperextension of the finger causes an avulsion fracture of the volar plate.
Often, in addition to hyperextension, pressure is applied to the fingertips, causing longitudinal compression forces on the middle phalanx towards the proximal phalanx and leading to an additional impaction fracture.

Deforming forces
The flexor digitorum superficialis (FDS) exerts a palmar pull on the middle phalanx around a pivotal point determined by the junction of intact cartilage and the fracture, which leads to subluxation and dorsal tilting, depending on the degree of the impaction.
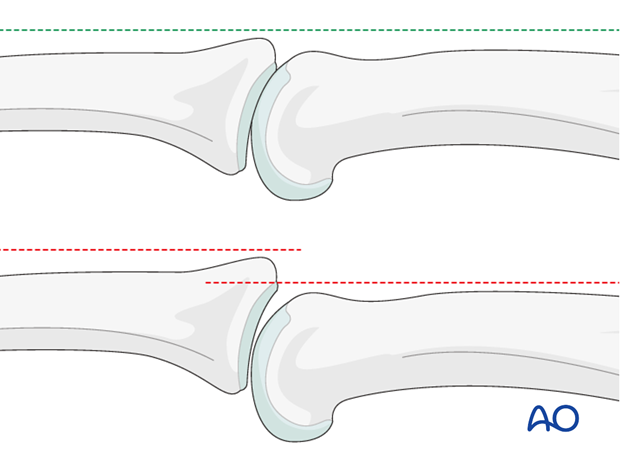
Recognizing subluxation
Diagnosis is based on
- the clinical history of the trauma and mechanism of the injury
- the clinical examination of the patient
- the x-rays
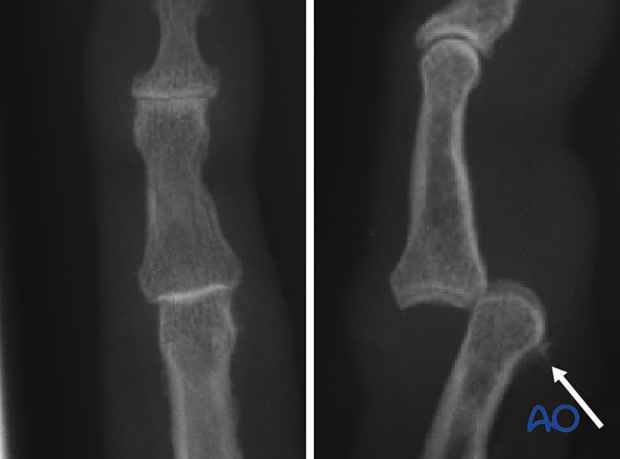
AP and lateral x-rays are necessary for diagnosis. Be careful to avoid interposition of other fingers in the x-rays.
An AP view will help to recognize impaction fractures.
Often, a subluxation is not apparent on the lateral view. Look for the characteristic “V” sign of diverging joint surfaces, which indicates this injury.
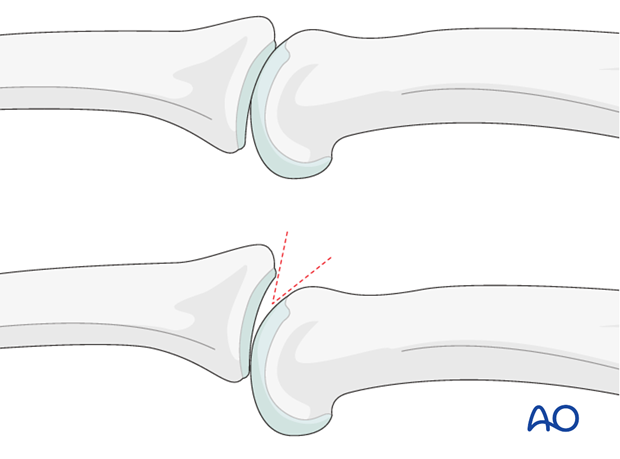
In the lateral view, the proximal and middle phalanges should be collinear. Any axial malalignment is a clear indication of subluxation.
2. Indications
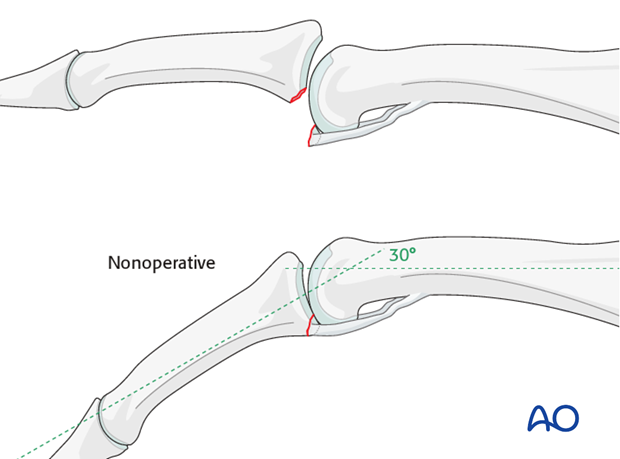
Indication for nonoperative treatment
Ask the patient to flex the finger under image intensification.
If reduction of the avulsion fracture is achieved with less than a 30 degree bend, nonoperative treatment may be a good choice.
However, if it takes more than 30 degrees of bending, operative treatment is indicated.
Reduction will not be achieved if tissues are interposed between the fracture fragments. This, too, is an indication for surgical treatment.
Passive lateral movement of the finger under image intensification will help to assess lateral stability.
Small-fragment avulsion fracture
When the avulsed fragment is very small (<30% of the articular segment), nonoperative treatment is usually a good choice.
Irreducible fracture – operative treatment
In some cases, the fracture can not be reduced due to interposed tissues, or blood clot.
In these cases, internal fixation is indicated.
As the use of a lag screw could easily shatter a small fragment, internal fixation with sutures is a good choice in such fractures.
3. Approach
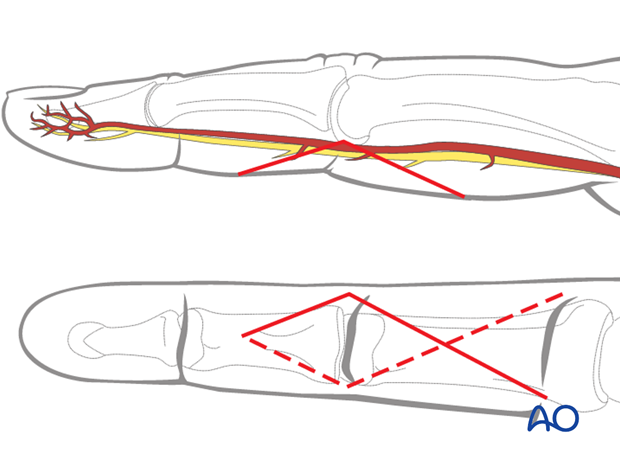
For this procedure a palmar approach to the PIP joint is normally used.
4. Visualize the Joint
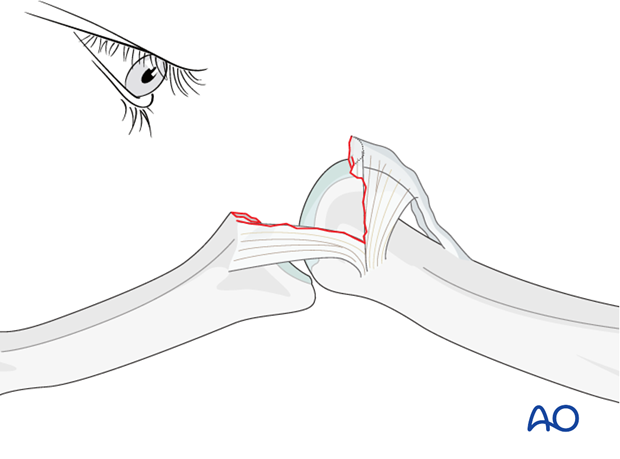
Hyperextend the middle phalanx to gain a maximal view of the joint.
In order to gain better view of the fracture, use a syringe to clear out blood clot with a jet of Ringer lactate.
Assess fracture geometry and look for comminution or impaction, which may not be apparent from the x-rays and can only be determined under direct vision.
5. Fixation
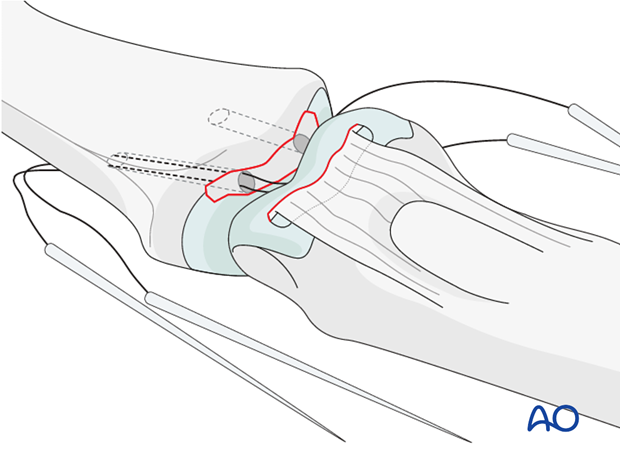
Drilling
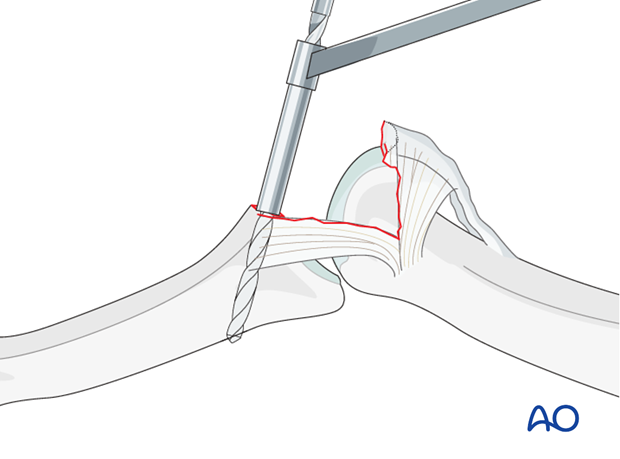
Keeping the phalanx hyperextended, drill holes for the needles in the ulnar and radial sides of the in the base of the middle phalanx.
Each drill hole must be placed halfway between the palmar and dorsal edges of the fracture surface
It is mandatory to use a drill guide to protect the cartilage of the condyles.
The drill holes must perforate the dorsal cortex of the middle phalanx.
Drill holes
Always choose the diameter of the drill holes corresponding to the width of the small avulsed fragment. If the drill holes are too small, reduction may be prevented by interposing sutures.
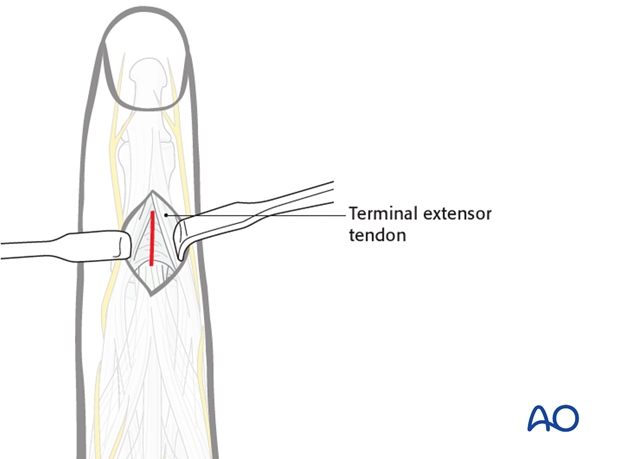
Dorsal incision
Make a dorsal incision of about 1 cm, distal to the insertion of the central slip, incising the triangular ligament.
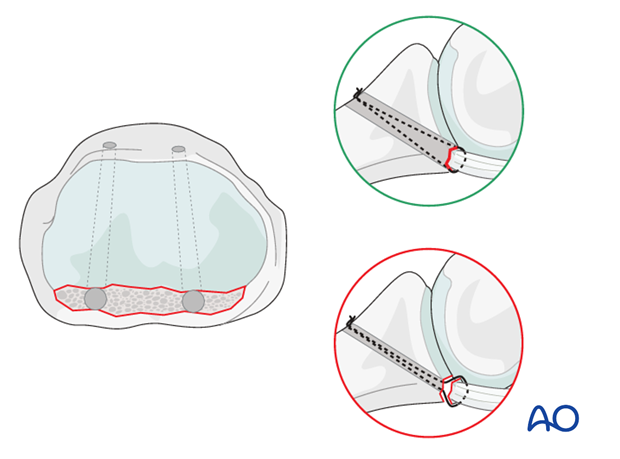
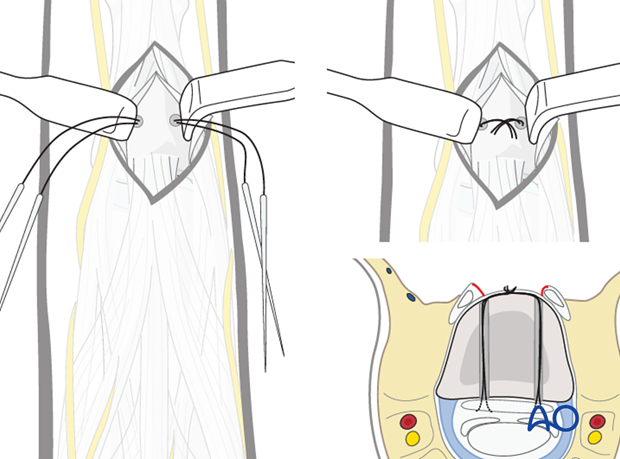
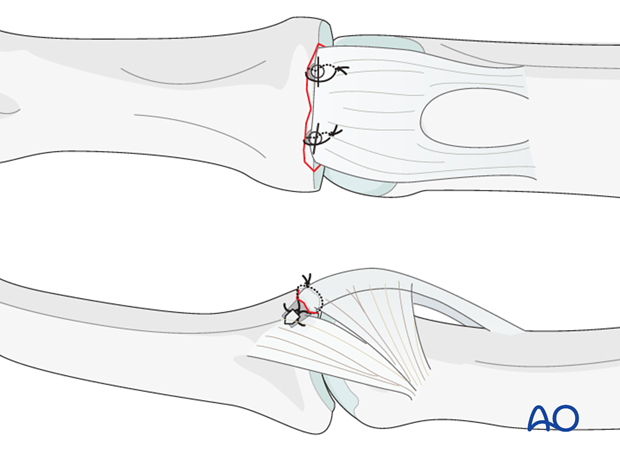
Insert sutures
Use 4.0 multifilament nonabsorbable sutures with double-mounted straight needles.
Wrap each suture around the small fragment attached to the volar plate, and insert the two ends of each suture through its drill hole. Both needles should exit dorsally through the skin incision.
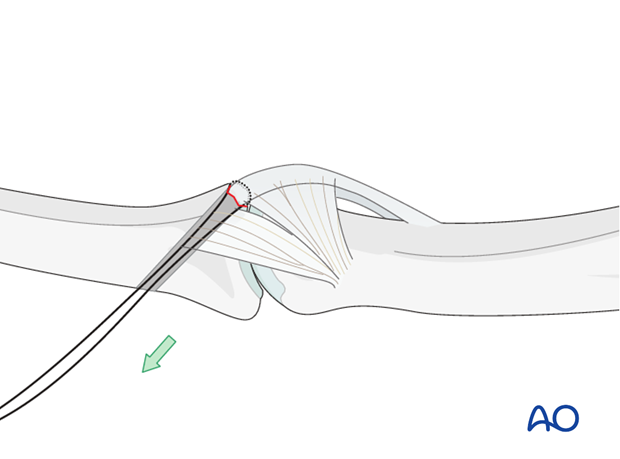
Reduce fracture
Now gently reduce the fracture by pulling on the sutures in a dorsal direction.
Confirm anatomical reduction using image intensification.
Tighten the sutures
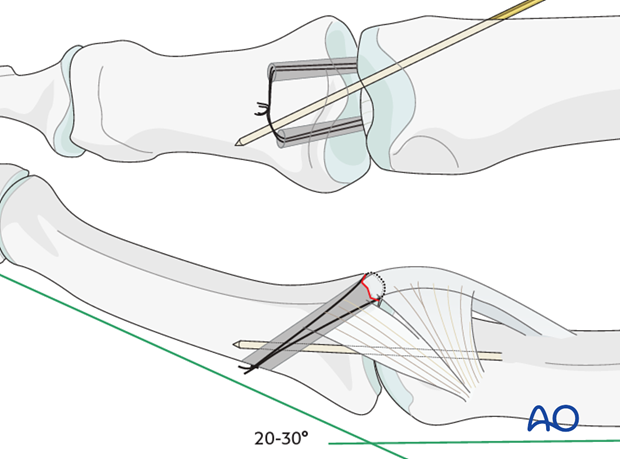
After confirming that the volar plate is not too short, and that fixed flexion does not exceed 30 degrees, tighten the sutures over the dorsal cortex of the middle phalanx.
Resuture the triangular ligament, if possible.
6. Alternative fixation
Suture anchors
Alternatively to the described method, suture anchors can be used.
7. Check stability of fixation
Check the stability of the fixation by extending the PIP joint.
In case of any joint instability, insert a K-wire crossing the joint obliquely with the finger in 20-30 degrees of flexion.
8. Aftertreatment
DIP joint movement is encouraged immediately to avoid extensor tendon adhesion.
Implant removal
When a K-wire has been used, it is removed after 3 weeks. X-rays are taken to confirm articular congruency. Unlimited flexion is encouraged after wire removal.
Functional exercises
Active flexion of the PIP joint is initiated by using a dorsal extension block splint at 30 degrees. This will need to be delayed until any K-wire has been removed.
After 4 weeks, the splint is removed, and unrestricted active extension is permitted.
Dynamic extension splinting
If after 5 weeks active extension is not full, dynamic extension splinting is recommended.
During the whole process, after removal of any K-wire, the hand therapist should closely monitor the rehabilitation.
The recovery process after such injuries is slow. Warn the patient to expect 6-8 months for full recovery.













