Screw fixation of lateral plateau compression fracture
1. Principles
Dislocations
While dislocations and ligament injuries are common throughout the hand, they are most common at the proximal interphalangeal (PIP) joint.
The spectrum of these injuries ranges from minor stretching (sprains) to complete disruptions of the ligaments.
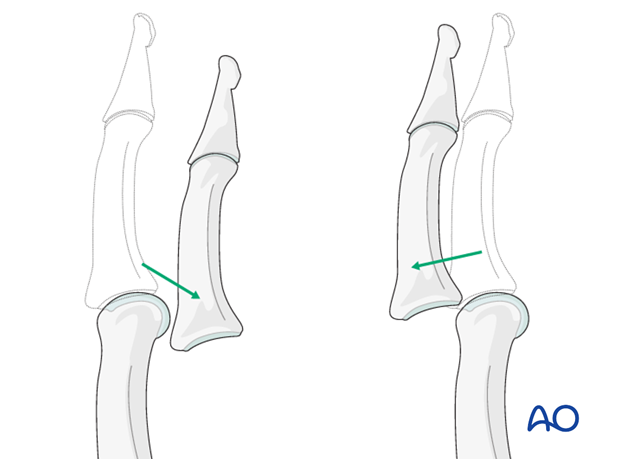
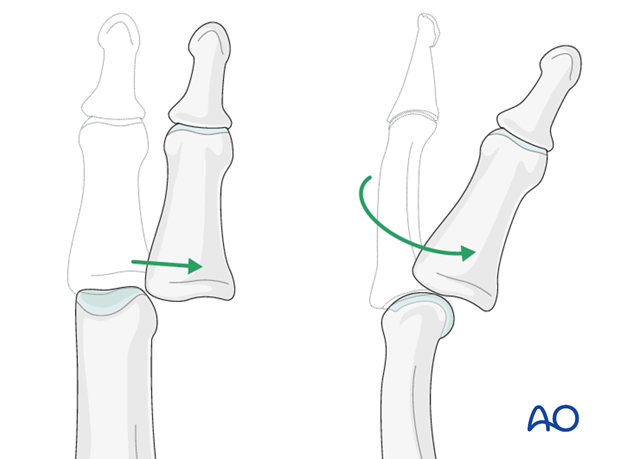
Dislocations of the PIP joint are classified according to the direction of displacement of the middle phalanx. They can be palmar, dorsal, lateral, or lateral rotatory.
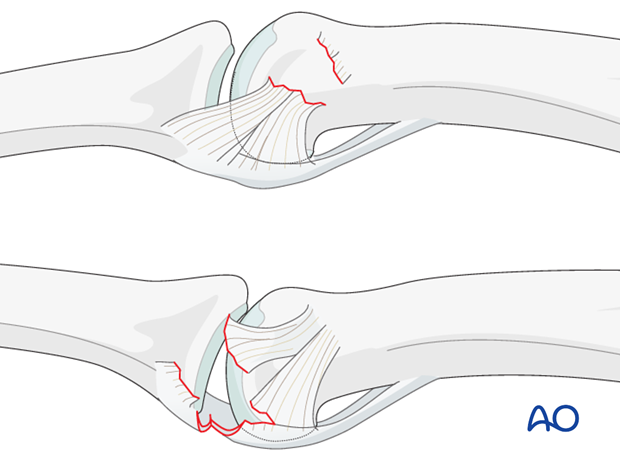
Ligament injuries
The collateral ligament usually tears at one of two locations:
a) at its attachment to the proximal phalanx
b) at its attachment to the volar plate and middle phalanx.
Often, these injuries are accompanied by a partial lesion of the volar plate.
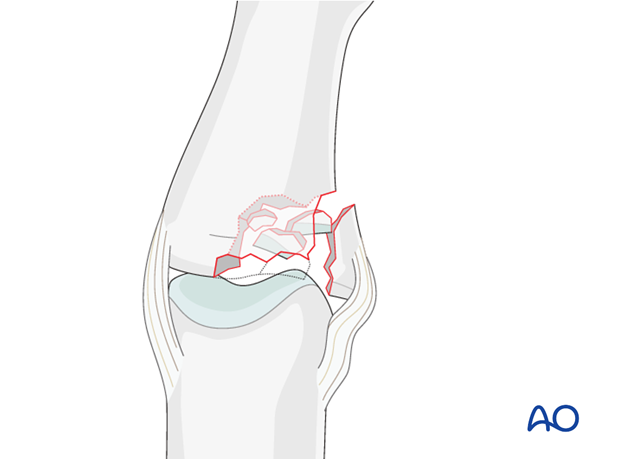
Accompanying fractures
Lateral subluxation can be accompanied by a condylar fracture, or a plateau fracture (either as an avulsion fracture, or as an impaction fracture).
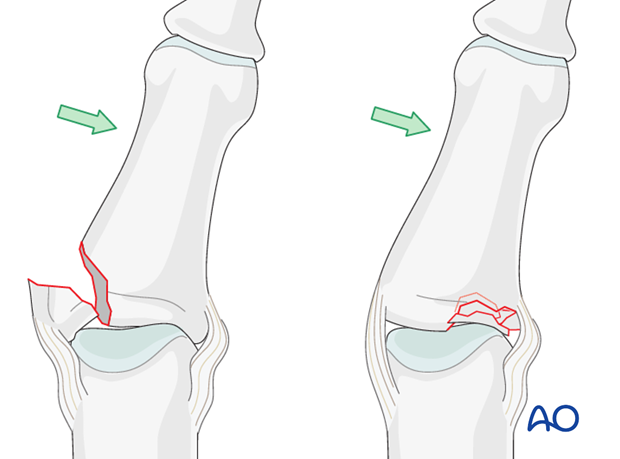
Mechanism of the injury – plateau compression fracture
A combination of lateral angulation and axial loading of the finger results in eccentric longitudinal compression forces on one condyle of the middle phalanx, leading to impaction fracture.
Often dorsal instability, or dorsal rotatory instability, is a result.
2. Approach
For this procedure a midaxial approach to the PIP joint is normally used.

3. Reduction
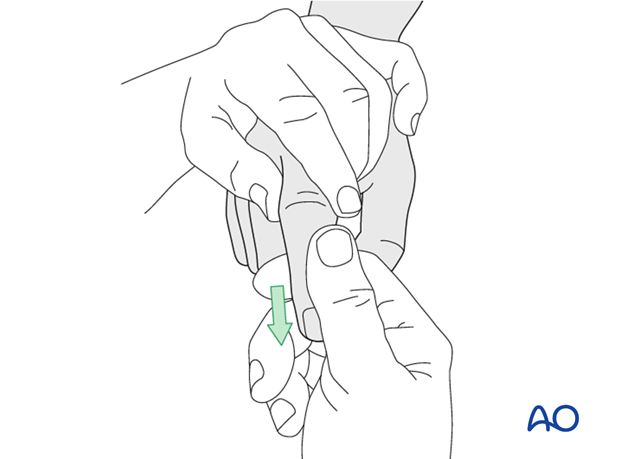
Closed reduction of dislocation
In cases of associated dislocation, start by reducing the dislocation.
Apply traction to the finger, with the PIP joint in slight flexion, to relax the flexor tendons and the lateral band.
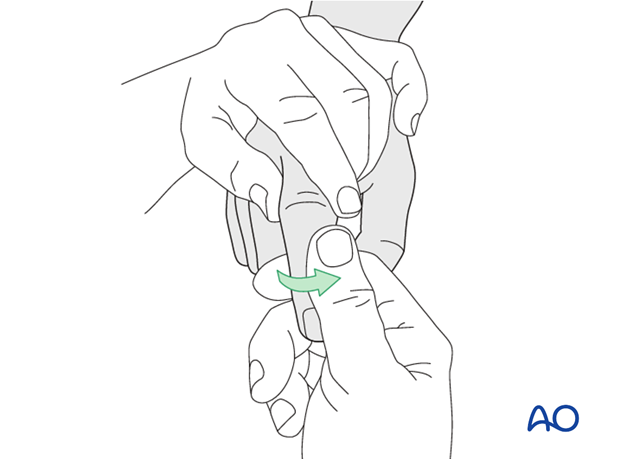
Then, maintaining the traction, deviate the finger laterally...
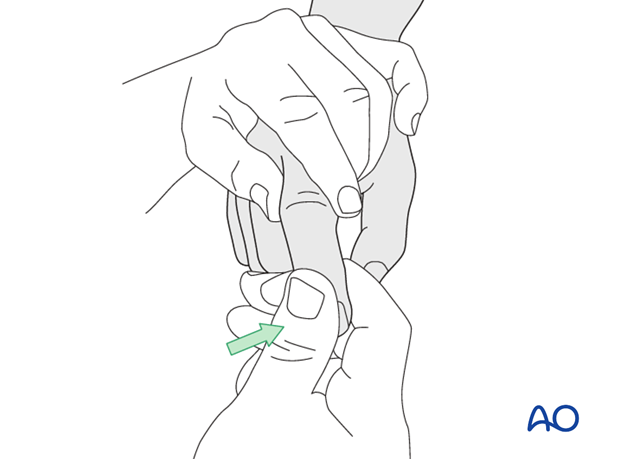
...and rotate towards the contralateral side.
In the majority of cases, the collateral ligament regains its natural anatomical position after reduction.
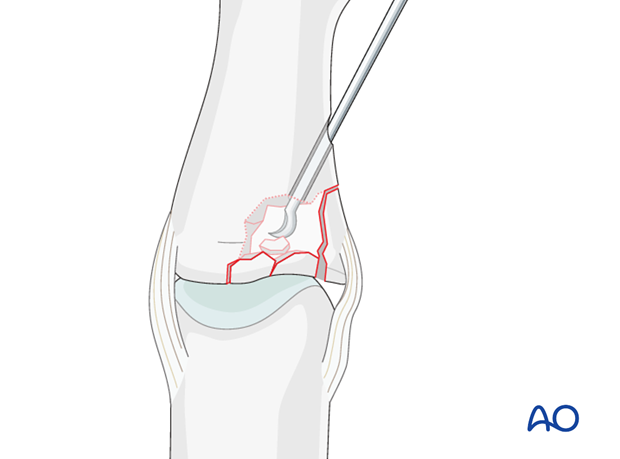
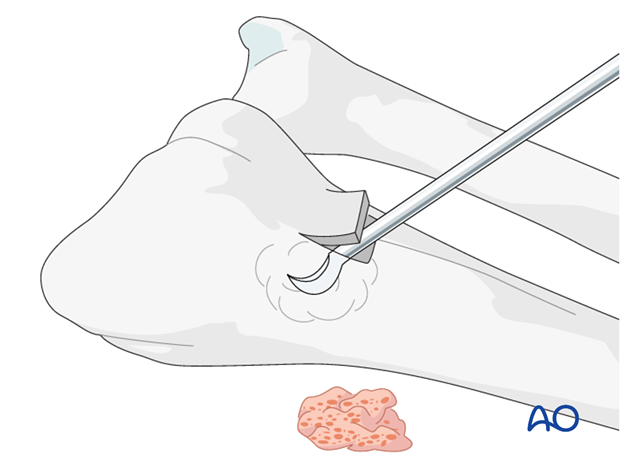
Create a metaphyseal entry portal
Use a 2.5 mm drill bit to create an entry portal just distal to the fracture zone, to permit disimpaction.
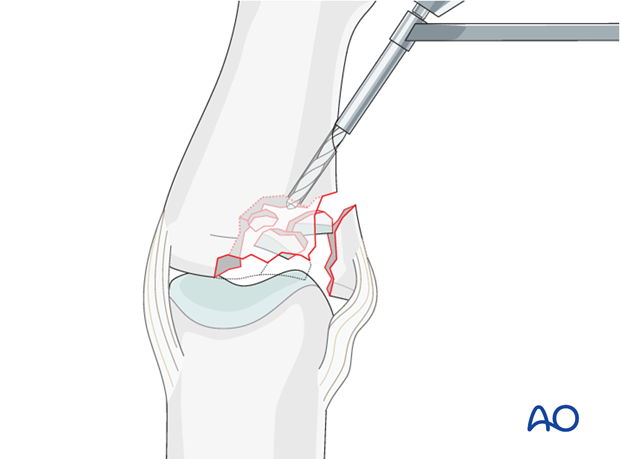
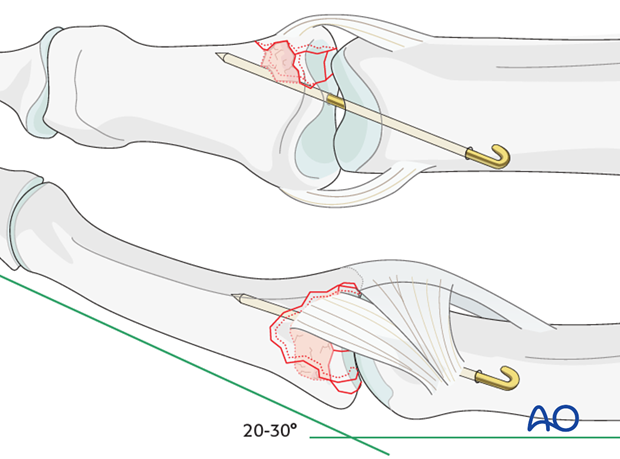
Disimpact the fragments
Insert a K-wire, a dental pick, or a tiny curette, into the drill hole. Disimpact the fragments and push them towards the head of the proximal phalanx, which can be used as a template to ensure congruity of the articular surface of the middle phalanx.
If a cartilage step-off greater than 1 mm remains, degenerative joint disease is likely to follow.
As the metaphyseal cancellous bone is disimpacted, a void may be created.
This jeopardizes the fracture in two ways:
- It is a very unstable situation in which the fragments may easily redisplace (collapse)
- the healing process is delayed.
4. Bone graft
Harvest site
Cancellous autograft will be necessary to support the articular fragments and fill the void. The graft will also assist the healing process.
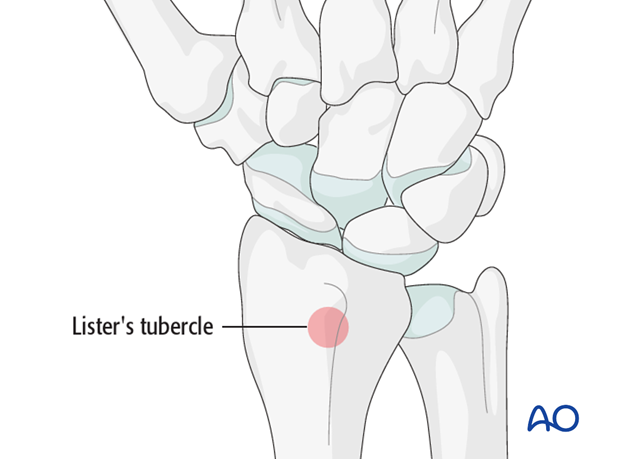
Harvest the bone graft from the distal radius. A suitable and safe place for the harvest is just proximal to Lister’s tubercle.
Harvesting
Make a 2 cm long incision proximal to the Lister’s tubercle. Retract the tendons of the second compartment radially, and the extensor pollicis longus (EPL) in an ulnar direction.
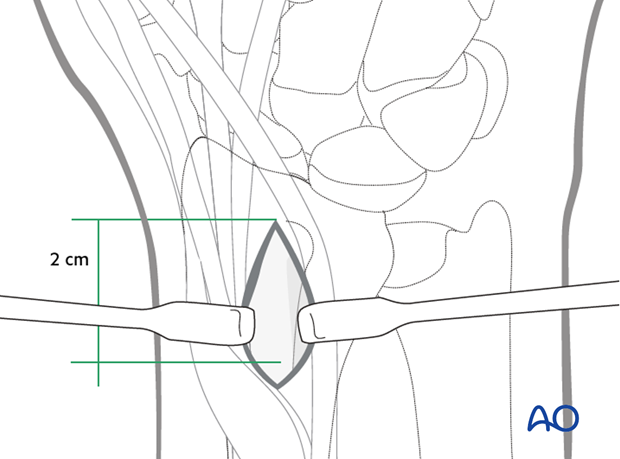
Use a chisel to cut three sides of a square. Hinge up the dorsal cortical flap. After harvesting cancellous bone, replace the “lid” and suture the periosteum and the skin incision.
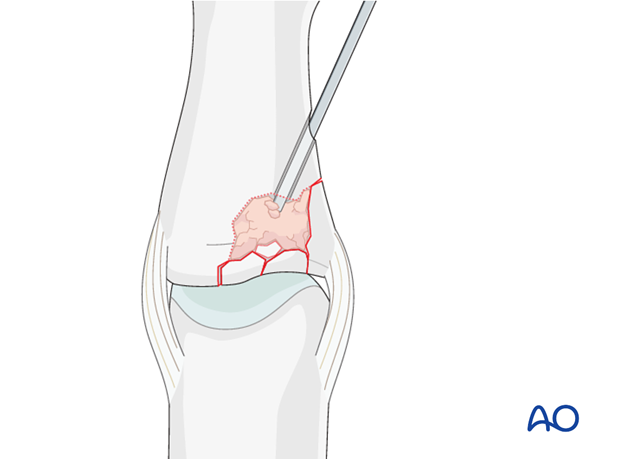
Insert graft into cavity
Fill the whole fracture cavity with compacted bone graft, using a blunt dissector.
The bone graft increases the potential for bone regeneration and healing, and mechanically supports the subchondral bone, helping to avoid its collapsing.
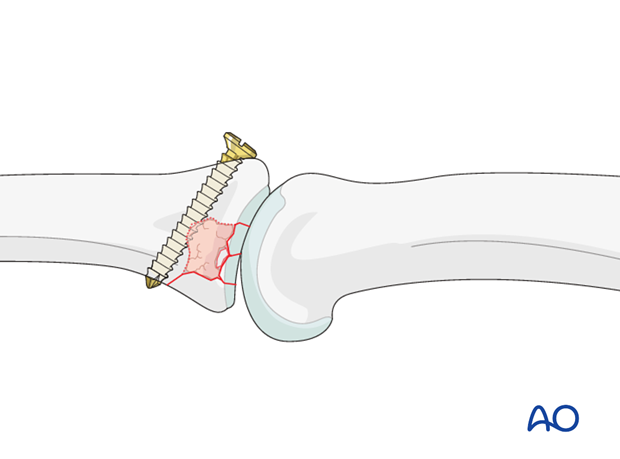
5. Fixation
Larger fragment
If a large fragment is present, maintain its reduction using a position screw.
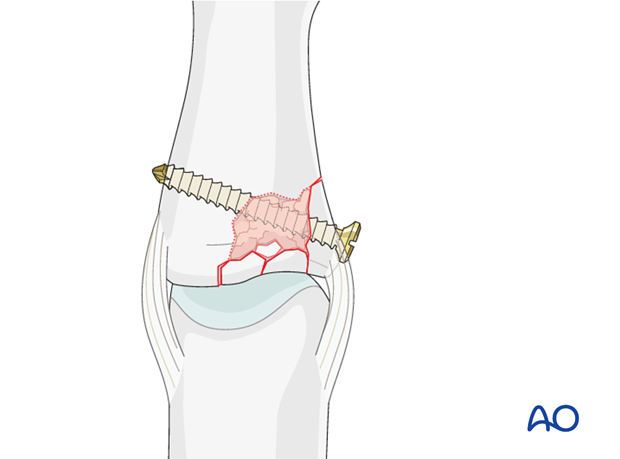
Small cavity
In case of a small cavity, one option is to insert a position screw from dorsal to palmar, just at the distal edge of the bone graft. This screw will serve to buttress the graft.
Alternative small cavity option
Another option for small cavities is to insert a K-wire to protect the reduction.
The K-wire crosses the PIP joint obliquely and holds it in 20-30 degrees of flexion.
6. Aftertreatment
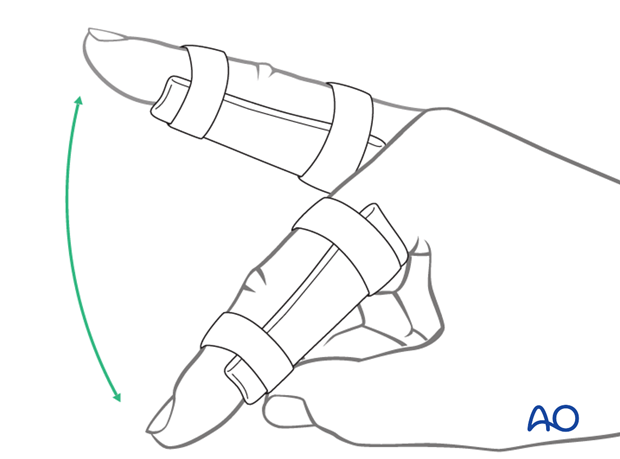
The PIP joint is immobilized in extension using a palmar splint, leaving the DIP joint free.
DIP joint ...

... and MP joint movement is encouraged immediately, in order to avoid extensor tendon adhesion and joint stiffness.
If no K-wire was used, leave the finger in the splint for 3 weeks.
K-wire removal
If a K-wire was inserted, retain it for 3 weeks, and then remove it.
Flexion and Extension
The removable palmar splint is worn for another 2 weeks after K-wire removal, and the patient is encouraged to take it off 4-5 times a day to do gentle flexion and extension exercises with buddy straps for protection.
Functional exercises
After the splint is removed, unrestricted active flexion and extension with buddy straps is permitted.
A night splint is recommended until the end of the 8th week.
Sporting activities
Sporting activities are allowed only after 3 months, and buddy strapping is recommend.












