Midaxial approach to the PIP joint
1. Indications for the lateral approach to the PIP joint
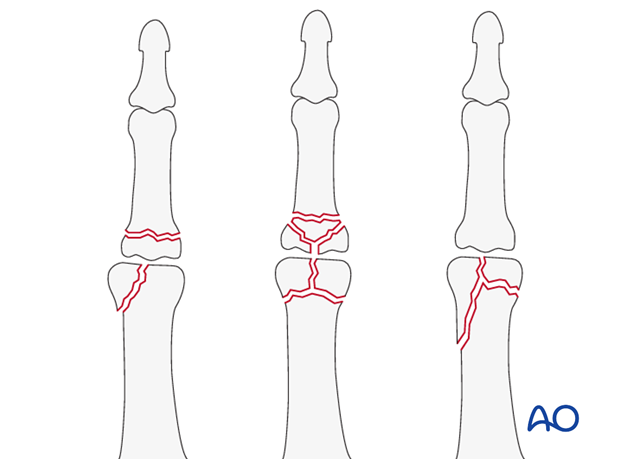
This approach is indicated for intra- or extraarticular basal, or condylar fractures. It is also used for irreducible dislocations with repair of the collateral ligament.
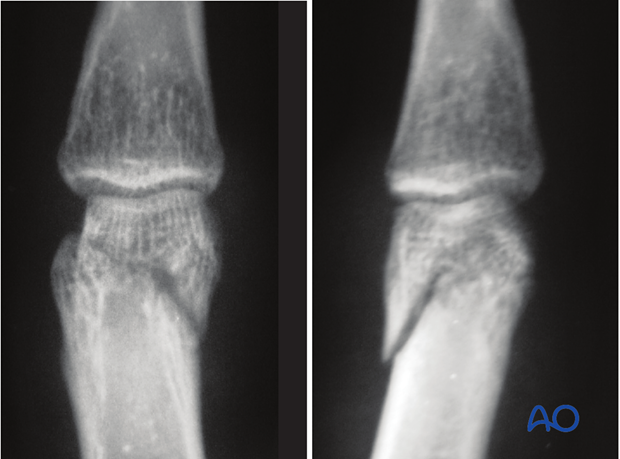
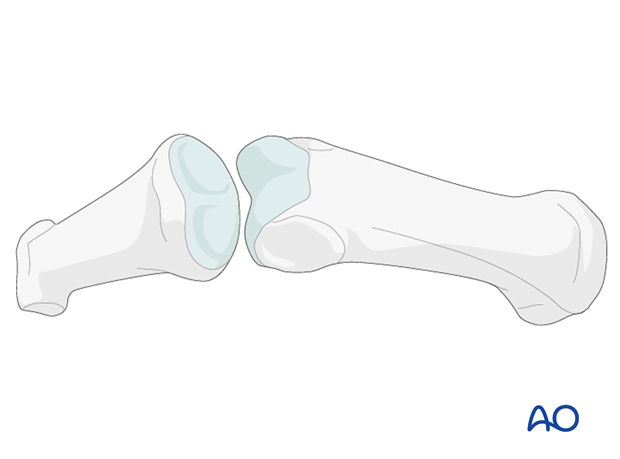
This x-ray shows a true unicondylar fracture, the ideal indication for this approach.

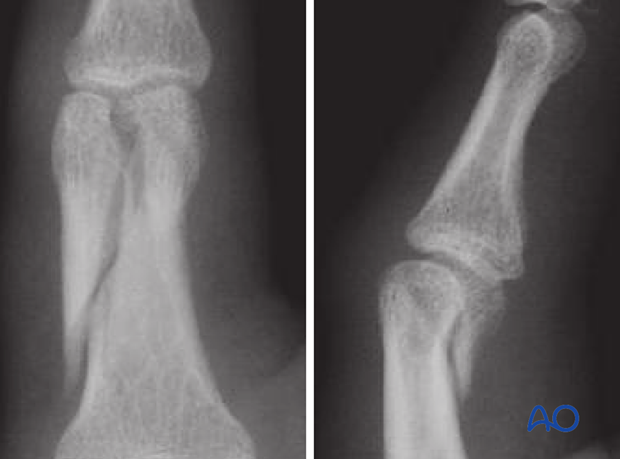
This approach is also used for juxtaarticular fractures.
It is occasionally used for bicondylar fractures with an extension into the diaphysis, but only if the contralateral condyle can be reduced and fixed.
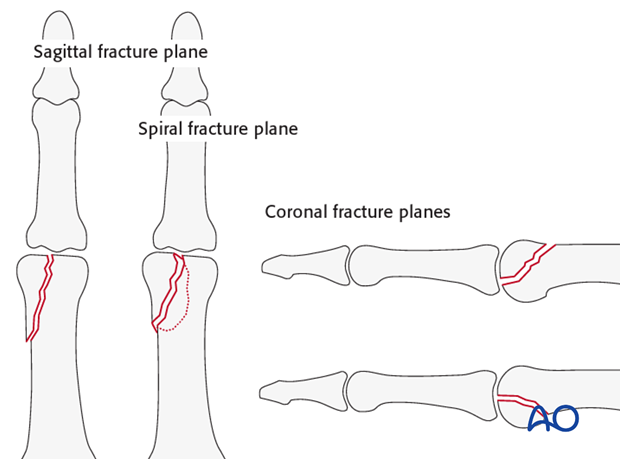
Intraarticular fractures in the interphalangeal joints may lie in the sagittal plane or the coronal plane. Complex, e.g. spiral, fractures may have multiple planes lying both sagittally and coronally.
Pitfall: Limited exposure
The lateral approach does not give access to the opposite condyle, which in some situations is necessary, notably in irreducible bicondylar fractures.
2. Surgical anatomy
The interphalangeal joints are hinge joints. The heads of the proximal and middle phalanges each have two articular condyles that resemble a grooved trochlea, and assist in preventing adduction/abduction and rotation, in conjunction with the collateral ligaments.
Dynamic stability results from compressive forces, which increase during pinch and grip. Passive stability derives from the bone morphology and tension in the collateral ligaments and the volar plate. This passive stability is maximal in full extension.
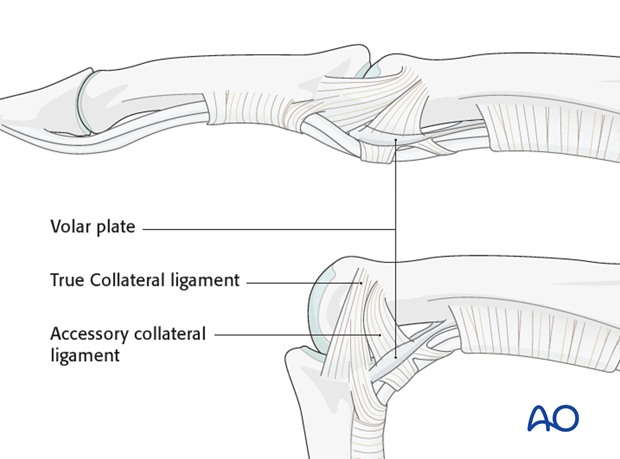
The primary structures stabilizing the interphalangeal joints and preventing displacement in the coronal plane (abduction/adduction) are the two collateral ligaments and the volar plate.
The collateral ligaments also prevent side-to-side translational displacement.
The accessory collateral ligaments slacken in flexion, while the true collateral ligament is further tensioned in flexion as a result of the greater palmar width of the condyles.
When using a lateral approach it is mandatory to avoid injury to these structures.
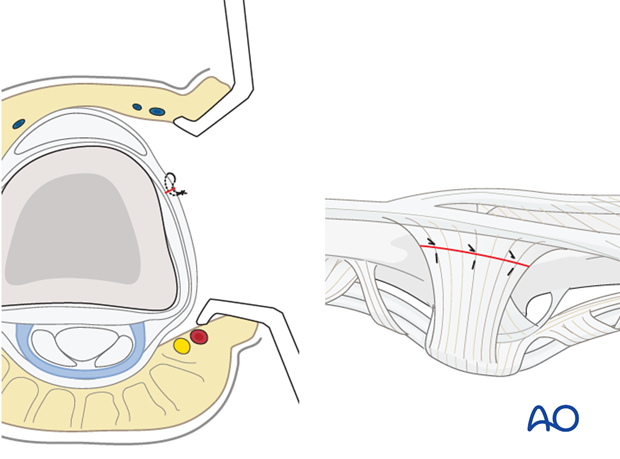
3. Planning the incision
To plan the line of the incision, fully flex the finger as shown and mark the dorsal ends of the flexor creases with dots.

Extend the finger and connect the dots in a line.
The resulting line is safe for a midaxial skin incision. The digital artery and digital nerve will lie palmar to this line.

4. Skin incision
Make a skin incision from the middle point between A and B to the middle point between B and C.
A limited approach using only this short part of the incision line may be used as an adjunct to percutaneous techniques of fixation.

5. Division of the transverse retinacular ligament (TRL)
In order to avoid accidentally cutting the collateral ligament, insert a dental pick between it and the TRL.
The TRL can now be divided safely by cutting onto the dental pick.
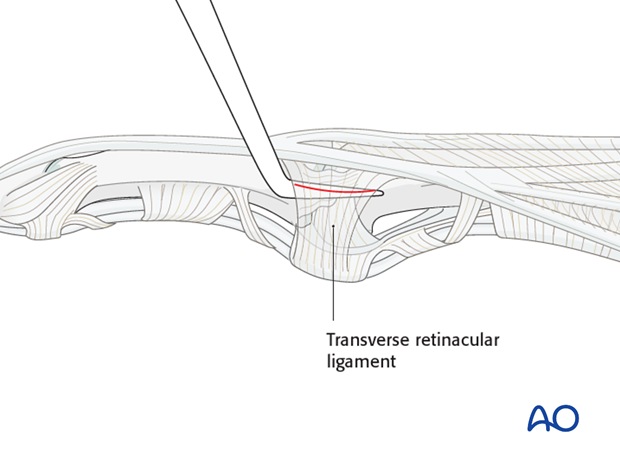
The dorsal fringe of the TRL is then retracted dorsally with the lateral band of the extensor tendon, to expose the collateral ligament. The palmar remainder of the TRL is retracted in a palmar direction, using two fine sutures.
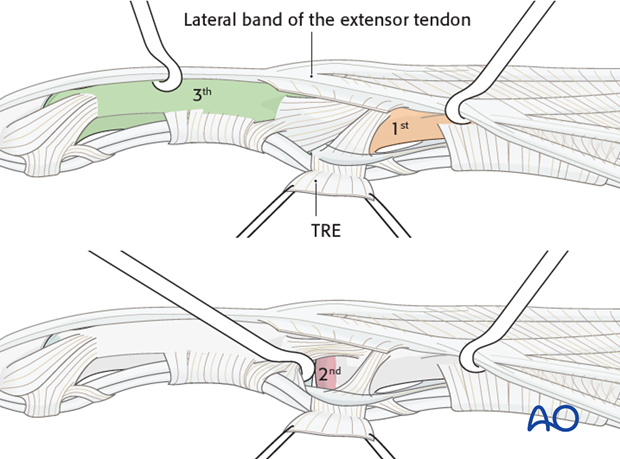
Three windows can therefore be developed:
First window
The first window is proximal to the collateral ligaments (shown in yellow), allowing exposure of the distal of the proximal phalangeal diaphysis.
Second window
Secondly, there is a small intermediate window between the true collateral and the accessory ligaments (shown in red).
This is likely to be necessary to approach and stabilize certain small articular fragments.
Third window
The third window (shown in green) is distal to the collateral ligaments, allowing exposure of the middle phalangeal shaft.
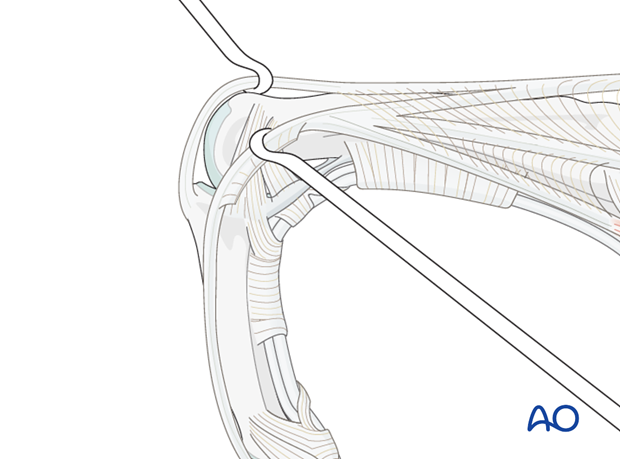
6. Alternative articular window
A further window can be created, firstly by flexing the PIP joint and developing the interval between the central and lateral slips of the extensor apparatus. A longitudinal capsulotomy can then be made to inspect the joint.
The central slip insertion should be preserved, otherwise a boutonnière deformity can result.
7. Wound closure
Repair the TRL with multiple fine mattress sutures before closing the skin.