Central slip reattachment
1. General considerations
Indication
Surgical management of a central slip rupture or avulsion is indicated if:
- the fracture does not reduce, usually as a result of soft-tissue interposition.
- the reduced joint is unstable.
Suture anchors or bone tunneling
Two alternative techniques are available for reattachment of the central slip: suture anchors or bone tunneling.
The advantage of suture anchors is the relative ease of the procedure. It is also a time-saving technique.
Tunneling is the more demanding procedure, but it is significantly less expensive.
Recovery process
The recovery process after such injuries is slow. Advise the patient to expect 6–8 months for full recovery.
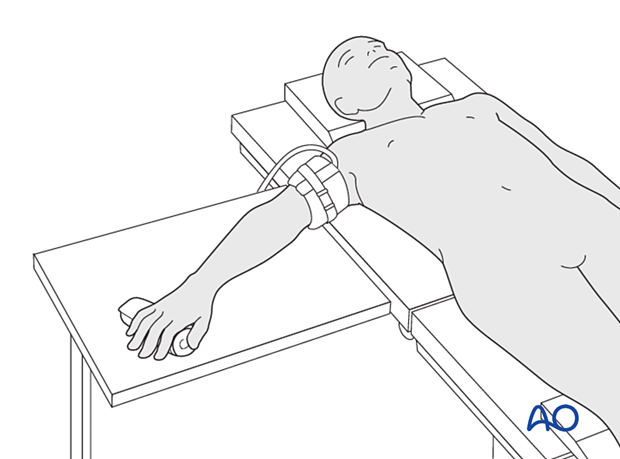
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.
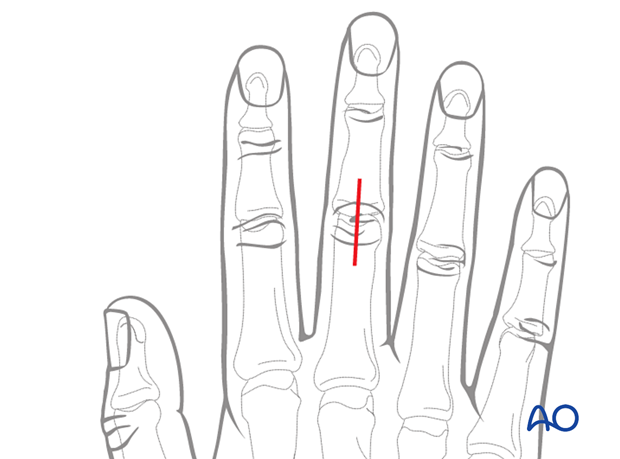
3. Approach
For this procedure a dorsal approach to the PIP joint is normally used.
4. Reduction of dislocation
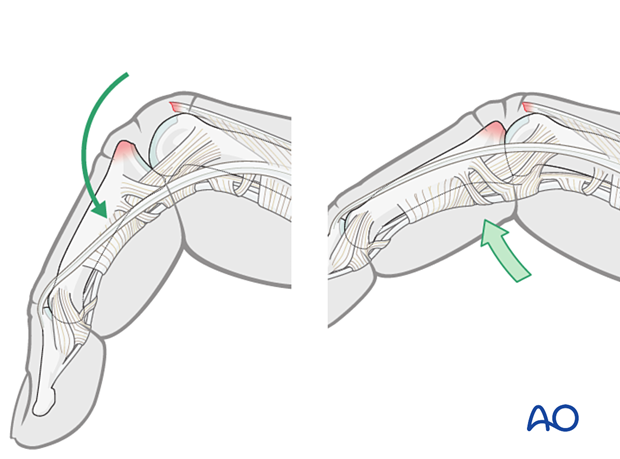
Dislocation usually occurs as a hyperflexion deformity.
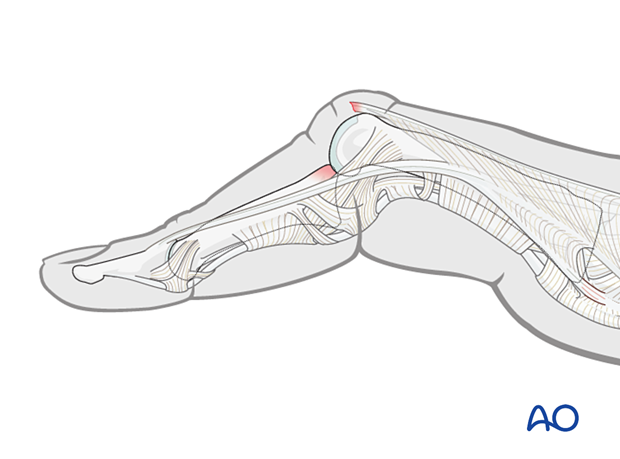
This can be reduced by increasing the deformity with some volarly applied pressure on the middle phalanx to reduce the joint. This keeps the collateral structures in tension and reduced the risk of soft-tissue interposition.
Stability evaluation
Confirm reduction with an image intensifier and check the joint stability by passive flexion and extension. This should show congruent movement compared with the adjacent joints.
If the central slip avulsion fragment is perfectly reduced and maintained throughout full range of motion, no further operative treatment is necessary but splintage is mandatory.
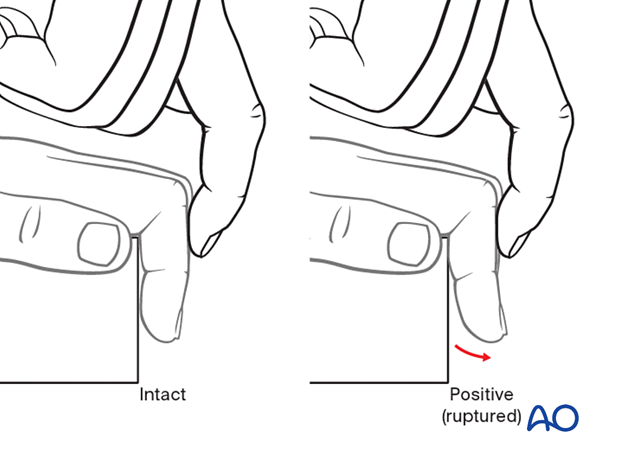
If there is no avulsion fragment visible in the x-ray, the central slip lesion should be assessed with the Elson test.
5. Visualizing the joint
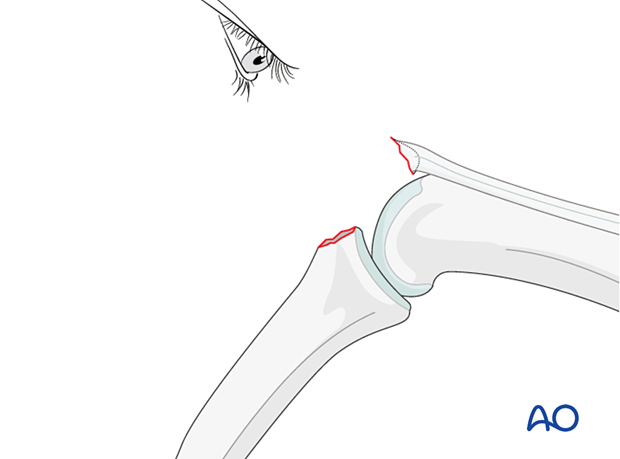
Flex the PIP joint to gain a better view of the fracture and the joint.
Often the presence of comminution is not apparent from the x-rays and can only be determined under direct vision.
Use a dental pick carefully to free interposed tissues, and to remove blood clot and other debris.
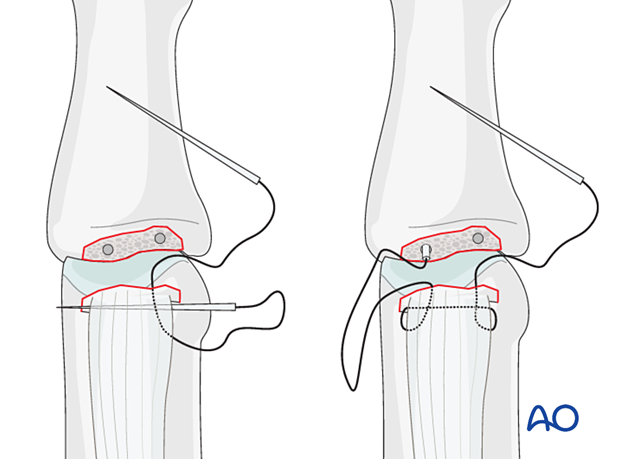
6. Option 1 – Suture anchor fixation
Drilling an anchor hole
Keep the PIP flexed to visualize maximally the area of the fracture at the base of the phalanx.
Use the appropriate drill to prepare a pilot hole for the anchor.
Insertion of the anchor
Insert an anchor with appropriate size according to the manufacturer’s instructions at the isometric point of insertion.
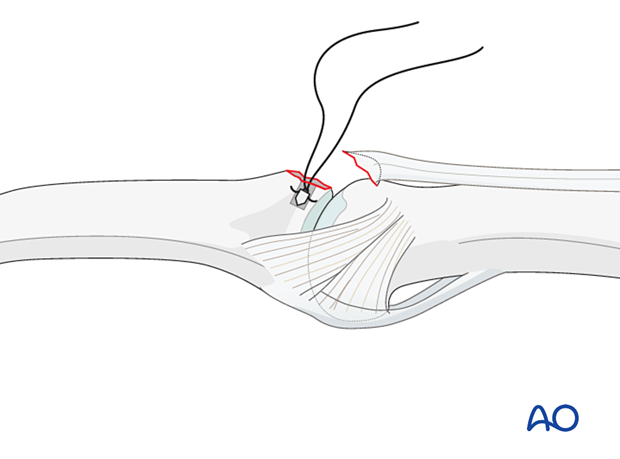
Insertion of sutures
Insert the sutures into the free end of the ligament.
Reapproximate the central slip to the phalanx and make a loop in each end of the thread as an anchoring pass. Tie a knot to secure the tendon to the phalanx.
Reattaching the central slip close to the subchondral bone will ensure a smooth surface for ideal mobility.
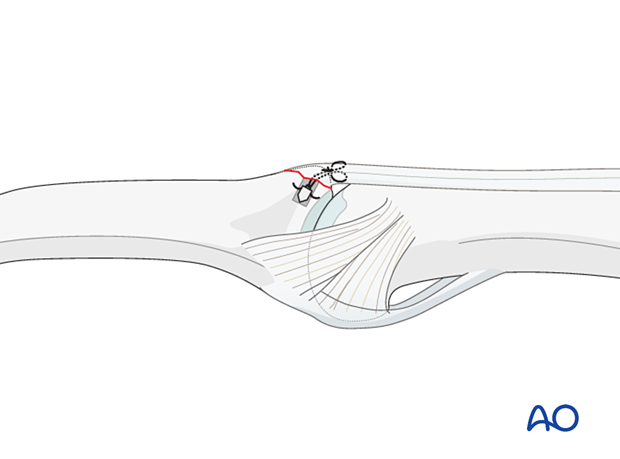
Alternative: fixation with two suture anchors
If the size of the fragment allows, two suture anchors can be used.
Choose anchors corresponding to the breadth of the fracture.
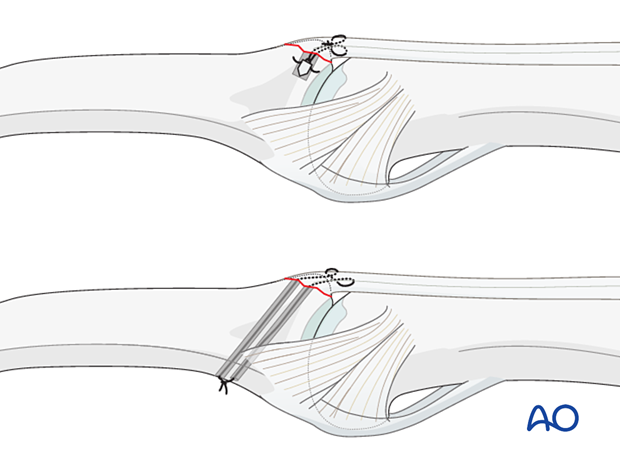
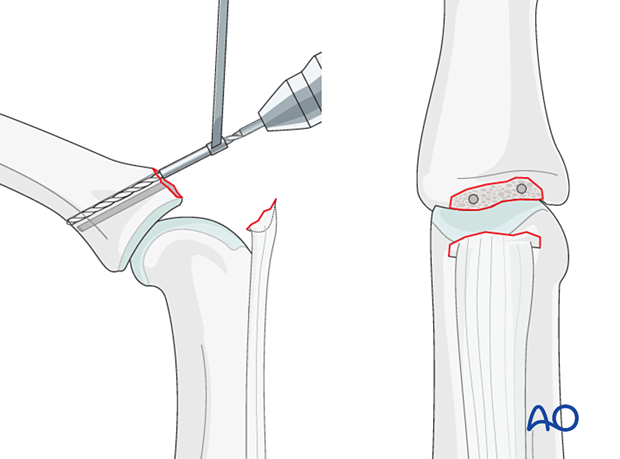
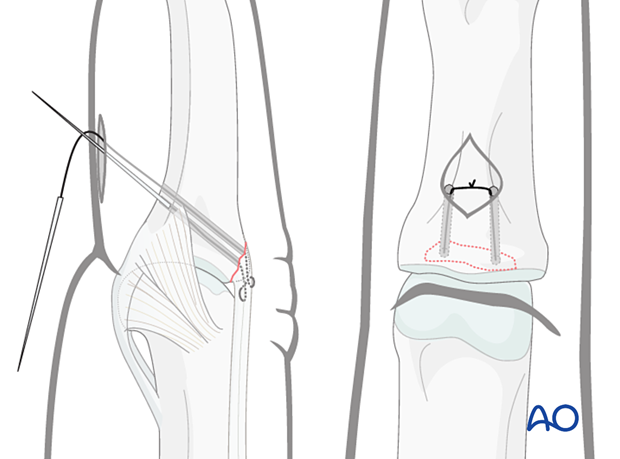
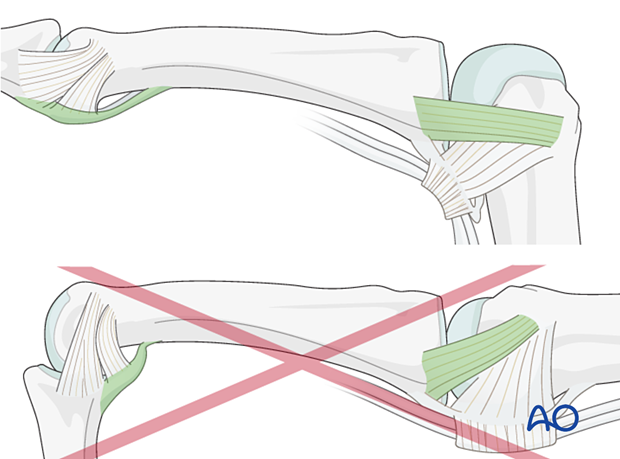
7. Option 2 – Bone tunneling
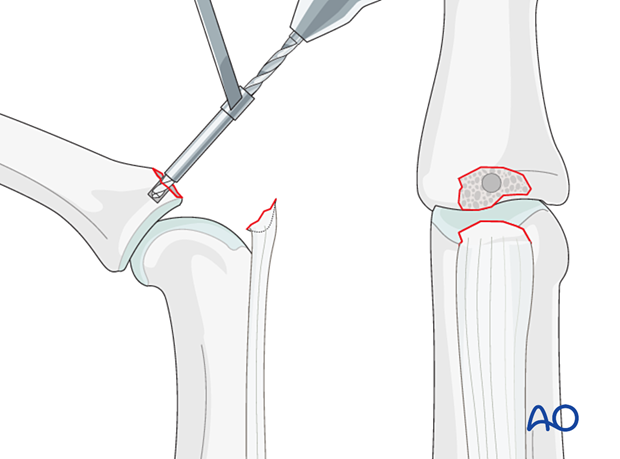
Drilling
Use a 1.0 mm drill or a K-wire to create two parallel drill holes, angled from proximal to distal and penetrating the opposite cortex. The entry point is close to the articular margin.
A drill sleeve for soft-tissue protection is mandatory.
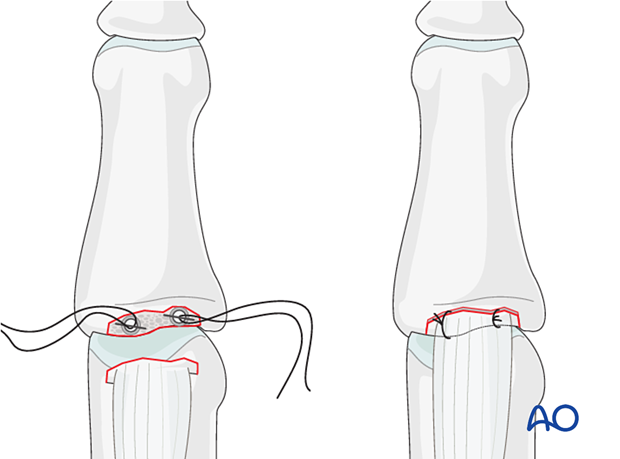
Insertion of sutures
4.0 nonresorbable, braided sutures, with straight needles, are used.
Insert the sutures obliquely through the end of the central slip, make a loop in each end of the thread as an anchoring pass, and thread each needle through a drill hole.
Reapproximating the central slip
Make a small incision in the opposite side of the finger to retrieve the sutures. Cut off the needles, pull the sutures to approximate the central slip, and tie a knot over the cortical bone.
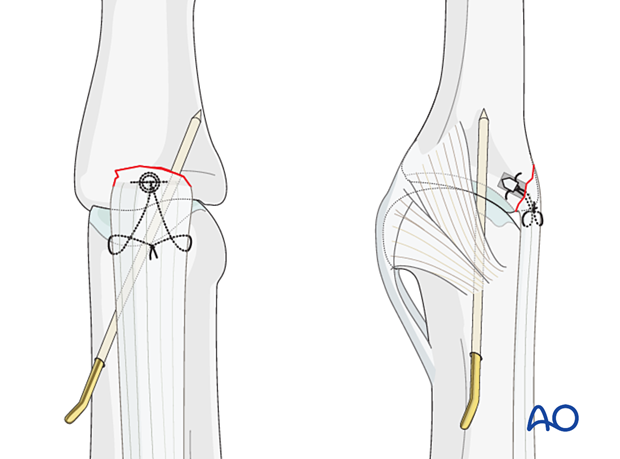
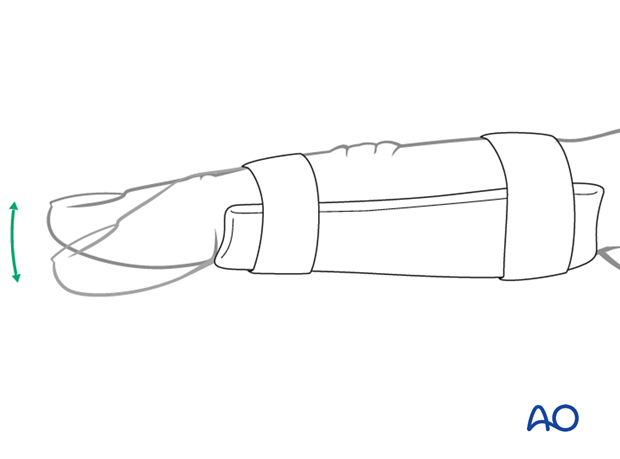
8. Joint transfixation with K-wire
Transfixation of the joint for 4–6 weeks is recommended to protect the central slip reattachment. There is an increased risk of joint stiffness.
Pass a 1.2 mm K-wire obliquely across the PIP joint with the joint in extension. This position protects the ligament reattachment.
Leave the end of the K-wire outside of the skin to facilitate later removal.
The fixation must be protected with a splint to reduce the risk of wire breakage.
9. Final assessment
Check joint congruity using image intensification. Reduction must be anatomical.
10. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
If there is swelling, the hand is supported with a dorsal splint for a week. This should allow for movement of the unaffected fingers and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
The hand should be immobilized in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- MCP joint in 90° flexion
- PIP joint in extension
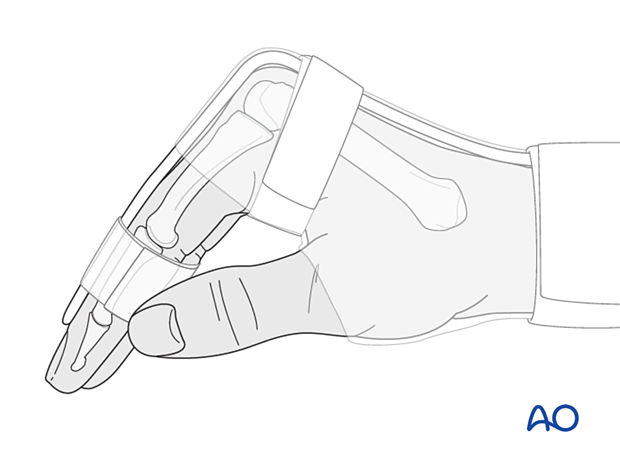
The MCP joint is splinted in flexion to maintain its collateral ligaments at maximal length to avoid contractures.
The PIP joint is splinted in extension to maintain the length of the volar plate.
After swelling has subsided, the PIP joint is protected in extension with a palmar splint, leaving the DIP joint free.
Cleaning
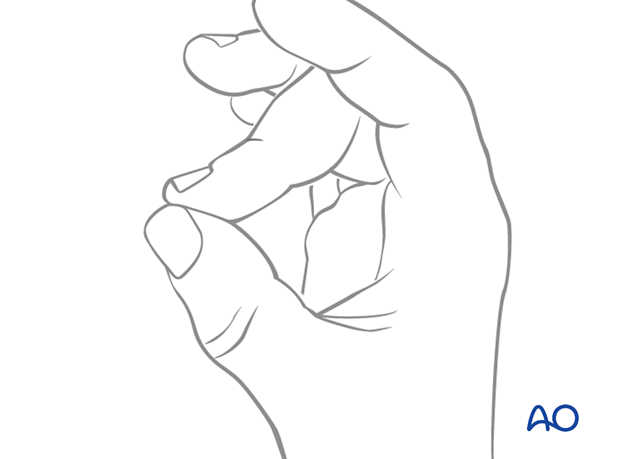
Removal of the splint and skincare must be performed by the patient at weekly intervals.
Instruct the patient to keep the finger in extension by pinching it with the thumb when the splint is taken off for cleaning or by pressing the tip of the finger onto a tabletop.
Any flexing of the finger may disrupt the healing process.
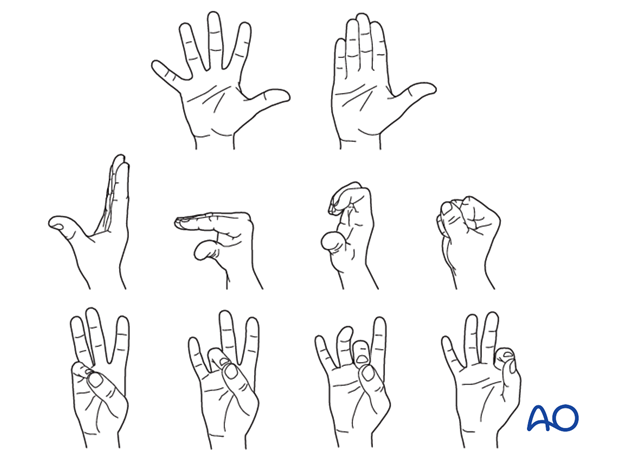
Mobilization
To prevent joint stiffness, the patient should be instructed to begin active motion (flexion and extension) of all nonimmobilized joints immediately after surgery.
After K-wire and splint removal, unrestricted active flexion and extension is permitted.
Follow-up
X-ray checks of joint position must be performed immediately after the splint has been applied.
Follow-up x-rays with the splint should be taken after 1 week and, if necessary, after 2 weeks. A final x-ray can be taken at the expected fracture consolidation.
In the middle phalanx, the fracture line can be visible in the x-ray for up to 6 months. Clinical evaluation (level of pain) is the most important indicator of fracture healing and consolidation.
K-wire removal
The K-wire is removed after 4–6 weeks.













