Collateral ligament repair
1. Principles
Dislocations
While dislocations and ligament injuries are common in the hand, they are most common at the PIP joint.
The spectrum of these lesions ranges from minor stretching (sprains) to complete disruptions of the ligaments.
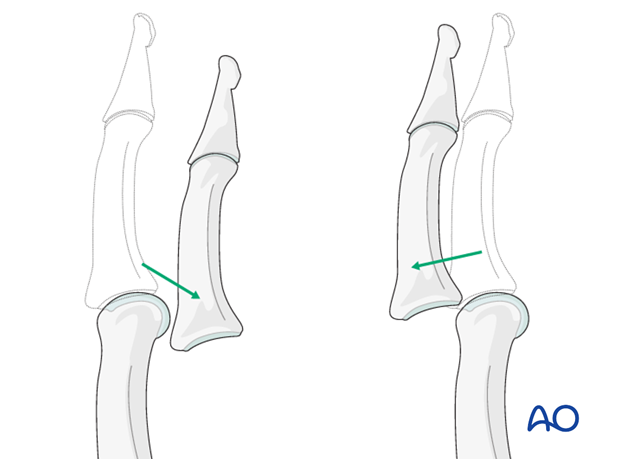
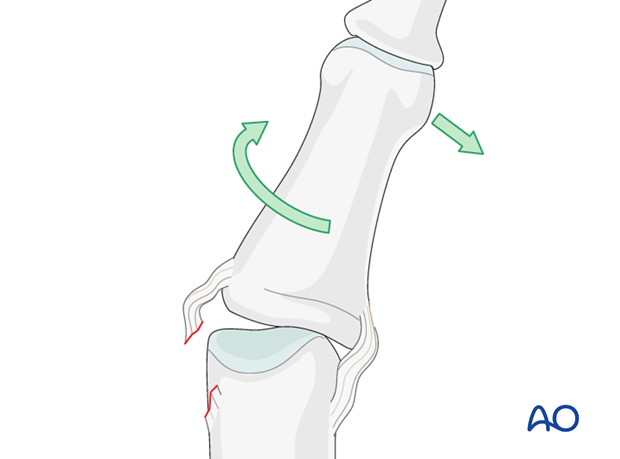
Dislocations of the PIP joint are classified by the direction of displacement of the middle phalanx. They can be palmar, dorsal, lateral, or lateral rotatory.
Ligament injuries
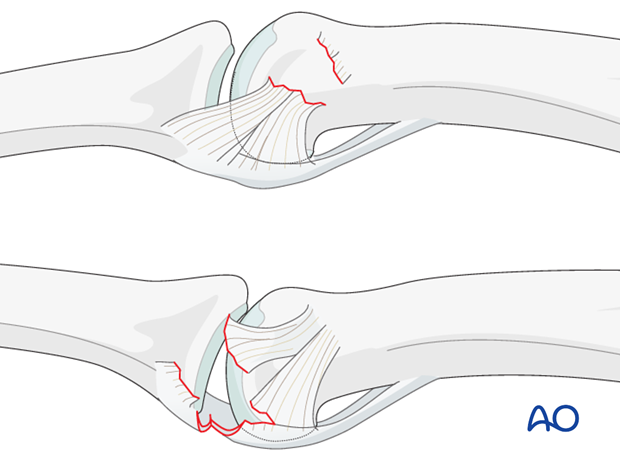
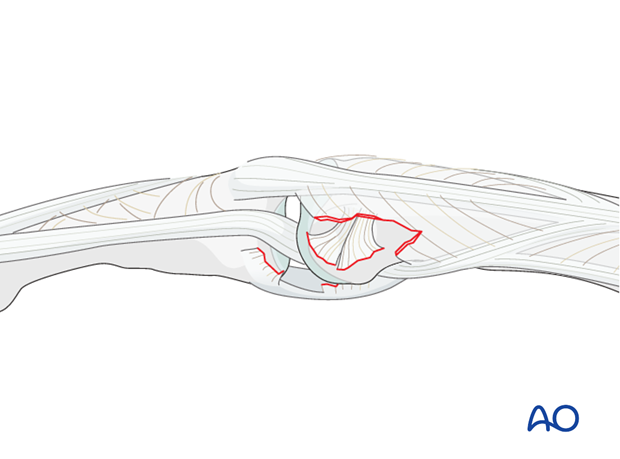
The collateral ligament usually tears at one of two locations:
a) at its attachment to the proximal phalanx
b) at its attachment to the volar plate and middle phalanx.
Often, these injuries are accompanied by a partial lesion of the volar plate.
Accompanying fractures
Lateral subluxation can be accompanied by a condylar fracture, or a plateau fracture (either as an avulsion fracture, or as an impaction fracture).
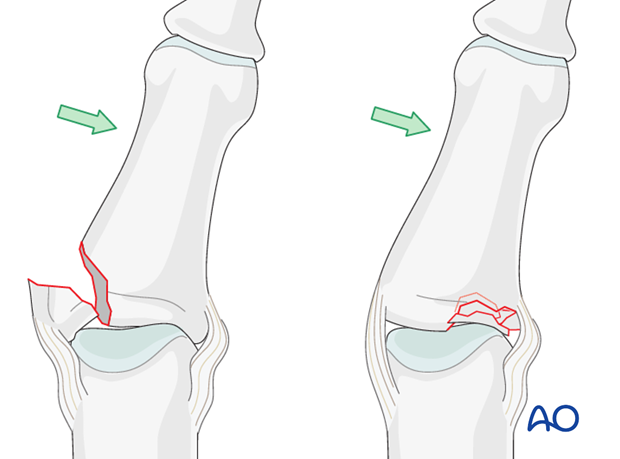
Lateral dislocation accompanied by plateau fracture
Mechanism of the injury
Typically, these injuries occur after lateral deviation and rotation, with the PIP joint in semi-flexion. This often happens during sporting activities, or while getting a finger caught in rotatory machines such as drills, etc.
Diagnosis
A diagnosis is made on the basis of the history and mechanism of the trauma, clinical examination, and by x-rays in 2 planes.
Check the vascularity and the digital nerve function. Very rarely, these injuries may have an open wound.
A typical sign of collateral ligament injuries is abnormal lateral mobility of the PIP joint even after reduction of the dislocation, while the patient can flex and extend the finger.
2. Indications
Ligament repair has been criticized because of the additional soft-tissue trauma inflicted.
The problem in these injuries is usually not instability, but the risk of joint stiffening.
Many publications have shown that, in skilled hands, ligament repair provides a more predictable outcome. It is especially indicated in high-demand patients, and in those requiring early function and return to normal activities.
Absolute indications for surgical treatment are:
- irreducibility due to interposed soft tissues
- gross instability after reduction (redislocation when patient flexes and extends the finger)
- subacute collateral ligament rupture with persistent PIP instability
- radial collateral ligament ruptures of the index finger.
Treatment principles
When ligament repair is necessary, the surgeon should be aware of 3 guiding principles:
- know precisely where the lesion is
- be familiar with the approach and the local anatomy
- minimize any soft-tissue dissection.
It is wise to use magnifying loupes throughout the procedure.
3. Approach
For this procedure a midaxial approach to the PIP joint is normally used.

4. Closed reduction
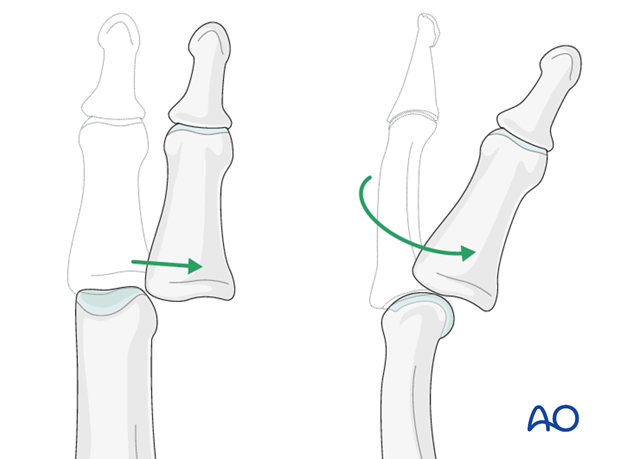
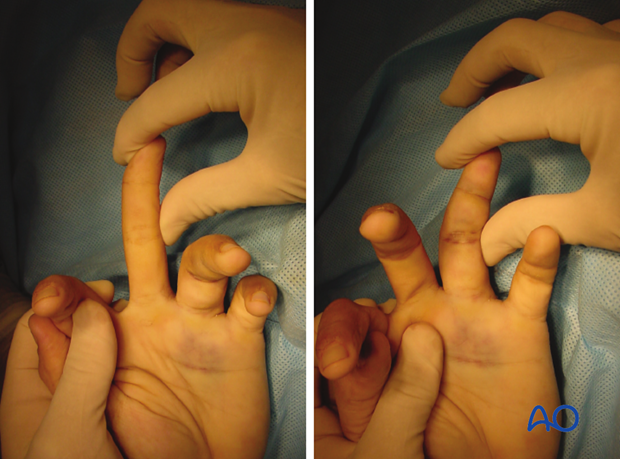
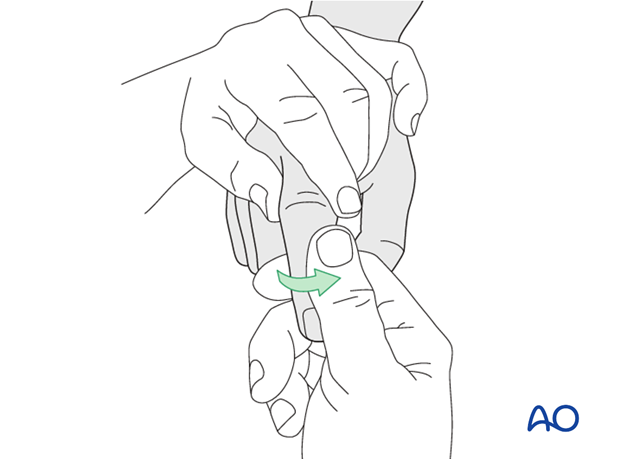
Apply traction to the finger, with the PIP joint in slight flexion to relax the flexor tendons and the lateral band.
Then, maintaining the traction, laterally deviate the finger...
...and rotate it towards the contralateral side.
In the majority of cases, the collateral ligament regains its natural anatomical position after reduction.
Check reduction with x-rays in two planes. The x-rays should show complete joint congruency.
If this is the case, no further operative treatment is necessary.
If any widening of the joint is visible, soft-tissue interposition, mostly of the lateral band, may be the cause.
In such cases, the condyle is trapped between the lateral band and the central slip (“buttonhole”).
This is an indication for open reduction and ligament repair.
5. Reduction and repair of interposed tissues
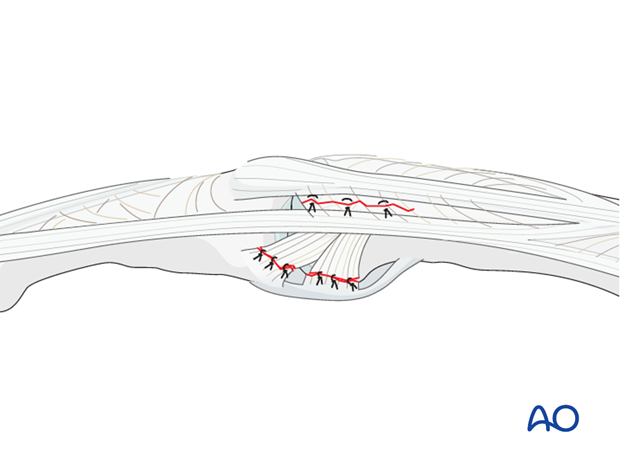
If the lateral band, or, more rarely, the central slip, or the collateral ligament, is trapped in the joint, use a dental pick to free and reduce it, while keeping the PIP joint in flexion.
In such cases, some repair is often necessary.
Use 6.0 nonabsorbable monofilament nylon sutures to repair the injury with interrupted stitches.
6. Collateral ligament detachment from proximal phalanx
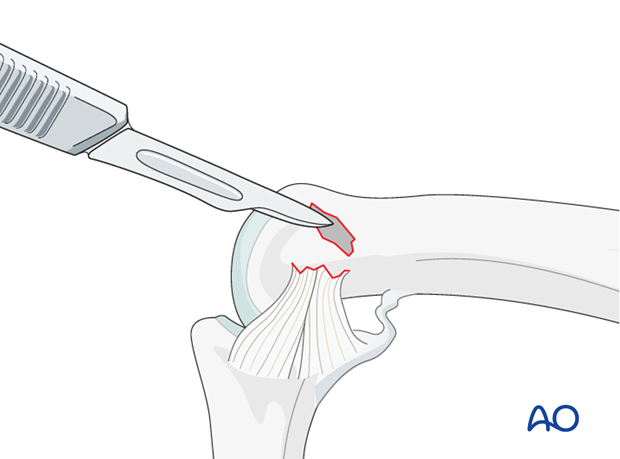
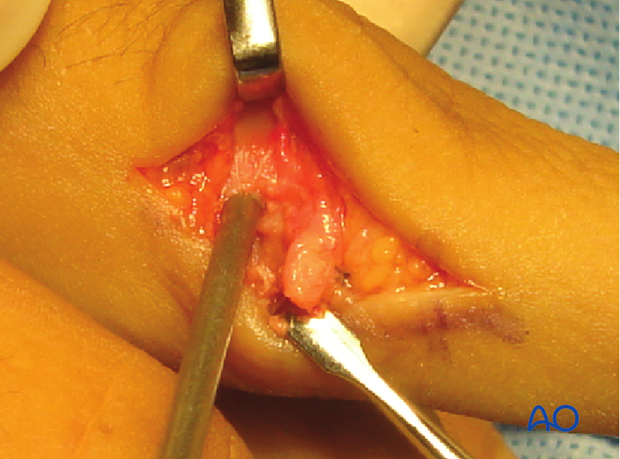
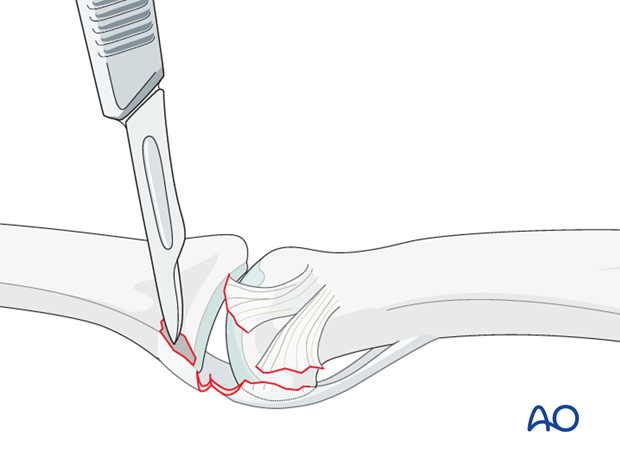
Prepare the attachment site
Using a scalpel, a tiny curette, or a small burr, clean the attachment site of the collateral ligament of any remaining soft tissues.
Prepare the reattachment site by exposing the cancellous bone. This improves the vascularity of the site and aids later healing.
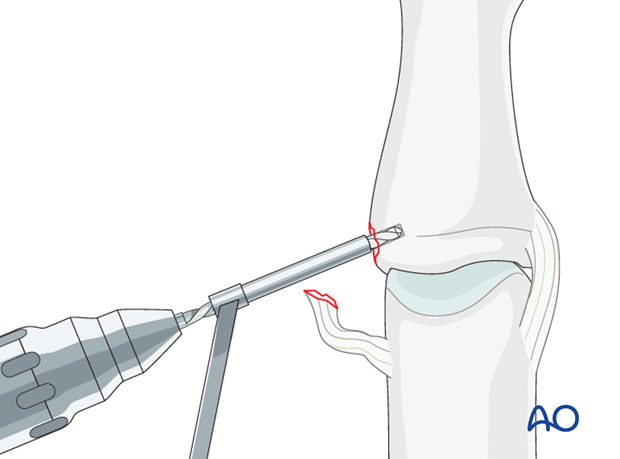
Drill anchor hole
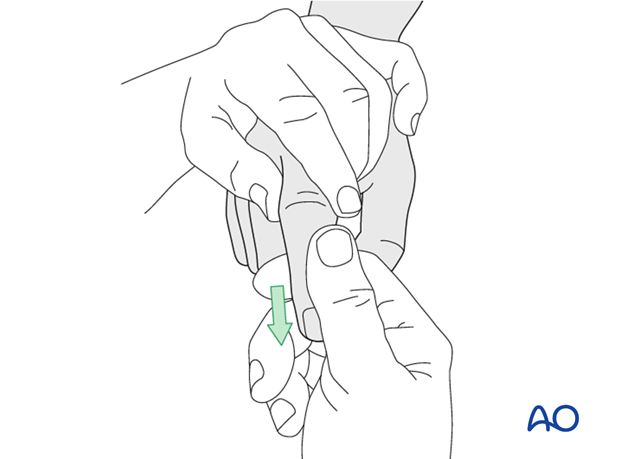
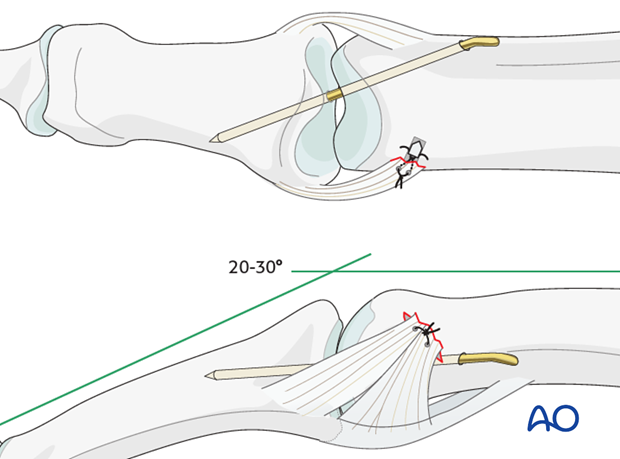
Keeping the finger flexed for better exposure, ...
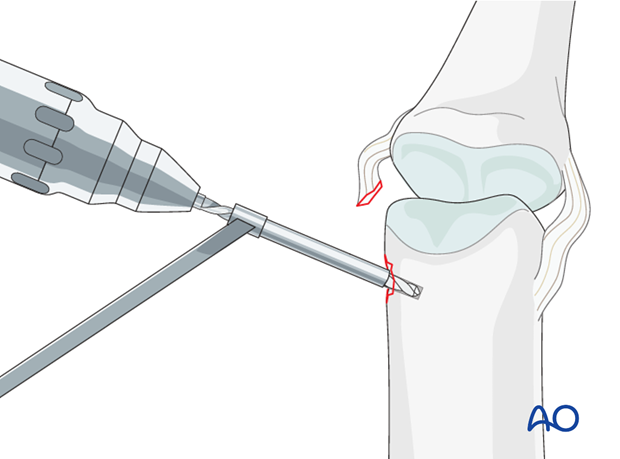
...use the appropriate drill bit to drill an anchor hole (1.3 mm).
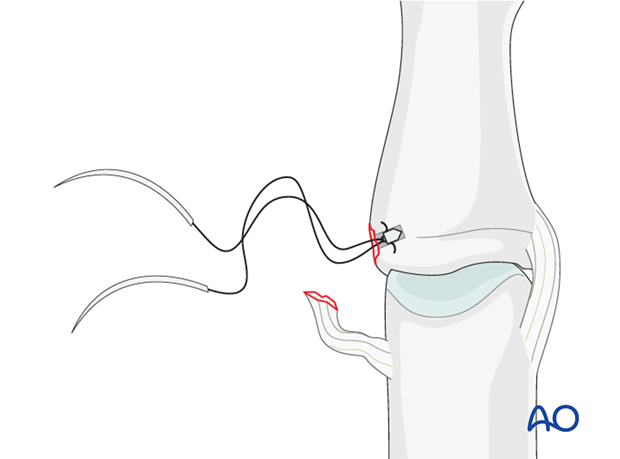
Insert anchor
Insert a 1.3 mm anchor into the drill hole.
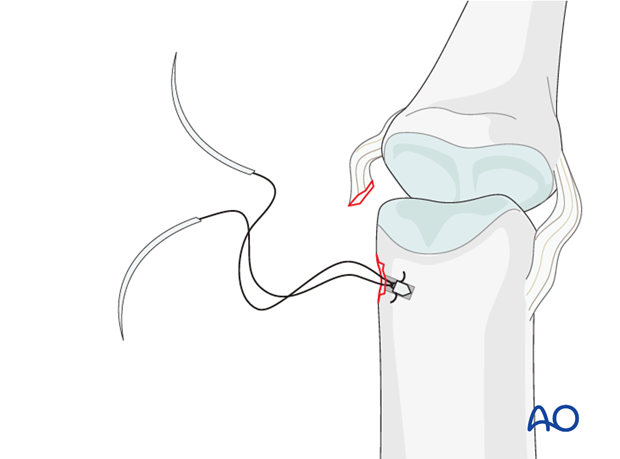
Insert sutures
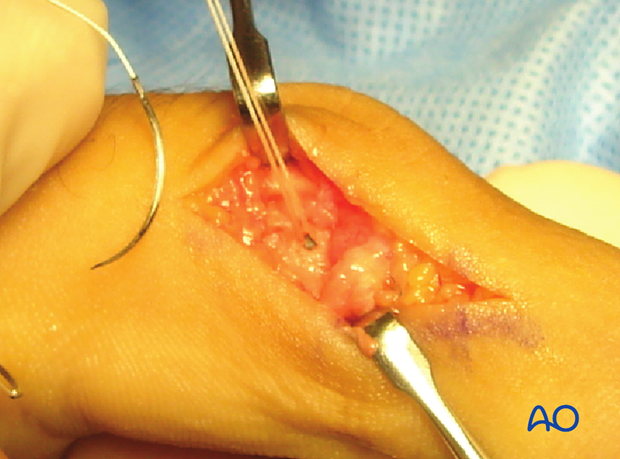
Approximate the collateral ligament to the reattachment site by extending the finger.
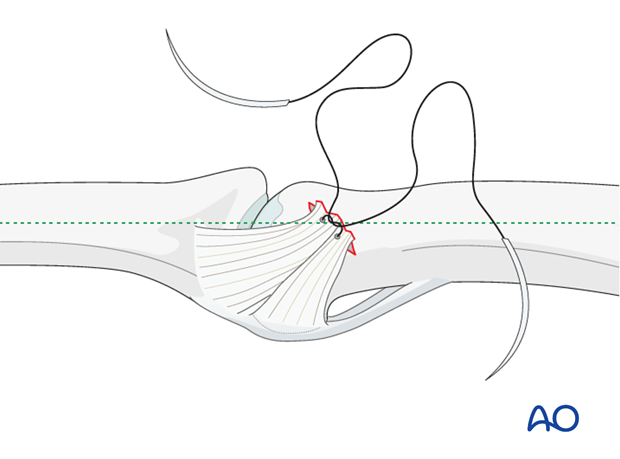
Insert the sutures through the ligament and tighten them.

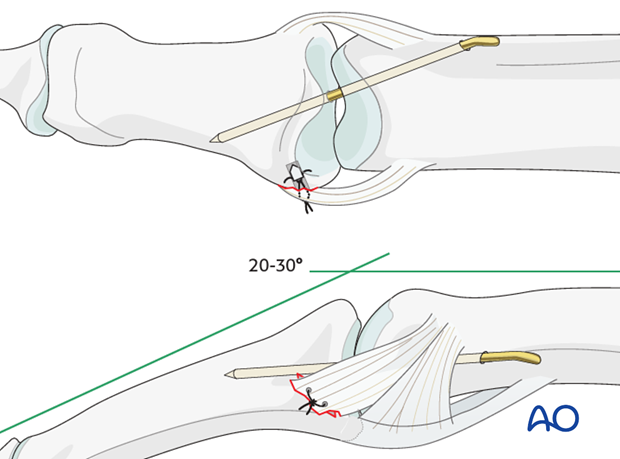
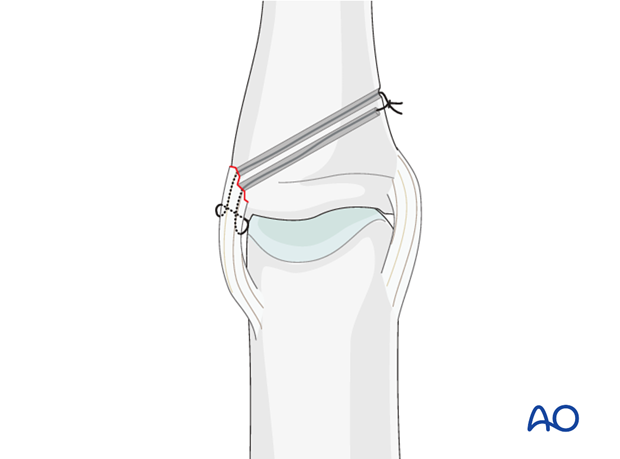
K-wire fixation
Insert a K-wire across the PIP joint obliquely, with the finger in 20-30 degrees of flexion.
7. Palmar detachment of collateral ligament
Description of the injury
In this kind of injury, the collateral ligament is fully detached from the middle phalanx. It is also fully detached from the volar plate. In most such cases, the volar plate is partly detached from the middle phalanx and has to be reattached.
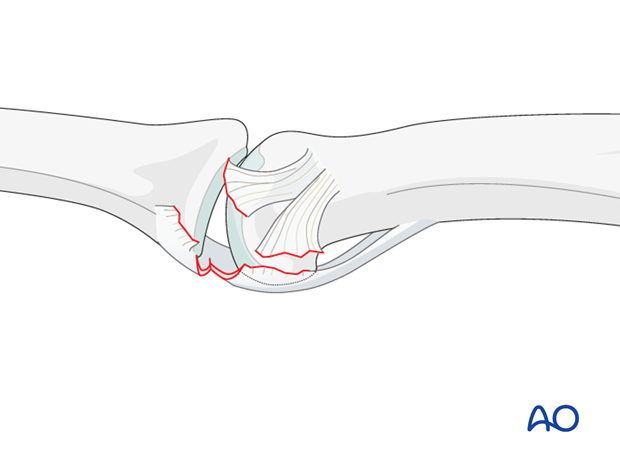
Prepare the attachment site
Using a scalpel, a tiny curette, or a small burr, clean the attachment site on the middle phalanx of any remaining soft tissues.
Prepare the reattachment site by exposing the cancellous bone to improve vascularity and subsequent bone healing.
Drill anchor hole
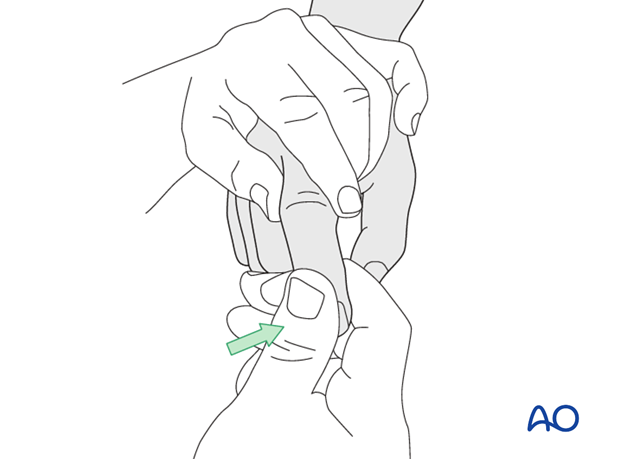
Extend the finger for better vision, and use the drill bit corresponding to the anchor (1.3 mm) to drill an anchor hole.
Insert anchor
Insert a 1.3 mm anchor into the drill hole.
Insert sutures
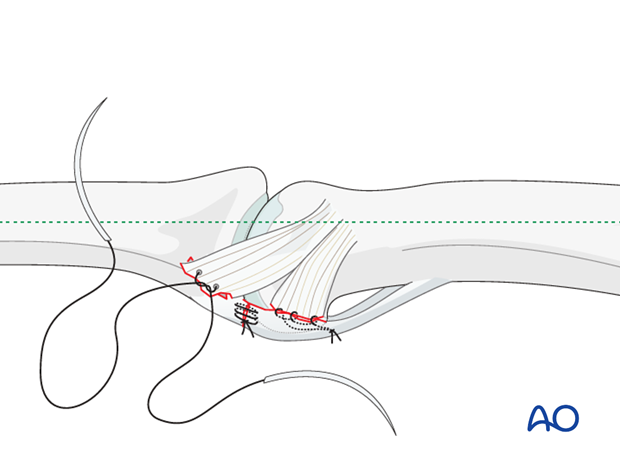
Approximate the collateral ligament and the volar plate to the reattachment site.
Insert the sutures through the ligament and the volar plate with one stitch, and tighten them.
K-wire fixation
Insert a K-wire across the PIP joint obliquely, with the finger in 20-30 degrees of flexion.
8. Alternative anchorage
If suture anchors are not available, an alternative method is to thread the sutures through two fine oblique drill holes in the base of the middle phalanx.
Make a small dorsal incision, and tie the sutures across the far cortex.
9. Aftertreatment
The PIP joint is immobilized in extension in a palmar splint, leaving the DIP joint free.
DIP joint ...

... and MCP joint movement is encouraged immediately to avoid extensor tendon adhesion and joint stiffness.
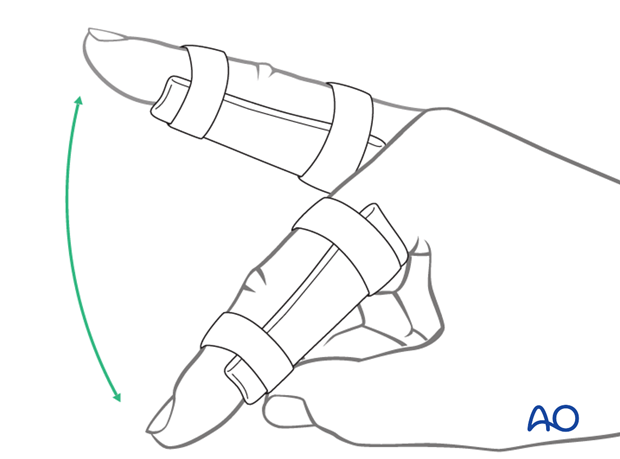
K-wire removal
Keep the K-wire in place for 3 weeks, and then remove it.
Flexion and Extension
The removable palmar splint is left on for another 2 weeks after K-wire removal, and the patient is encouraged to take it off 4-5 times a day to practise gentle flexion and extension exercises, with buddy strapping for protection of the ligament.
Functional exercises
After 5 weeks, the splint is removed, and unrestricted active flexion and extension is permitted.
A night splint is recommended until the end of the 8th week.
Sporting activities
Sporting activities are allowed only after 3 months, and buddy strapping is recommend.












