Intramedullary nailing
1. Principles
Indications
Intramedullary nailing of fractures of the shafts of the adult radius and/or ulna is rarely indicated and the role of intramedullary nailing is still to be defined. Rotational stability has long been a factor against the use of nails in adult forearm shaft fractures, although several locking options currently are proposed and may lead to a wider use in adult forearm fractures in the future.
The radius and ulna, in concert with the proximal and distal radio-ulnar joints, constitute a complex articulation, which permits supination and pronation of the forearm. As with all articular injuries, restoration of the exact skeletal morphology is essential as a platform for full functional recovery.
In the skeletally immature, there is some residual capacity for remodeling, especially in the very young, and approximate morphological restoration can be acceptable, in certain circumstances. For this reason, flexible intramedullary nailing of pediatric forearm shaft fractures is widely accepted.
In the adult, intramedullary nailing of forearm shaft fractures is only acceptable when the injury is such that anatomical reduction and plate osteosynthesis are strongly contraindicated. Such circumstances include crushing injury of the forearm with major soft-tissue mutilation (as in the illustrated case), the presence of extensive burns, and multiple skeletal injuries presenting a major pathophysiological challenge.
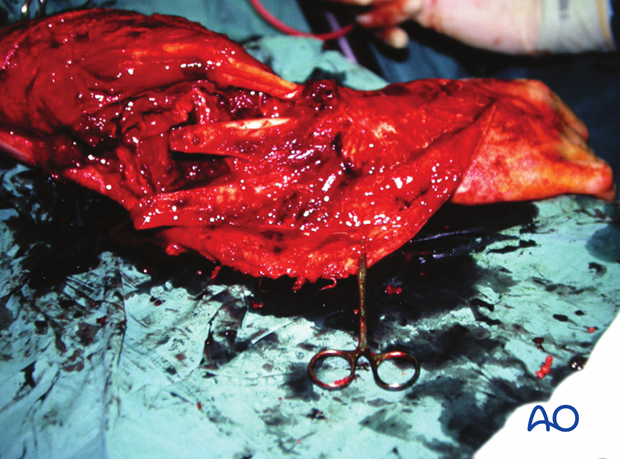
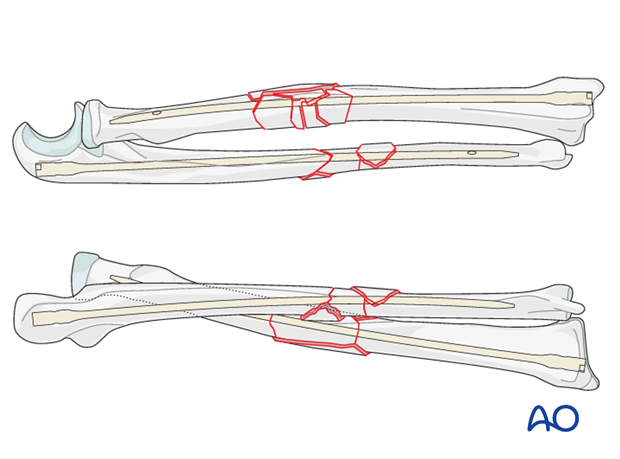
This clinical image shows a major crush injury of the forearm with multifragmentary fractures of both bones.
The same case after surgical debridement and before intramedullary nailing of both bones.
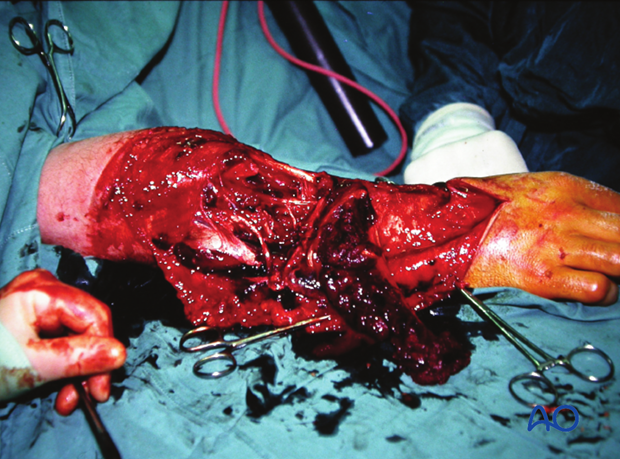
Early healing after split–skin grafting. The patient went on to bony union but there was considerable functional compromise related to the extreme severity of the soft-tissue injury.

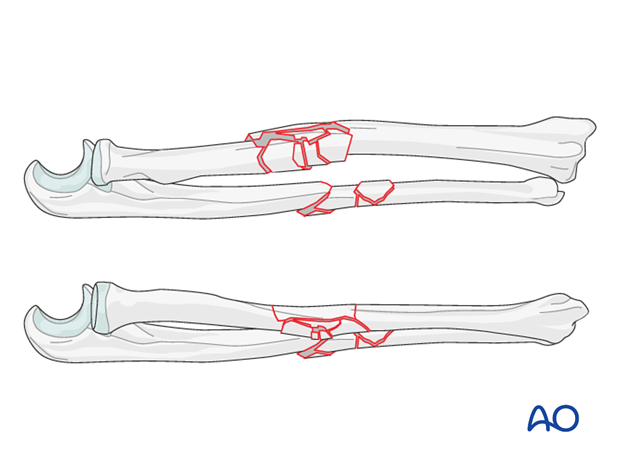
In multifragmentary both bone fractures, where one of the bones has an intact segmental fracture, anatomical reduction and absolute stability may be possible in that bone, provided the soft-tissue envelope permits. However, in the presence of limb-threatening soft-tissue injury the achievement of this goal may not be possible, and this may constitute an indication for locked intramedullary nailing.
When both bones have fragmentary segmental fractures, the multifragmentary zone in each bone precludes anatomical reduction and absolute stability.
We shall consider only these fractures in this section on nailing.
Additional relative indications
Further relative indications may be:
- Certain segmental fractures
- Gunshot fractures with severe comminution
- Refractures of the ulna after plate removal
See: A Hofmann, MH Hessmann, L Rudig (2004) Intramedullary osteosynthesis of the ulna in revision surgery. [Article in German] 107(7):583-92 - Pathological fractures
Limitations and contraindications
- Fractures occurring less than 3 cm from the proximal or distal end of the bone
- Canal diameter smaller than 3 mm
- Preexisting forearm deformity
- Active infection
Which bone should be addressed first?
This issue is controversial. On one hand, the preference could be to start with the radius with its more complex shape, or with the more comminuted fracture pattern, in order to facilitate the manipulation of the forearm. Nailing the other bone first might limit this possibility.
On the other hand, starting with the easier fracture, or the more simply shaped ulna, may assist in restoring length and alignment of the forearm.
In certain circumstances, depending on soft-tissue compromise and fracture morphology, nailing of one bone and plating of the other bone is an option.
2. Preoperative planning
It is crucial to select nails of appropriate lengths and to contour them accurately. Inappropriate nail selection or shape can result in malalignment, fracture distraction, and functional loss.
Accurate nail selection and contouring can be performed, based on one of the following methods:
1) X-ray method
X-rays of the contralateral forearm may be obtained to determine the lengths and diameters of both bones, as well as the shape of the radial bow. Some nails are provided with a template for the contralateral side. The magnification effects should be taken into consideration.
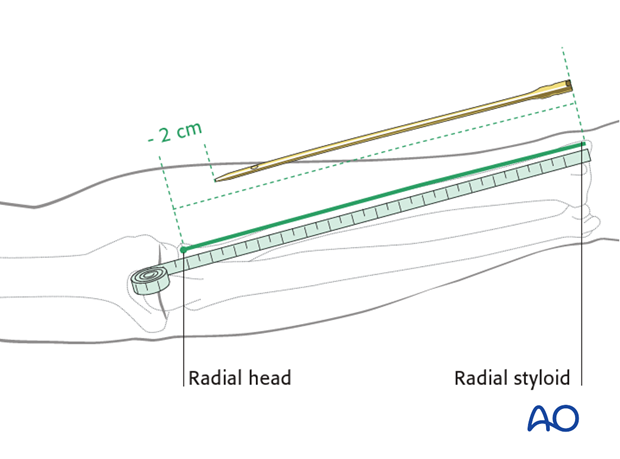
2) Measuring tape method
On the uninjured forearm, measure the distance from the tip of the olecranon to the ulnar styloid and subtract 1 cm to indicate the desired length of the ulnar nail.
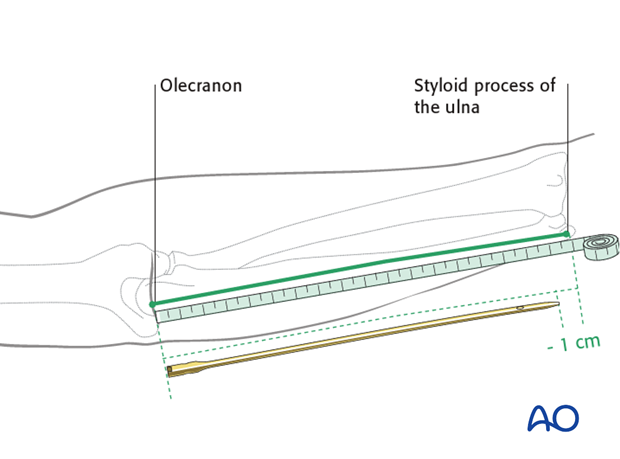
For the radius make the measurement from the tip of the radial styloid to the radial head and subtract 2 cm to indicate the desired length of the radial nail (the radial head may be difficult to palpate).
3) Intraoperative method
Place a nail of known length against the injured bone, while pulling the limb to length using manual traction. Image intensifier views of the length and fit of the nail are used to calculate the desired length of the nail to be used.
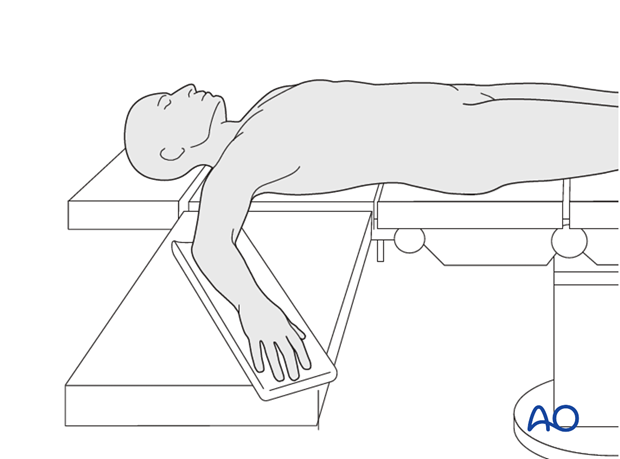
3. Patient preparation
This procedure is normally performed with the patient in a supine position.
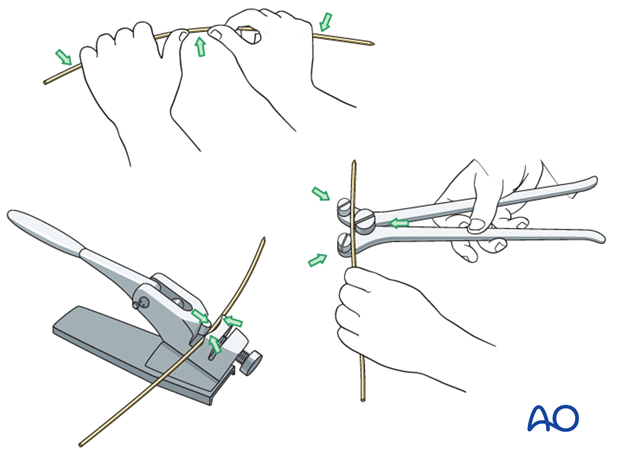
4. Bending
All flexible nails and some rigid nails are manufactured straight. Straight rigid nails need to be bent to match the contour of the bone, according to the preoperative plan/template. It is self-evident that contouring the radial nail is mandatory, but there is a less obvious bow to the proximal part of the ulna in the coronal plane; this might necessitate some contouring in cases of more proximal ulnar fractures.
Some rigid nails are prebent and others require the use of a mechanical bender.
5. Approach and entry point
Ulnar nails are always inserted in an antegrade fashion with the nail entry point at the tip of the olecranon process.
Radial nails are always inserted in a retrograde fashion with the entry point radial to Lister’s tubercle.
The entry point for ulnar nails is almost independent of the specific nail design, but the radial entry point may vary according to the nail design.
Click here for more detailed descriptions of the approaches.
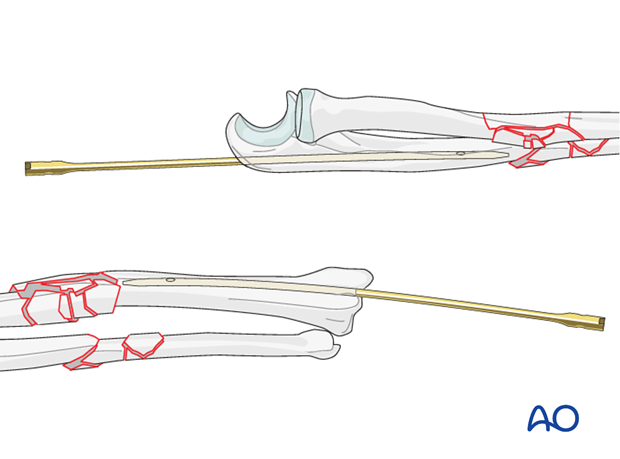
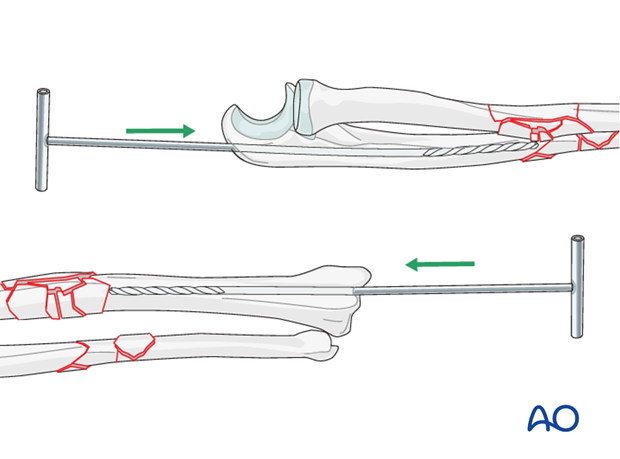
6. Closed versus open reduction
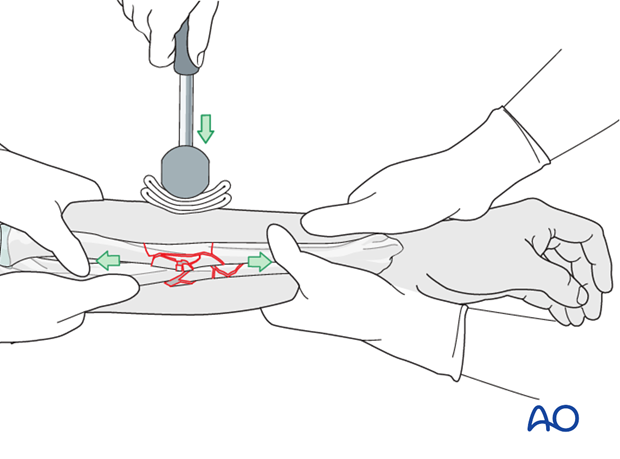
Closed reduction is preferable if possible, in order to preserve the blood supply of the fracture zone. This can be achieved by manual traction and direct pressure over the fracture site.
When fracture fragments are locked in malposition or in the presence of soft-tissue interposition, a limited open reduction should be used.
Open approach
Use the standard approaches to the forearm.
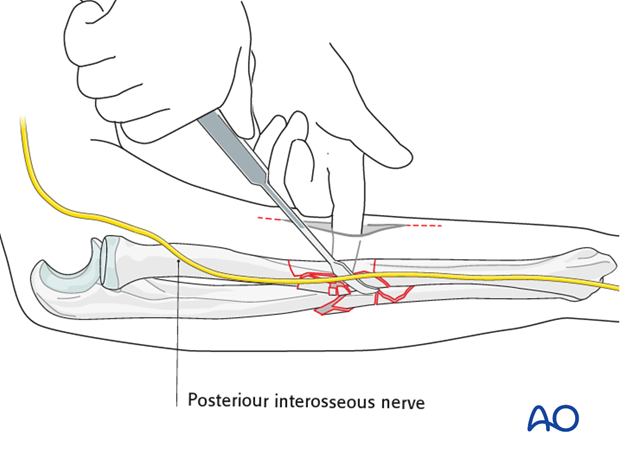
The incision needs only to be long enough to identify and protect neurovascular structures.
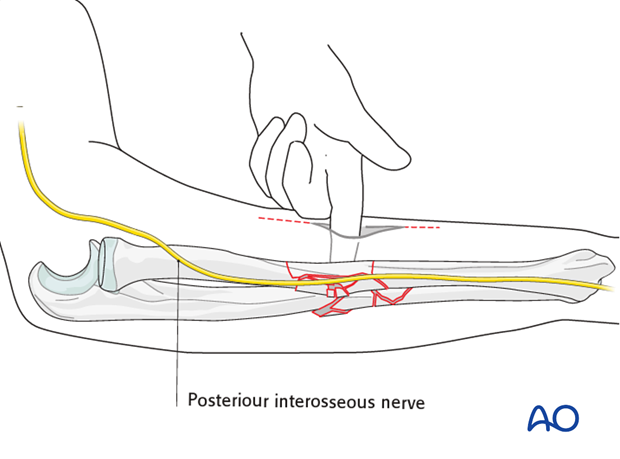
It is unnecessary and undesirable to strip the bone entirely, but rather use a blunt dissector, or a similar instrument, and a finger to align the fracture fragment, in order to allow the nail to pass through.
Note: Be aware of the posterior interosseous nerve in proximal radial fractures.
7. Canal preparation
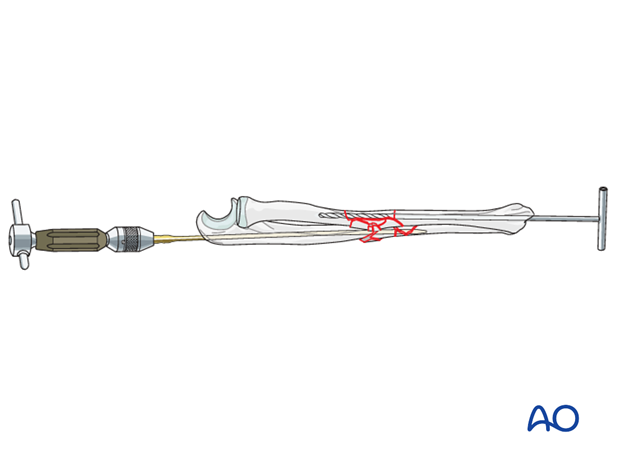
Whenever open, or closed, nailing is performed, both medullary canals should be prepared before either bone can be definitively nailed.
In most cases reaming needs to be performed due to the narrowness of the intramedullary canals and the risk of nail incarceration, or iatrogenic fracture.
In some nail designs, the reamer can be used to aid reduction by levering the fragments.
8. Nail insertion
After the canals have been prepared and both fractures have been reduced, the nails can be inserted sequentially. While inserting a nail into one bone, the other bone should be provisionally stabilized by leaving a guide wire or a reamer in situ. With small diameter forearm nails, or nails without guide wires, the fracture may need to be reduced again, after removal of the reamer.
Remember that a fixed nailed bone may hinder the reduction of the other bone.
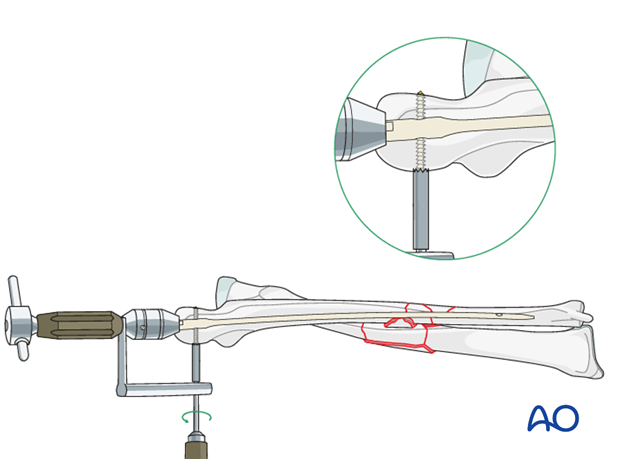
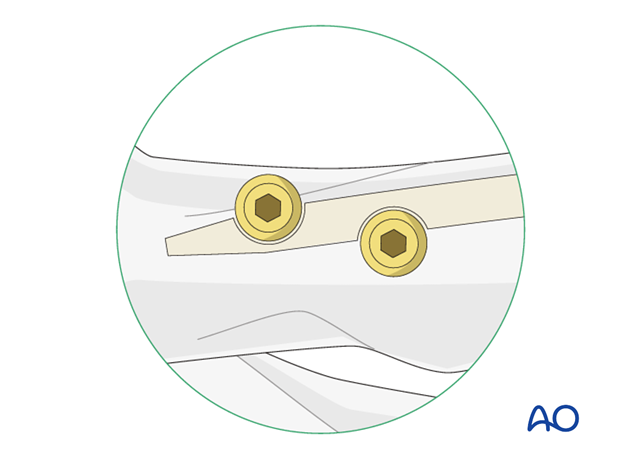
9. Locking
Since rotational stability is hard to achieve with forearm nails, locking is important.
Due to the shape and size of the bones, and the risk to neurovascular structures, locking is more demanding compared to other long bones.
In order to overcome the challenges of locking a forearm nail, different mechanisms are available. Such mechanisms include:
- Targeting devices
- Threaded cap principle
- Set screw principle
Targeting device
Some nails use an interlocking mechanism similar to femoral and tibial nails. Interlocking screws are inserted through a targeting device.
Threaded cap principle
A threaded nail cap is inserted into the end of the nail.
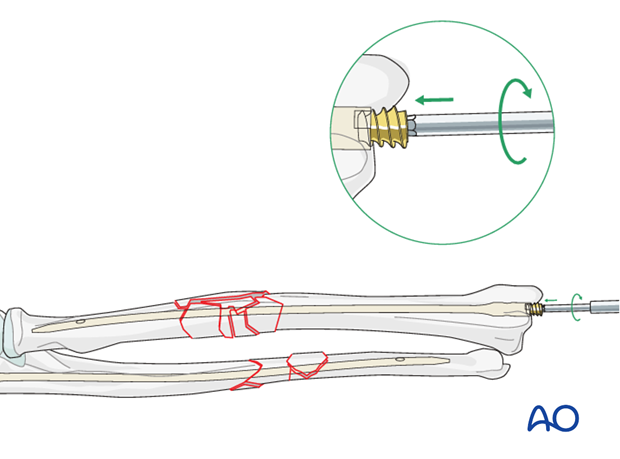
Set screw principle
One or more set screws engage grooves in the nail and thereby block rotation of the nail within the bone.
10. Check stability and range of motion
Check the ranges of motion of the elbow and wrist, and the arc of supination/pronation. Check the position of the nails and screws with the aid of image intensification. Make sure that all interlocking screws are properly placed and that there is no excessive prominence of the hardware.
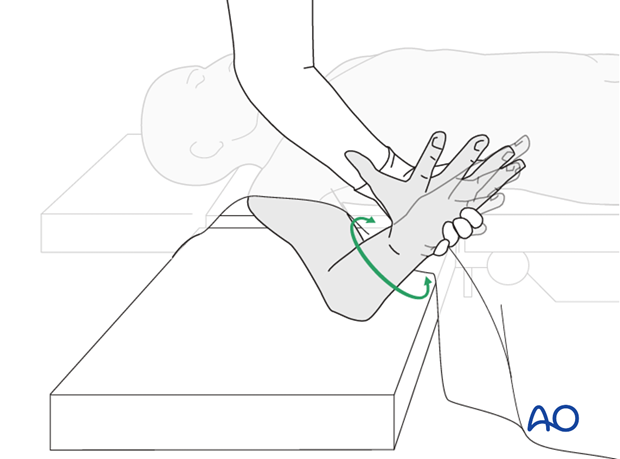
11. Assessment of Distal Radioulnar Joint (DRUJ)
Before starting the operation the uninjured side should be tested as a reference for the injured side.
After fixation, the distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
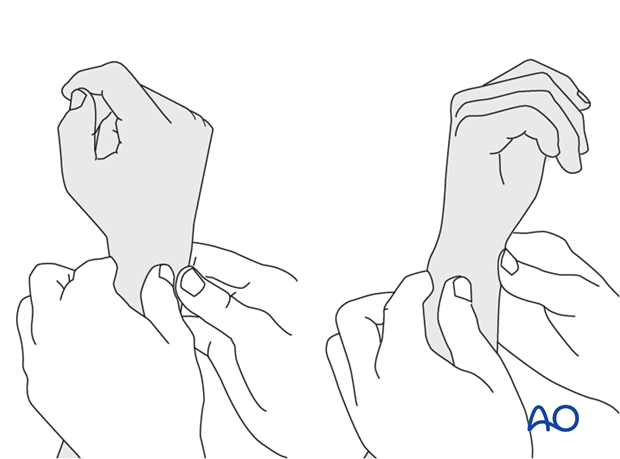
Method 1
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
This is repeated with the wrist in full supination and full pronation.
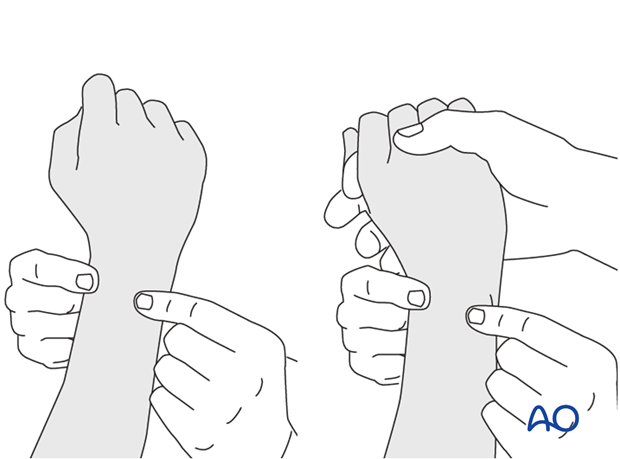
Method 2
In order to test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
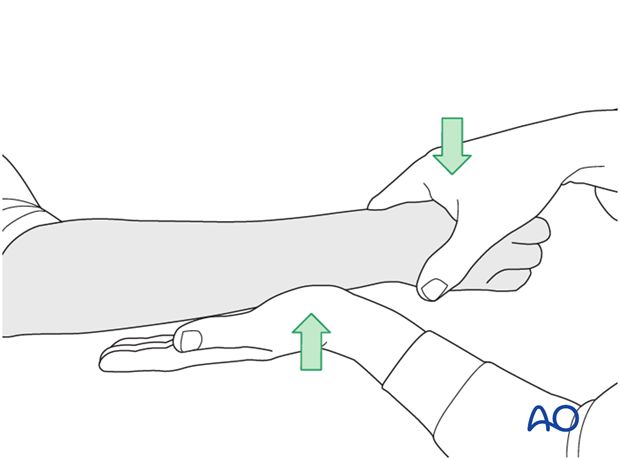
...while the forearm is passively put through full supination...
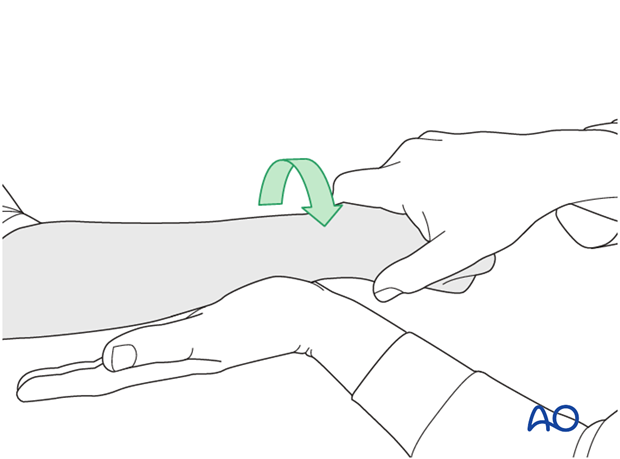
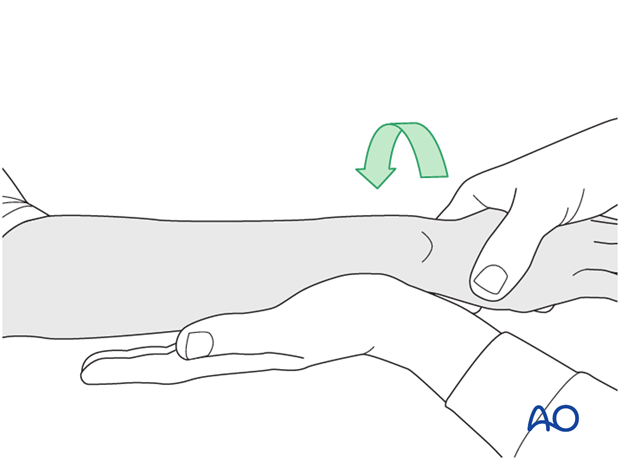
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.
12. Pitfalls
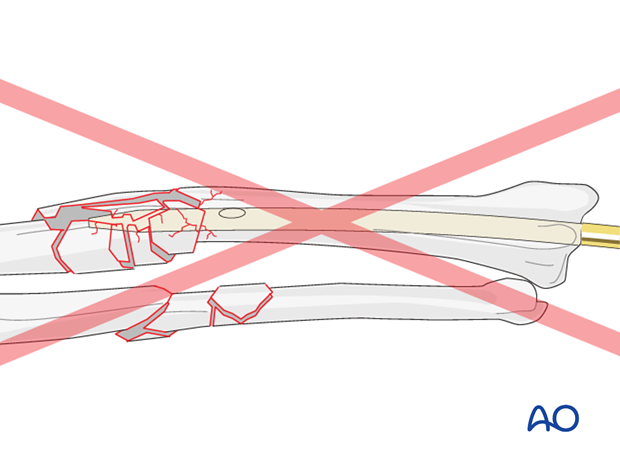
Nail and canal mismatch
A nail too thick for the canal may result in further comminution, incarceration of the nail in the bone, or distraction of the fracture zone. To prevent such complications, canal preparation and selection of the correct nail diameter are crucial.
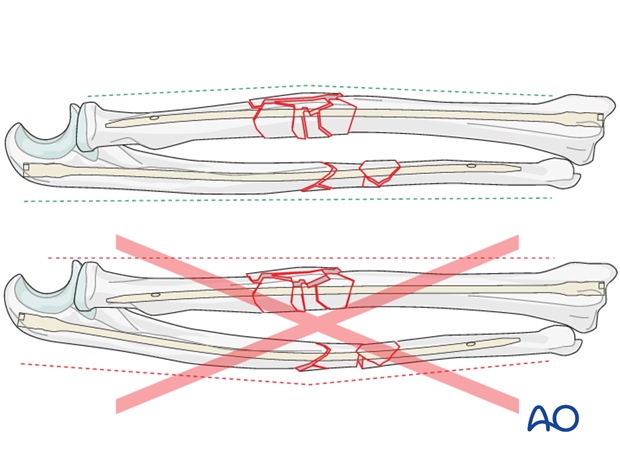
Malreduction
Malreduction of one bone might produce malalignment of the other bone, e.g., an excessively curved ulna will result in a straight radius.
Soft-tissue compromise
In the ulna, excessive prominence of the nail may interfere with the function of the triceps tendon and cause subcutaneous tissue irritation.
While inserting the radial nail, care should be taken to protect the extensor tendons and the nail should not protrude outside the dorsal radial cortex, in order to avoid chronic irritation of the overlying tendons.
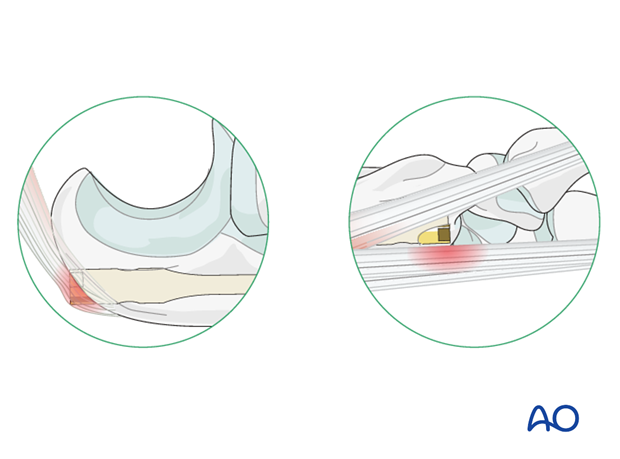
The same principles apply to interlocking screws.
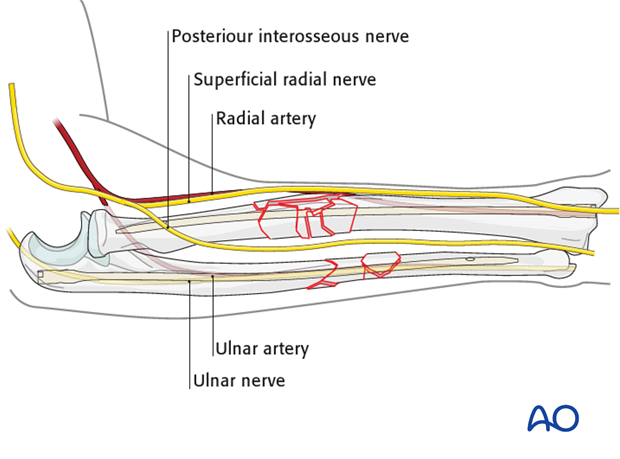
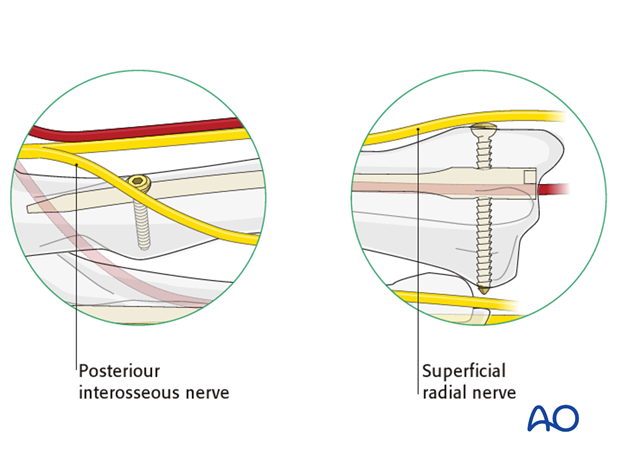
When inserting interlocking screws, great care should be taken to prevent damage to neurovascular structures. An example is the posterior interosseous nerve at the proximal part of the radius.
Proximal interlocking screws in the radius may endanger this nerve. A skin incision is made and then progressively deepened by spreading a forceps and advancing the retractors layer by layer until the bone is reached.
In distal locking of the radius using screws, the dorsal branch of the superficial radial nerve may be at risk. Therefore, a large enough incision, developed as above and with an adequate bone exposure is mandatory prior to screw insertion.
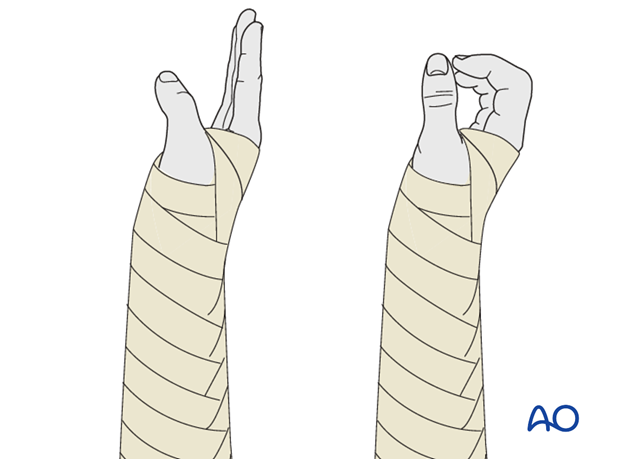
13. Postoperative treatment of a multifragmentary fracture treated with nailing
Functional aftercare
Following stable fixation, postoperative treatment is usually functional.
Since soft-tissue swelling and edema are associated with these high-energy fractures, temporary immobilization with a well-padded, bulky splint for 10-14 days is advised to allow adequate soft-tissue healing. During this period, elevation, gentle finger motion, active and passive, together with elbow flexion/extension and shoulder motion, can be started, if a stable fixation and/or static locking has been achieved.
If the stability of the fixation is questionable, splinting should continue for 4-6 weeks.
Lifting and resisted exercises are restricted until radiographic signs of healing appear. More intensive exercises, such as progressive resisted exercises and return to sports should be delayed until at least 3-6 months after surgery.
Follow-up
Close postoperative follow-up is required in these fractures that have been treated by means of relative stability. Secondary bone healing with callus formation is anticipated and early signs of delayed union should alert the surgeon to consider secondary interventions, such as bone grafting.
Follow-up x-rays should be obtained according to local protocol. X-rays to assess fracture position are usually taken at 1, 2, and 4 weeks after operation. Subsequent x-rays are usually taken to assess bony healing at appropriate intervals from 6-8 weeks, depending on the fracture configuration and potential for healing.
Implant removal
Unlike plating, the risk for refracture after nail removal is low. However, routine removal of these implants is unnecessary unless the hardware is symptomatic.













