Compartment syndrome
1. Introduction
Principles
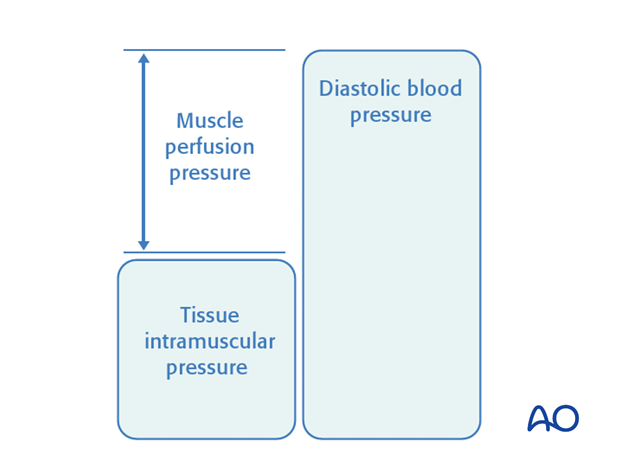
Compartment syndrome occurs when the pressure within a closed osteo-fascial muscle compartment rises above a critical level. This critical level is the intramuscular tissue pressure which collapses the capillary bed and prevents low-pressure blood flow through the capillaries and into the venous drainage. Normal tissue pressure is 0-10 mm Hg. The capillary filling pressure is essentially diastolic arterial pressure. When tissue pressure approaches the diastolic pressure, capillary blood flow ceases. A number of studies have shown that if diastolic arterial pressure is not more than 30 mm Hg above intramuscular tissue pressure, compartmental capillary blood flow is significantly obstructed and severe hypoxia occurs in muscle and nerve tissue.See also:
- Gourgiotis S, Villias C, Germanos S, et al (2007) Acute limb compartment syndrome: a review. J Surg Educ; 64(3):178-86.
- Mabee JR (1994) Compartment syndrome: a complication of acute extremity trauma. J Emerg Med; 12(5):651-6.
The critical measurement is muscle perfusion pressure (MPP), the difference between diastolic blood pressure (dBP) and measured intramuscular tissue pressure. (MPP has also been called ΔP, to indicate the difference between diastolic blood pressure and intramuscular tissue pressure.) This difference in pressure reflects tissue perfusion dynamics far more reliably than the absolute intramuscular pressure in isolation.
- Muscle tolerates short periods of hypoxia, but after a few hours, progressive necrosis begins.
- An arterial injury may cause compartmental tissue ischemia. After blood flow is restored, capillaries leak and ischemic muscle swells. Such reperfusion injury is another cause of compartment syndrome.
2. Diagnosis
Symptoms
The diagnosis of this severe complication rests on two factors: a high index of suspicion and a thorough understanding of its variable clinical presentation.
In a conscious and alert patient, there will be unrelenting, worsening pain, greater than expected for the particular injury, and not related to limb position.
Commonly there is a relatively pain-free interval, perhaps a few hours following fracture treatment, before such pain develops.
The level of pain can often be judged by increasing requests for ever-stronger analgesia, or increasing use of patient-controlled analgesia (PCA) systems.
Any nerve traversing the involved compartment will become hypoxic, often causing numbness and tingling in the nerve distribution. After some hours, ischemic nerves cease to function and the pain resolves.
Signs
Clinical features of an impending muscle compartment syndrome include tenderness and induration of the affected compartment, increase in the pain on passive muscle stretching, possible sensory (and later motor) deficit in the territory of a nerve traversing the compartment, and muscle weakness.
The presence of a distal pulse does not exclude compartment syndrome, because in a normotensive patient the muscle pressure rarely exceeds the systolic level.
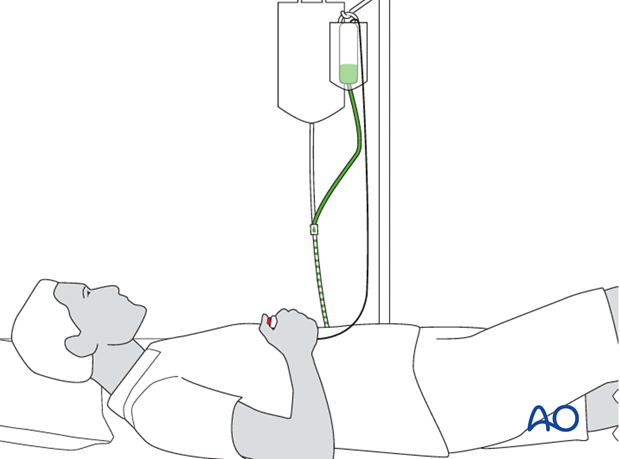
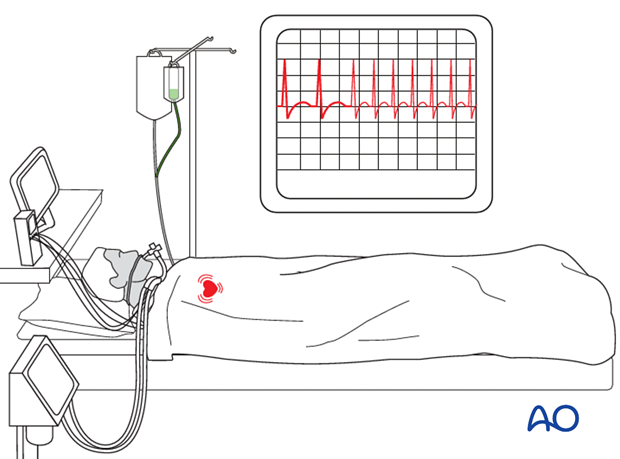
In an unconscious, drugged, or intoxicated patient, it is easy to miss a compartment syndrome. Any visible limb swelling becomes a vital clue as does persistent, unexplained tachycardia. For such patients, direct tissue pressure measurement is very helpful for diagnosis.
3. Treatment principles
Fasciotomy
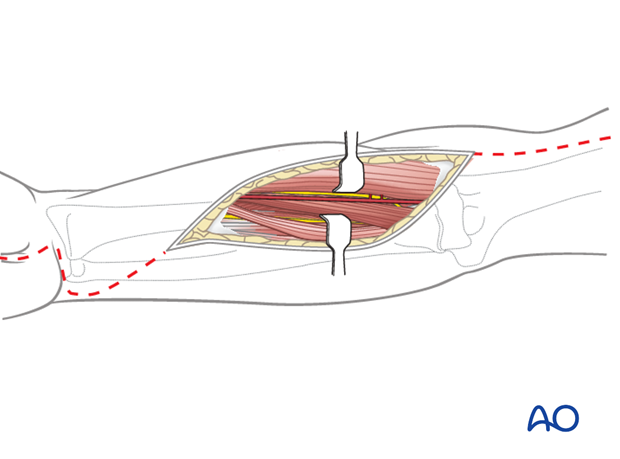
Once a diagnosis of muscle compartment syndrome has been established, or even strongly suspected, each of the relevant compartments must be decompressed fully by extensive dermatofasciotomy, as a matter of urgency.Be aware that there are three main compartments in the forearm (mobile wad, anterior compartment, and dorsal compartment – with each of the latter two being divided into a superficial and a deep portion).
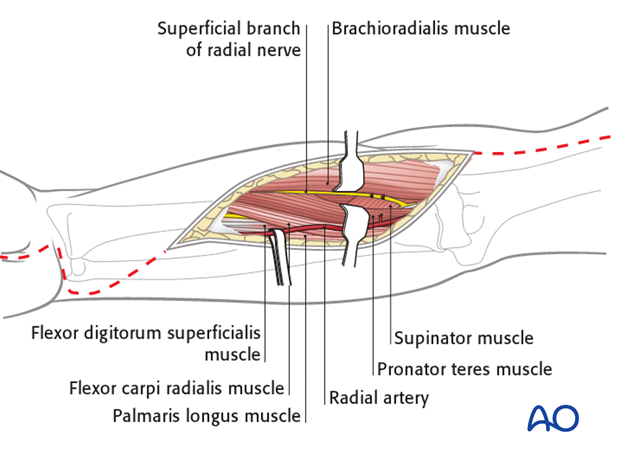
The approach to the relevant muscle compartment will be based on one of the standard surgical approaches in the forearm, respecting the important neurovascular structures.
The procedure should include decompression of the median nerve in the carpal tunnel and the ulnar nerve in the distal forearm.
Evidence
Forearm shaft fractures have been reported in 34% of a recent series of patients with compartment syndrome of the forearm [Duckworth]. A routine approach to the different compartments of the forearm may differ from the approaches for the fixation of the shaft fractures. Different fasciotomy approaches have been described [Kalyani] with no specific variation of the approaches when fractures and compartment syndrome need to be treated concurrently. It has been reported that a modified anterior approach of Henry is most commonly used [Kalyani]. An additional posterior fasciotomy has been reported in 20-26% of cases and carpal tunnel release in 49-54% of cases [Duckworth, Kalyani].
Gelberman et al in 1978 measured the pressure in the different forearm compartments before and after various fasciotomy techniques. They found no firm fascial division between the anterior compartments of the forearm and also that different anterior fasciotomy designs resulted in adequate reduction of all anterior compartment pressures.
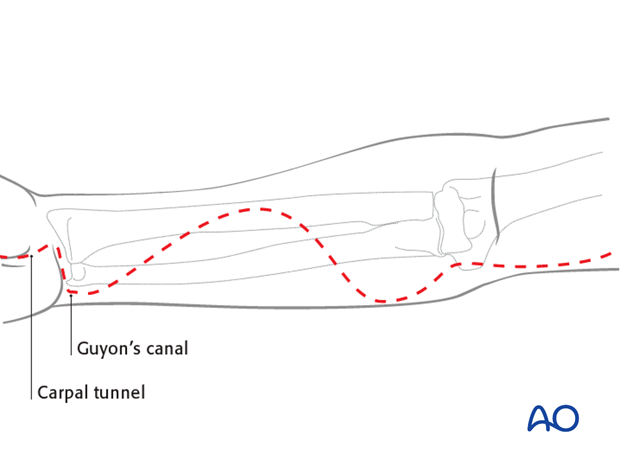
Brostrom et al. reported on 16 patients with acute compartment syndrome in forearm fractures. They treated the patients with a curved anterior skin incision extended to open the carpal tunnel and the canal of Guyon.
4. Suggested modified approach
The standard anterior fasciotomy incision extends over the carpal tunnel and Guyon's canal distally (in order to decompress the median and ulnar nerves), continues with a curved incision towards the radial side of the mid-forearm and back to the ulnar side of the proximal forearm. It may be extended proximally across the elbow if wider access is required.
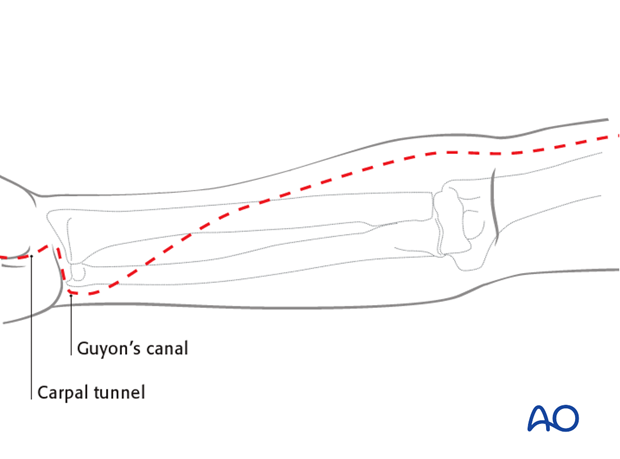
Proximal radial fracture
In proximal fractures of the radius, the fasciotomy incision continues proximally on the anterolateral aspect of the forearm, as in a standard Henry approach described previously. If needed, the fasciotomy should cross the anterolateral aspect of the elbow. This will maintain coverage of the neurovascular bundle running through the cubital fossa in those cases where the wound is left open. It should be taken into account that a straight incision across the anterior elbow may result in contracture of the joint and this problem should be dealt with early in the rehabilitation process.
Proximal and midshaft radial fractures
A combined approach for both indications may call for an approach to these fractures different from those previously described. In the mid-forearm, the curved incision with its apex on the anterolateral aspect of the mid-forearm will expose the flexor compartment and enable the fixation of the radial fracture.
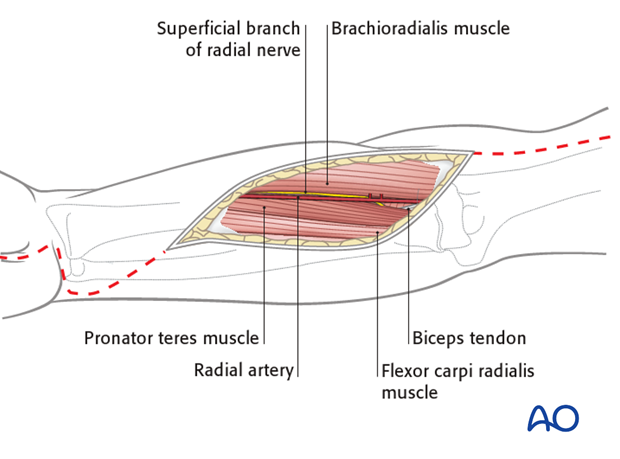
Through this part of the incision, the radial fracture may be approached between the radial artery and the flexor carpi radialis muscle. The artery is retracted radially (and not ulnarly as with the standard approach to the midshaft radius described previously). The flexor muscle mass is exposed and the overlying fascia released. This includes the finger and wrist flexors, as well as the median nerve. The nerve should be identified between the deep and superficial flexor muscles and protected, gently retracting it ulnarly with the flexor muscle mass. The radial artery is retracted radially with the brachioradialis muscle and superficial radial nerve, to expose the pronator teres and flexor pollicis longus muscles on the radius.
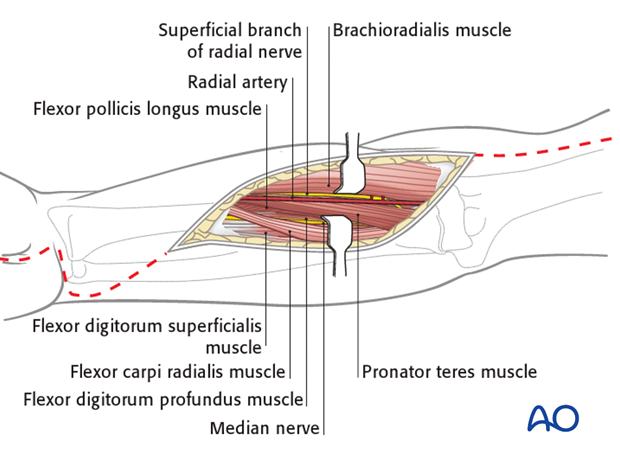
For more proximal fractures, the approach to the radius is similar to the upper part of the anterior approach (Henry), but the radial artery may need to be mobilized by dividing the recurrent branches on its lateral aspect to permit the artery to be retracted in a medial direction.
Distal radial fracture
Caution should be taken when exposing the radius distally, due to the path of the median nerve and its cutaneous branch, which runs along the ulnar side of the flexor carpi radialis tendon.
In cases where a combined approach to the fasciotomy and fracture may be inadequate, as with a distal radius fracture, other options may be chosen such as the use of an external fixator after closed reduction of the fracture, or a dorsal approach for plate fixation of the distal radius.
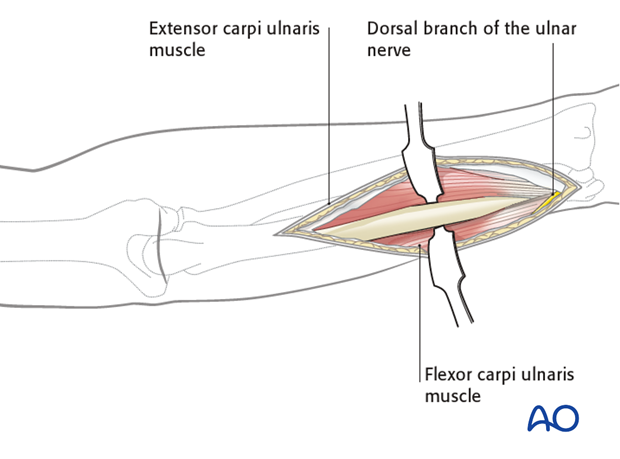
Ulnar fracture fixation and posterior fasciotomy
An additional posterior approach to the extensor compartment may not be necessary where a separate approach to the ulnar fracture is performed. Releasing the extensor carpi ulnaris muscle belly from the posterior aspect of the ulna may be sufficient, although there are no data to support this and a clinical decision has to be made during the procedure.
5. References
Broström LA, Stark A, Svartengren G. (1990) Acute compartment syndrome in forearm fractures. Acta Orthop Scand. 61(1):50-3.
Duckworth AD, Mitchell SE, et al. (2012) Acute compartment syndrome of the forearm. J Bone Joint Surg Am. 16;94(10).
Gelberman RH, Zakaib GS, et al. (1978) Decompression of forearm compartment syndromes. Clin Orthop Relat Res. (134):225-9.
Kalyani BS, Fisher BE, et al. (2011) Compartment syndrome of the forearm: a systematic review. J Hand Surg Am. 36(3):535-43.













