CRIF - K-wire fixation
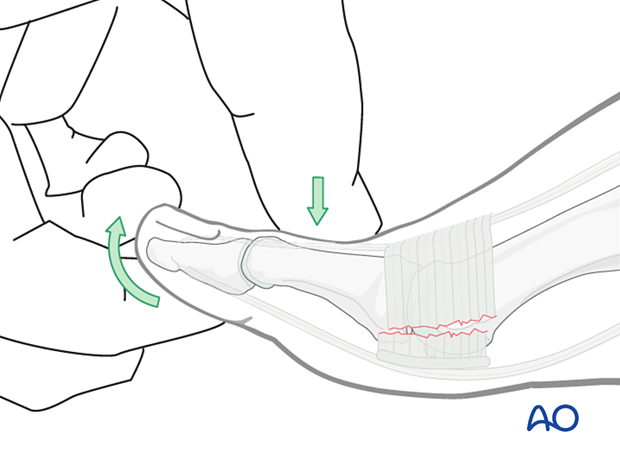
1. Closed reduction
Dorsal dislocation is most common due to the hyper-extension mechanism.
The reduction should be performed expeditiously under local anesthesia (digital block).
Impingement of the proximal phalanx base with the dorsal metatarsal neck may prevent spontaneous reduction.
The plantar plate and collateral ligaments may block reduction.
Dimpling may signify a complex dislocation where closed reduction may not be successful.
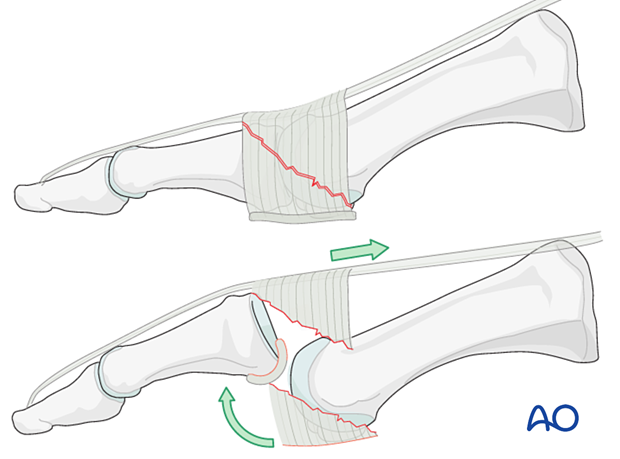
The proximal phalanx is extended, and traction is applied to free the inferior rim from its impingement on the metatarsal's dorsal surface.
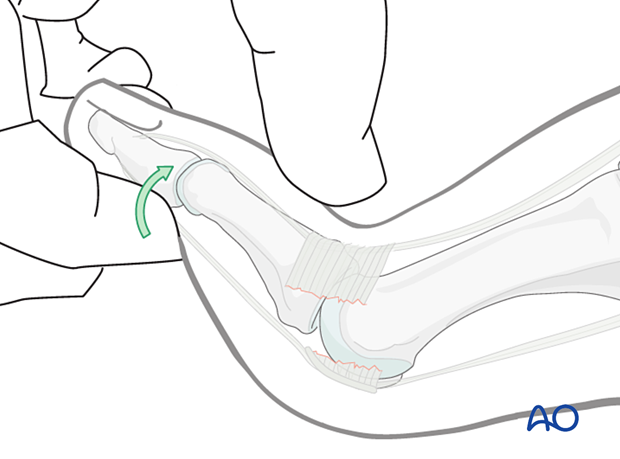
The toe is then translated in a plantar direction.
The MTP joint must be immobilized in an anatomical position to avoid a dorsiflexion contracture.
If the reduction is stable, K-wire fixation is not required, and alignment can be maintained by buddy taping.

Pitfall: interposition of the plantar plate
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.
Dislocation or injuries associated with the skin at risk requires immediate intervention regardless of the amount of soft tissue swelling.
2. K-wire fixation
There are two options to secure K-wire fixation.
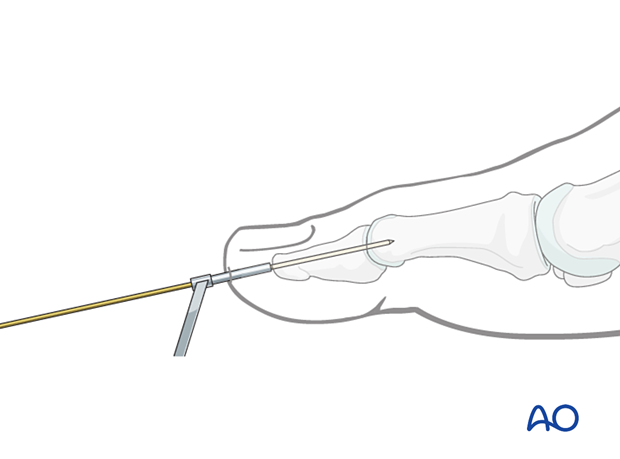
Option 1 : axial K-wire
IntroductionThe first option is to drive a K-wire through the toe, beginning just under the nail and then driving the K-wire in line with the toe's axis across the IP joint(s). The K-wire is advanced across the MTP joint while the joint is kept reduced.
In the hallux, two K-wires should be inserted.
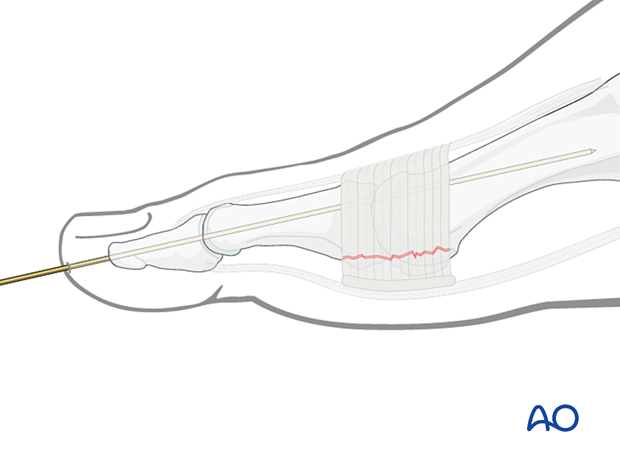
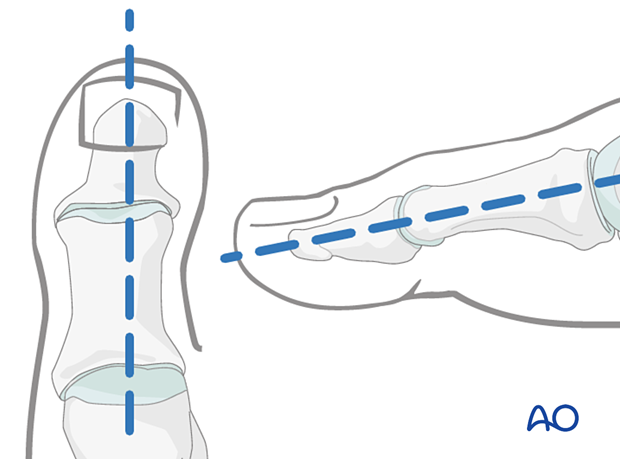
To avoid unnecessary radiation from image intensification, mark the K-wire's planned track with a skin marker on the distal phalanx in both the AP and the lateral aspects.
A 16 gauge hypodermic needle or a drill guide can be used to prevent the K-wire from slipping during insertion. Either finds good purchase on the distal phalanx tip and will ensure that the K-wire is inserted in the center and along the longitudinal axis of the phalanx.
If a K-wire is mistakenly inserted at an angle to the phalanx axis, it is recommended to leave it in until a second K-wire has been inserted in the correct orientation. Leaving the first K-wire in place prevents the second wire from going unintentionally along the wrong track.
In the lesser toes, this may not be possible.
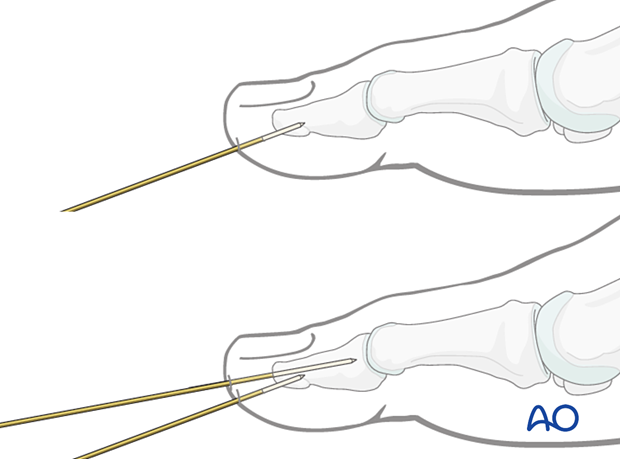
Reduce the MTP joint and drive the K-wire across the joint into the metatarsal.
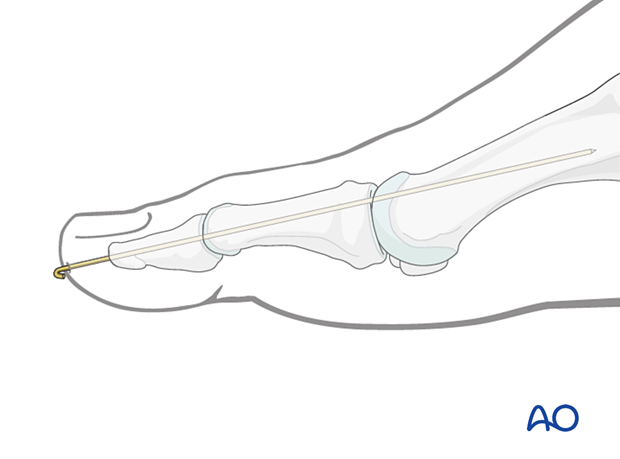
Cut the K-wire so that it protrudes through the skin, about 1 cm from the tip of the finger. Bend its end to form a tight U-configuration or add a pin cap to prevent catching on clothing.
Leaving the K-wire to protrude through the skin in this way has the advantage of its being easy to remove. The disadvantages are patient discomfort and the risk of pin-track infection.
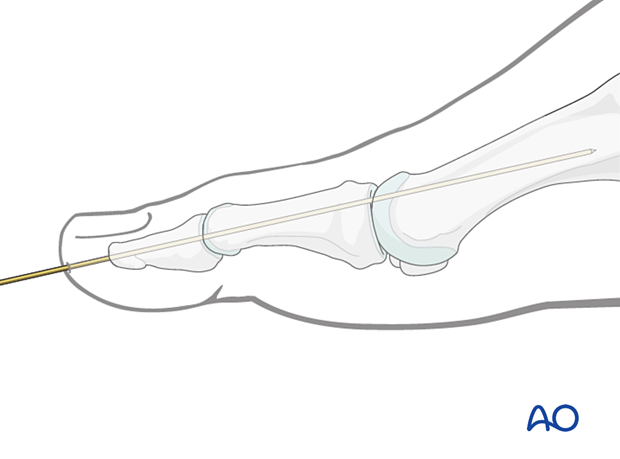
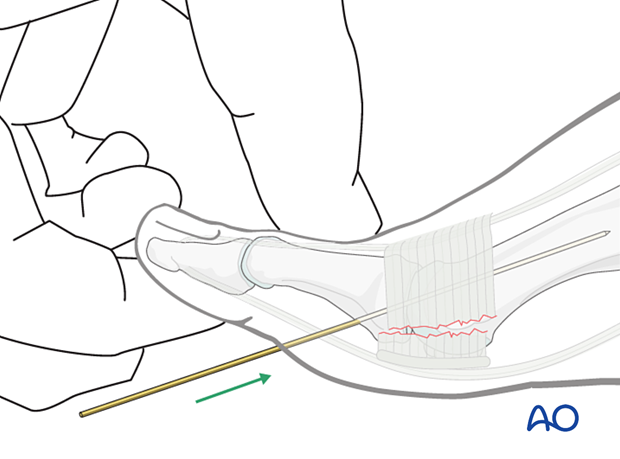
Option 2 : K-wire inserted through the base of the proximal phalanx
The alternative option would be to drive a K-wire that catches the base of the proximal phalanx.
While the reduction is maintained, the K-wire is driven across the joint into the metatarsal shaft.
The difficulty with this option is catching the proximal phalanx base with the K-wire.
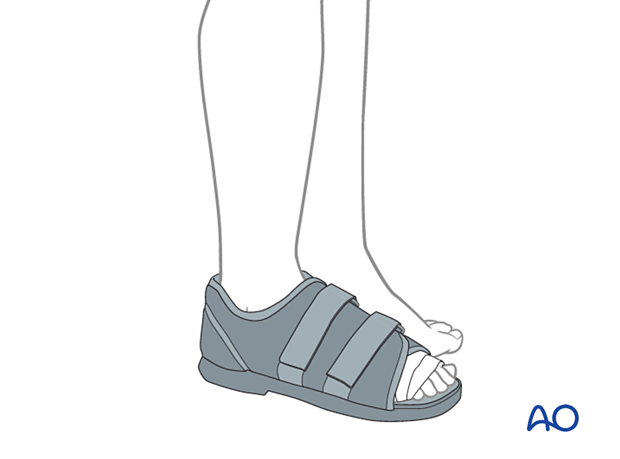
3. Aftercare
Instruct the patient in daily pin care to avoid pin-track infection.
The foot is immobilized in a hard-soled shoe.
If the pins are inserted through the plantar aspect, weight-bearing must be withheld until the pins are removed. If the pins are inserted through the toes into the metatarsals, then full weight-bearing can commence early, as soon as swelling and pain allow.
The foot should be elevated intermittently through the first two weeks with the application of ice packs to control edema.
The pin should be removed after 5–6 weeks.
4. Case
This case is a complex MTP dislocation with interposed soft tissues, making a closed reduction impossible.
AP and oblique view before open reduction

Lateral view before reduction

Lateral view following a succesful open reduction
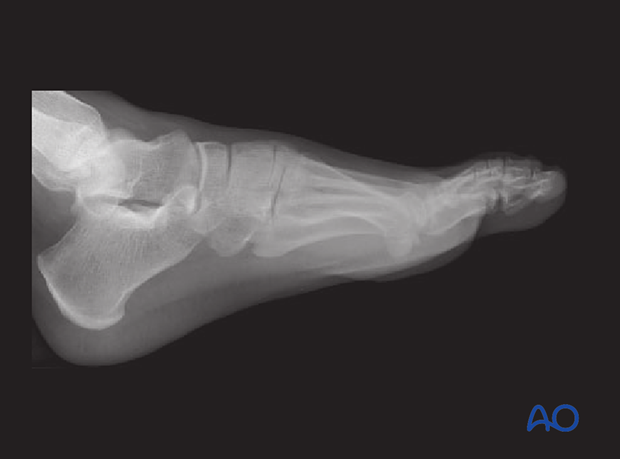
AP view showing the result of a successful open reduction














