Closed/open reduction with taping or rigid-soled shoe
1. Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.
Dislocation or injuries associated with the skin at risk requires immediate intervention regardless of the amount of soft tissue swelling.
2. Closed reduction
Dorsal dislocation is most common due to the hyper-extension mechanism.
The reduction should be performed expeditiously under local anesthesia (digital block).
Impingement of the proximal phalanx base with the dorsal metatarsal neck may prevent spontaneous reduction.
The plantar plate and collateral ligaments may block reduction.
Dimpling may signify a complex dislocation where closed reduction may not be successful.
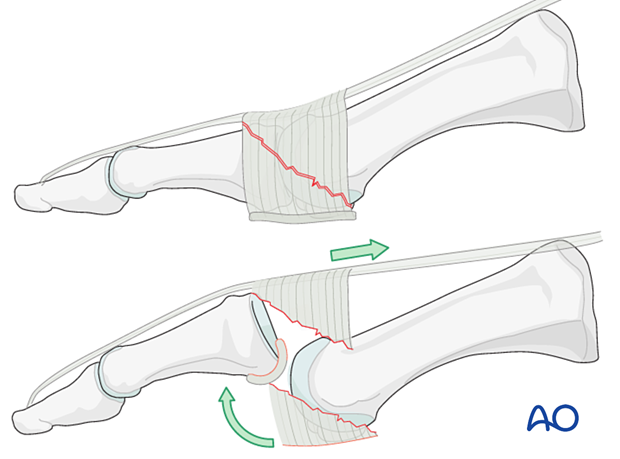
The proximal phalanx is extended, and traction is applied to free the inferior rim from its impingement on the metatarsal's dorsal surface.
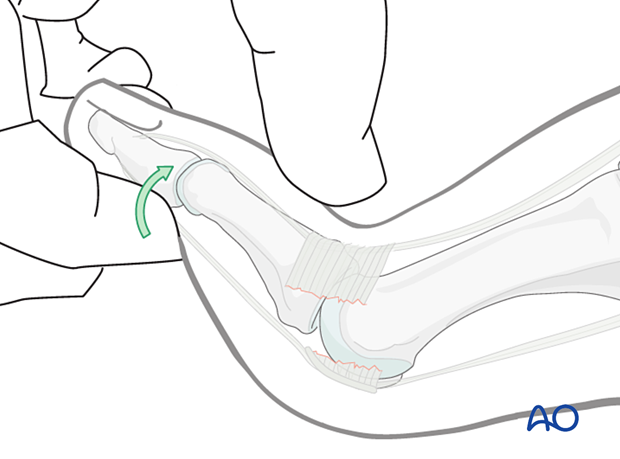
The toe is then translated in a plantar direction.
The MTP joint must be immobilized in an anatomical position to avoid a dorsiflexion contracture.
If the reduction is stable, K-wire fixation is not required, and alignment can be maintained by buddy taping.

Pitfall: interposition of the plantar plate
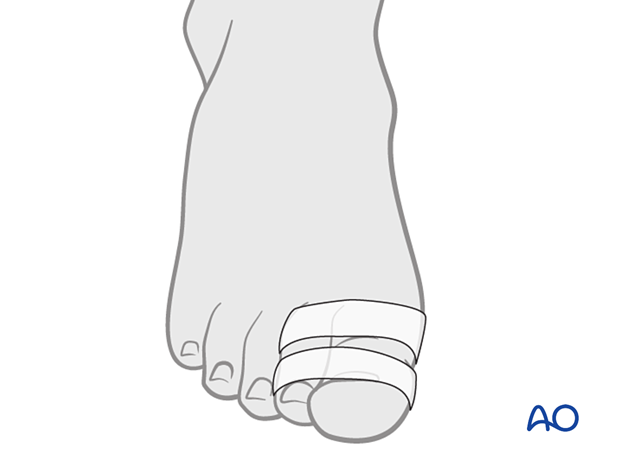
3. Buddy taping
The skin is cleaned, and 5–10 mm wide straps are fixed in a loop around the toes. Gauze may be placed between the toes to avoid maceration of the skin.
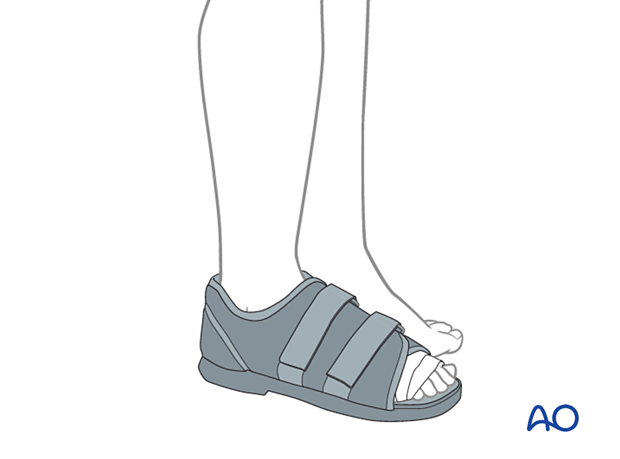
4. Aftercare
A stiff-soled orthosis, like a flat, rigid sole shoe, is used to protect the reduction and allow healing.
The symptoms usually settle over the first few weeks. The tape should be changed frequently to prevent maceration between the toes. Most patients are capable of doing this themselves.
Taping can be discontinued after 4–5 weeks.
5. Case
This case is a complex MTP dislocation with interposed soft tissues, making a closed reduction impossible.
AP and oblique view before open reduction

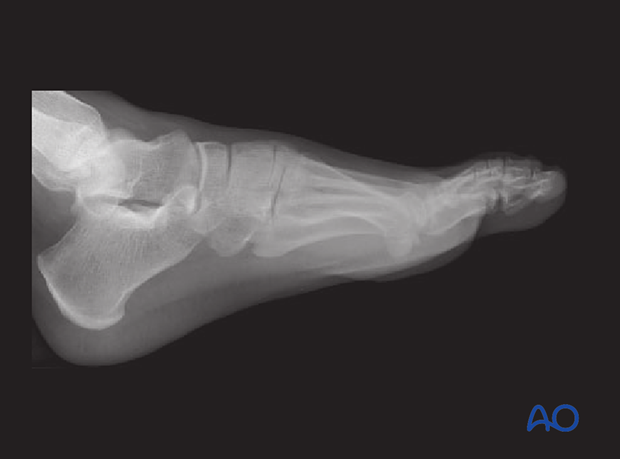
Lateral view before reduction

Lateral view following a succesful open reduction
AP view showing the result of a successful open reduction














