MIO - Bridge plating (DCS)
1. Principles
Note on illustrations
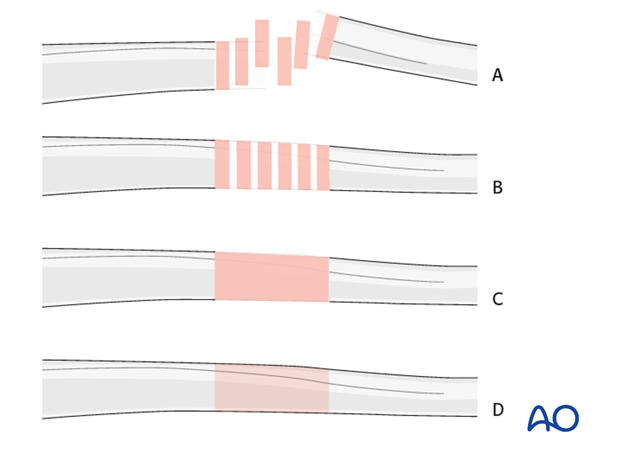
Throughout this treatment option illustrations of generic fracture patterns are shown, as four different types:
A) Unreduced fracture
B) Reduced fracture
C) Fracture reduced and fixed provisionally
D) Fracture fixed definitively
Bridge plating
Bridge plating uses the plate as an extramedullary splint, fixed to the two main fragments, leaving the intermediate fracture zone untouched. Anatomical reduction of intermediate fragments is not necessary. Furthermore, their direct manipulation would risk disturbing their blood supply. If the soft tissue attachments to the fragments are preserved, and the fragments are relatively well aligned, healing is enhanced.
Alignment of the main shaft fragments can be achieved indirectly with the use of traction and the support of indirect reduction tools, or indirectly via the implant.
Mechanical stability, provided by the bridging plate, is adequate for gentle functional rehabilitation and results in satisfactory indirect healing (callus formation). Occasionally, a larger wedge fragment might be approximated to the main fragments with a lag screw.
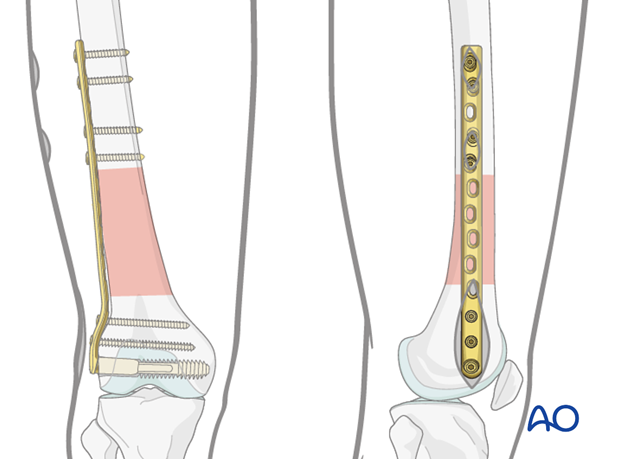
Minimally invasive osteosynthesis
Bridge plates inserted through a minimally invasive (MIO) approach leave the soft tissues intact over the fracture site. The incisions are made proximally and distally, and the plate is inserted through a sub-muscular tunnel. This normally requires fluoroscopic intensifier monitoring.

Reduction
It is important to restore axial alignment, length, and rotation.
Reduction can be performed with a single reduction tool (eg, large distractor), or by combining several steps (for example fracture table +/- external fixator, cerclage wires, +/- reduction via the implant, etc.) to achieve the final reduction.
The preferred method depends on the fracture and soft-tissue injury pattern, the chosen stabilization device, and the experience and skills of the surgeon.
If a large fragment has separated from the fracture zone and impaled the adjacent muscle, direct reduction may be required.
2. Patient preparation
The patient may be placed in one of the following positions:
3. Approach
For this procedure a MIO approach is used.
4. Preliminary reduction
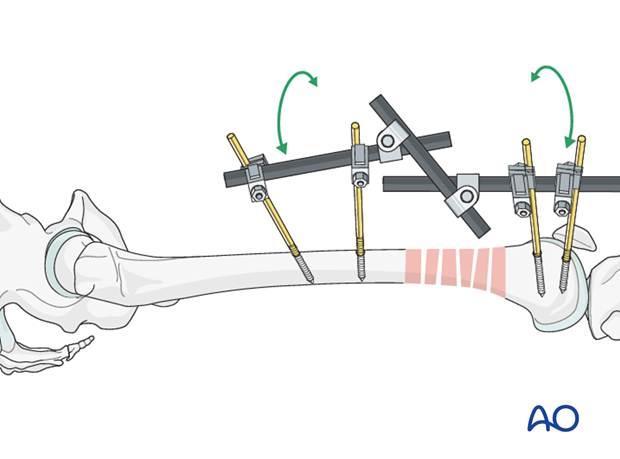
Reduction by external fixator or distractor
Sometimes, manual traction is not sufficient to achieve and hold preliminary reduction.
Then the use of an external fixator facilitates the reduction procedure and provide temporary alignment and stability for the bridge plating procedure.
Proximal and distal fixator screws should be inserted carefully not to conflict with the later plating procedure. For this purpose, anterolateral or anterior positions on the femur are safe.
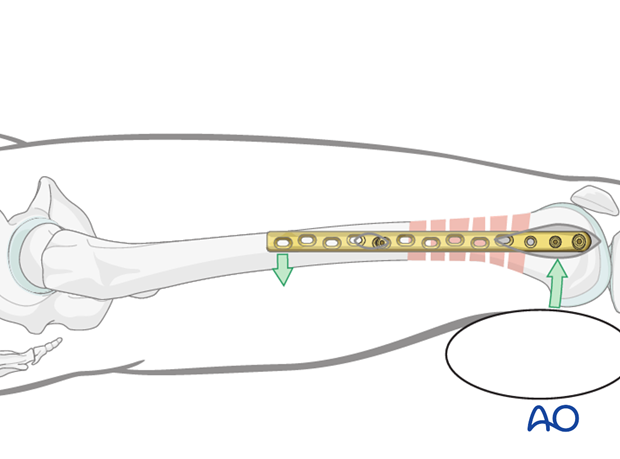
If no traction table is used, folded linen bolsters under the fracture zone may facilitate the reduction maneuver.
Teaching video
AO teaching video: Application of the large distractor
5. Plate fixation to the distal fragment
Guide wire insertion
As a first step, a guide wire for the condylar screw is inserted into the distal femur.
This is an extremely important step, because it determines the later plate positioning in two planes.
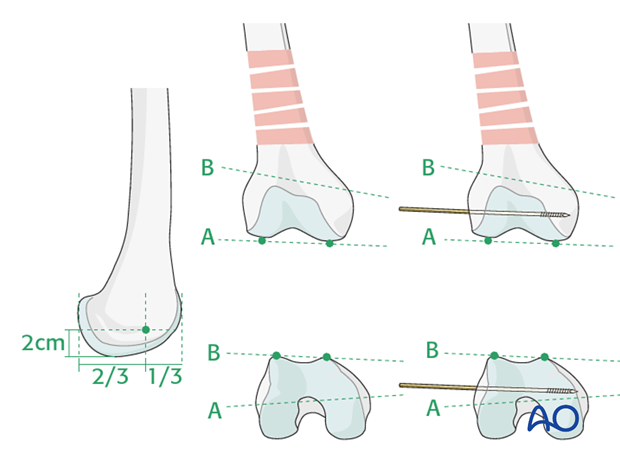
The guide wire for the cannulated condylar screw is inserted into the condylar mass from laterally. The entry point lies anterior to the mid-point between the anterior and posterior edges of the lateral femoral condyle, in line with the femoral shaft axis, and 2 cm proximal to the knee point.
The guide wire must be parallel to the plane of the tibio-femoral joint (line A) and, at the same time, parallel to the plane of the patello-femoral joint (line B).
Checking correct position of the guide wire
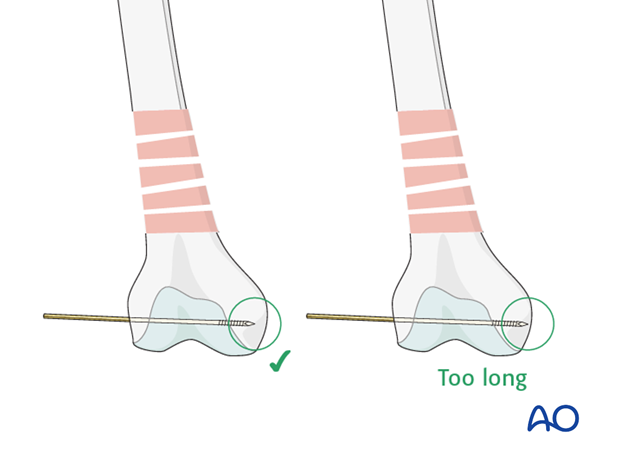
The correct positioning of the guide wire must be checked using image intensifier fluoroscopy. The depth of guide wire insertion is crucial. Remember that the cross-section of the distal femoral condylar mass is trapezoidal and slopes markedly on the medial side. The tip of the guide wire should just engage the medial cortex, and so will appear short of the medial condylar cortex on the AP intensifier image.
Screw length measurement
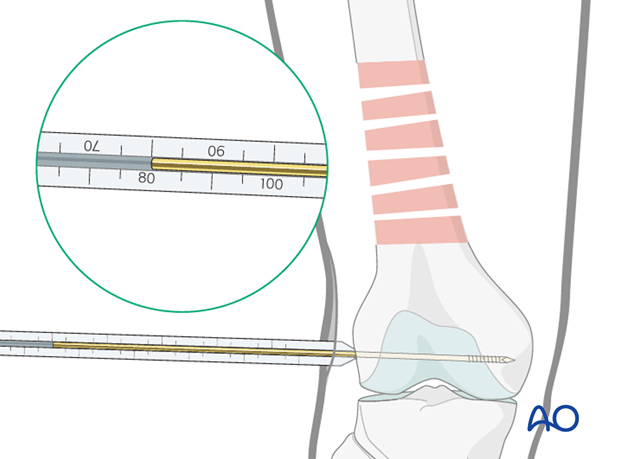
Next, the surgeon slides the direct measuring device over the guide wire and determines guide wire insertion depth and, thereby, the length of condylar screw required.
Drilling
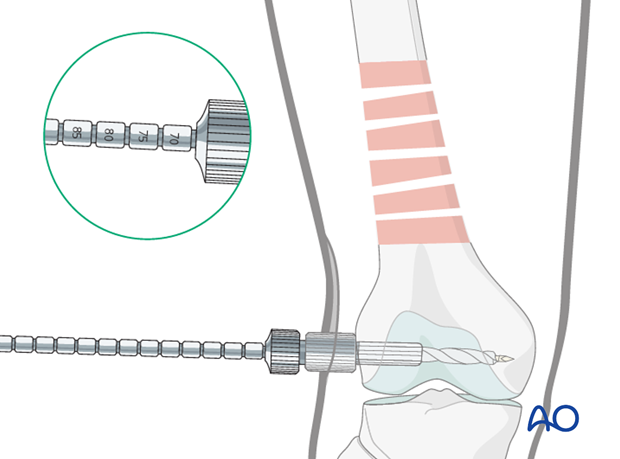
After assembling the DCS triple reamer and setting the reamer to the correct depth, the hole for the condylar screw is reamed over the guide wire.
Preliminary screw insertion
The following steps are recommended for the minimally invasive technique.
After tapping, the DCS screw is inserted over the guide wire in a manner so that its outer end is still visible outside the lateral cortex of the distal femur.
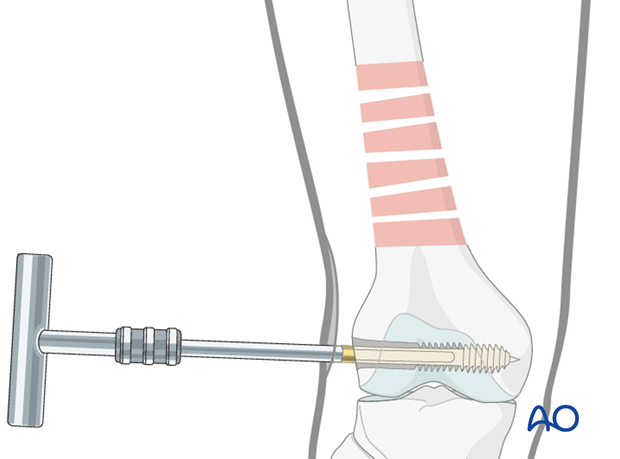
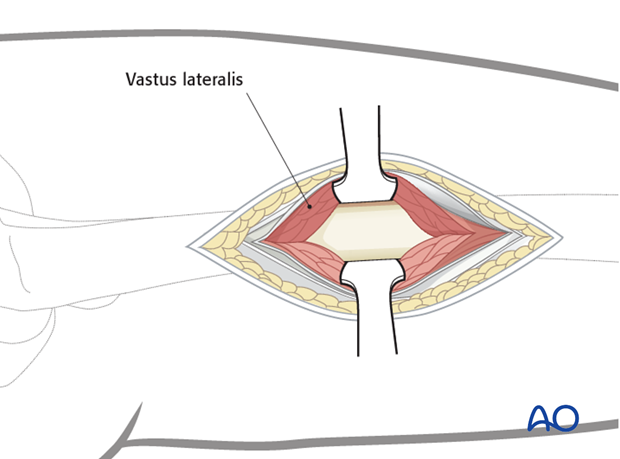
Plate placement
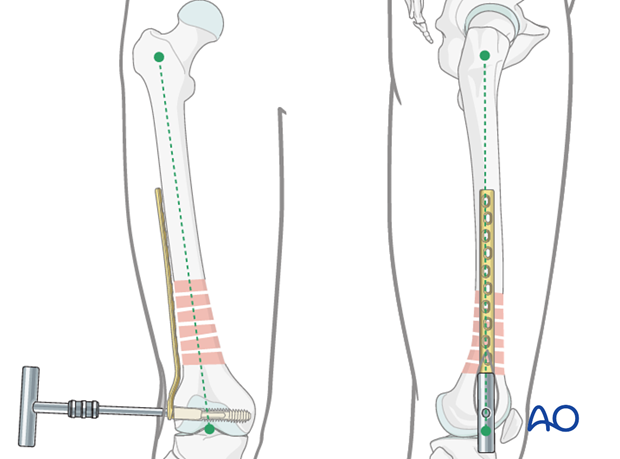
The T-handle is now detached and the plate is inserted submuscularly, from distal to proximal.
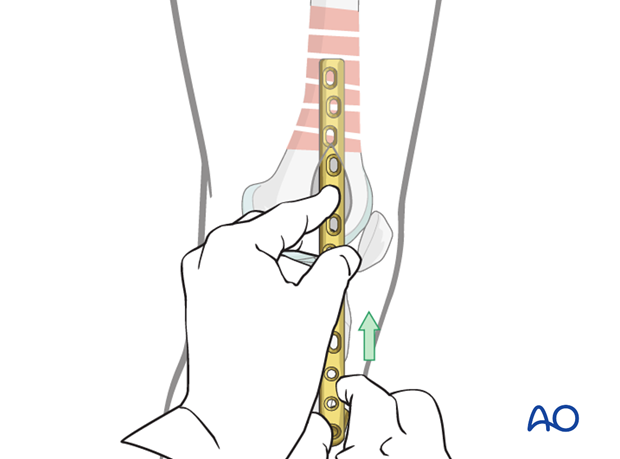
Preparation of the plate tunnel
Three options are in use for preparation of the plate path along the proximal main fragment.
- Insert a long pair of scissors, spread them, and then pull backwards
- Insert a periosteal elevator and slide it extraperiosteally along the proximal main fragment. (The tip of the plate can be used in a same manner)
- A soft tissue-retractor is available which serves the same purpose
Plate and screw combination
The T-handle is then inserted through the barrel of the plate and reconnected to the screw. This can be challenging and often requires abandoning the preliminary reduction.
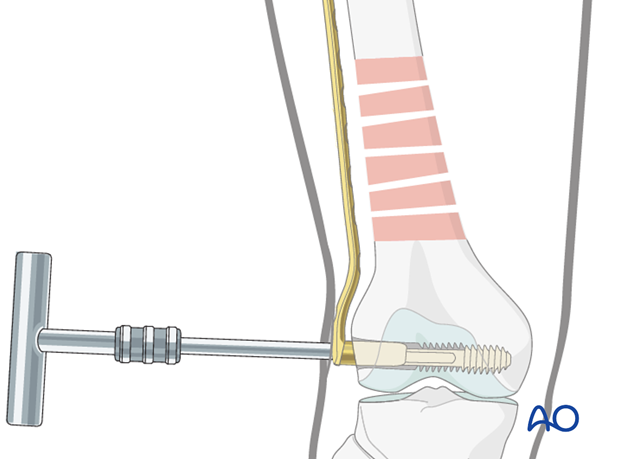
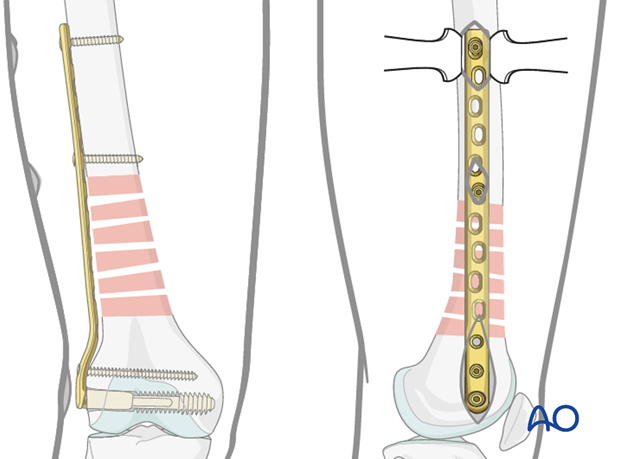
Final screw placement
When the condylar screw is in its final position (the T-handle is then parallel, on the lateral view, to the long axis of the distal fragment), the barrel is slipped fully over the screw and the T-handle removed. A cancellous screw can then be inserted into the distal screw hole of the plate to prevent rotation of the main distal fragment around the axis of the condylar screw.
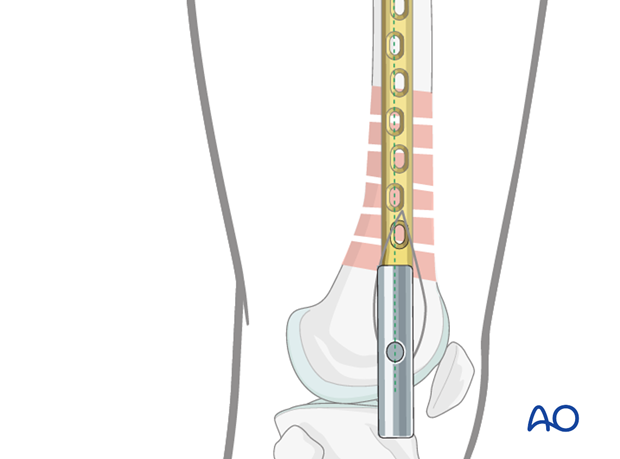
6. Plate fixation to proximal fragment
Verification of reduction
Under image intensifier control, the preliminary reduction is checked again with respect to axial alignment, length and, to a certain degree, rotation (in more complex fractures, judging the clinical accuracy of the rotation becomes more important, while at the same time the associated radiological findings can be challenging to interpret).
Insertion of first screw into proximal fragment
The approaches / stab incisions over the proximal fragment are made according to the planned final screw placement.
Two blunt Hohmann retractors placed ventrally and dorsally around the femoral shaft control the lateral position of the plate.
If the overall reduction is found to be satisfactory, the first cortical screw in the distal part of the proximal fragment is inserted, without being fully tightened. This still allows for the plate position to be fine-tuned.

Pearl: final reduction
If the lateral position prior to the placement of the second screw is inadequate, the use of sterile bolsters is recommended to aid correction.
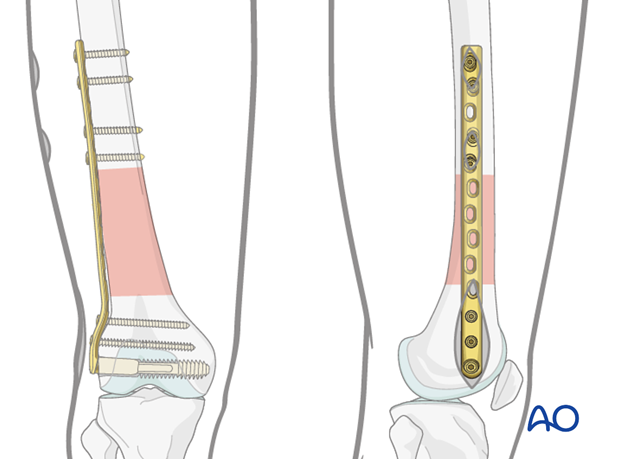
Insertion of a second screw into proximal fragment
The lateral plate position is confirmed by using two Hohmann retractors introduced through the second approach / stab incision over the proximal plate portion, or by palpation.
Once the most proximal screw is inserted, the more distal screw in the proximal fragment is fully tightened.
7. Additional screw insertion
According to preoperative planning, additional screws are inserted into the distal and proximal main fragments.
8. Aftercare
Compartment syndrome and nerve injury
Close monitoring of the femoral muscle compartments should be carried out especially during the first 48 hours, in order to rule out compartment syndrome.
Postoperative assessment
In all cases in which radiological control has not been used during the procedure, a check x-ray to determine the correct placement of the implant and fracture reduction should be taken within 24 hours.
Functional treatment
Unless there are other injuries or complications, mobilization may be started on postoperative day 1. Static quadriceps exercises with passive range of motion of the knee should be encouraged. If a continuous passive motion device is used, this must be discontinued at regular intervals for the essential static muscle exercises. Afterwards special emphasis should be placed on active knee and hip movement.
Weight bearing
Full weight bearing may be performed with crutches or a walker.
Follow-up
Wound healing should be assessed regularly within the first two weeks. Subsequently a 6 and 12 week clinical and radiological follow-up is usually made. A longer period may be required if the fracture healing is delayed.
Implant removal
Implant removal is not mandatory and should be discussed with the patient, if there are implant-related symptoms after consolidated fracture healing.













