Total elbow arthroplasty
1. General considerations
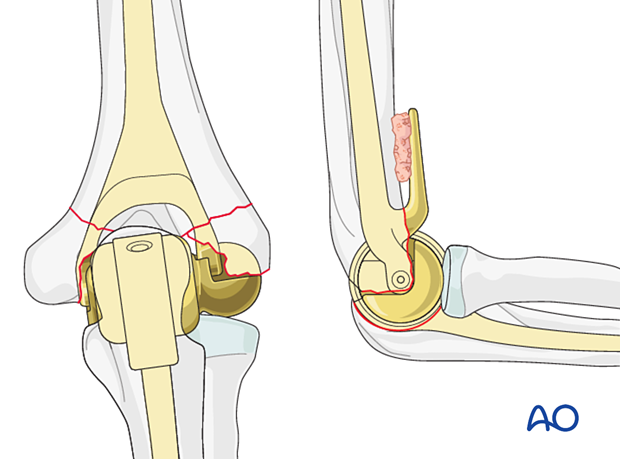
A total elbow arthroplasty performed for fractures is an inherently stable construct as the humeral and ulnar components are linked.
A potential disadvantage of this technique is the risk of stem loosening because of load transfer to the stem-cement-bone interface and polyethylene wear at the implant linkage.
Implant type
There are several total elbow arthroplasty systems available. Surgeons should refer to the manufacturer’s specific operative technique of their chosen implant for details. One system is illustrated in this procedure to demonstrate the generic techniques and principles.
Implant size
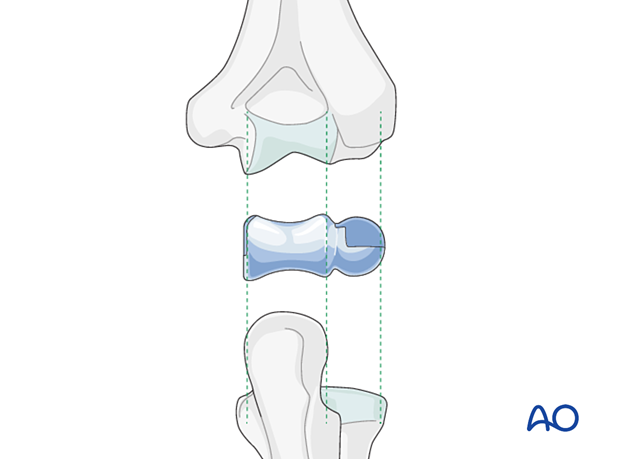
Compare implant size of the humeral trial spools with the patient’s native olecranon and radial head.
Sizing of the spool determines the stem size to be used.
Note: Ulnar nerve at risk
2. Patient preparation and approaches
Patient positioning
The patient is positioned in lateral decubitus or supine position according to surgeon’s preference.
The whole extremity should be prepared and draped.
The use of a sterile tourniquet is optional.
Approaches
For arthroplasty, access is needed to the whole distal humerus with additional access to the olecranon for total arthroplasty.
In general, triceps-sparing approaches (eg, paratricipital and lateral paraolecranon) are preferable to triceps-reflecting approaches (eg, triceps split or Bryan-Morrey) for all types of arthroplasty in fractures as they allow immediate rehabilitation with no need to protect a triceps repair and provide a more robust soft-tissue envelope which minimizes the risk of wound complications.
A transolecranon approach should not be used for total elbow replacement.
3. Humeral preparation
Removal of fragments
Remove the fractured articular fragments.
For a total elbow replacement, the epicondylar fragments may be excised or retained.
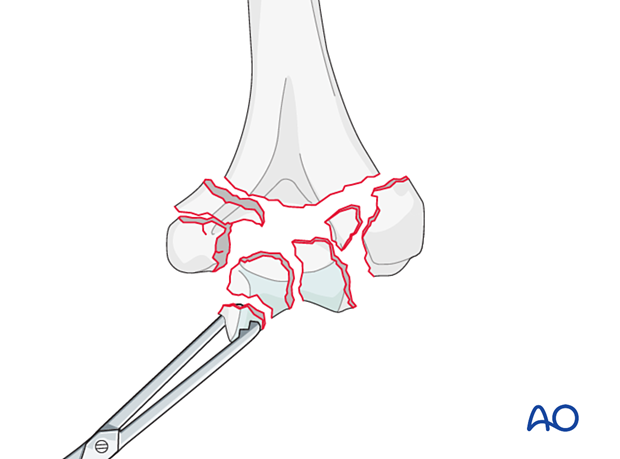
In almost all distal humeral fractures, the roof of the olecranon fossa remains in continuity with the humeral shaft regardless of fracture comminution.
This is the landmark for entry to the humeral canal.
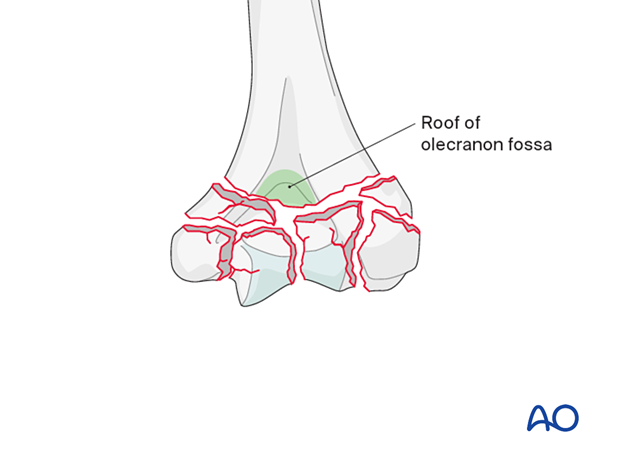
Opening the medullary canal
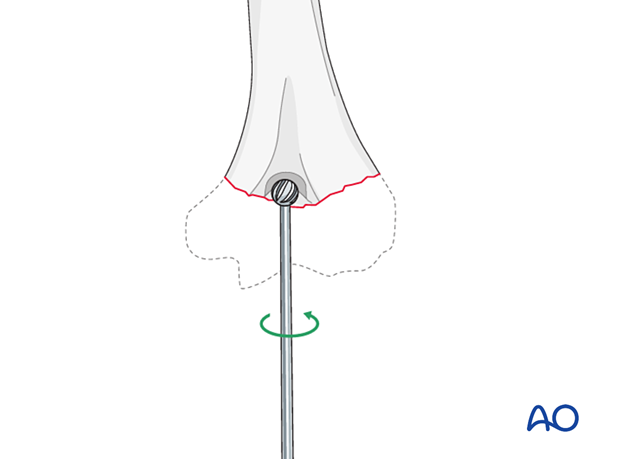
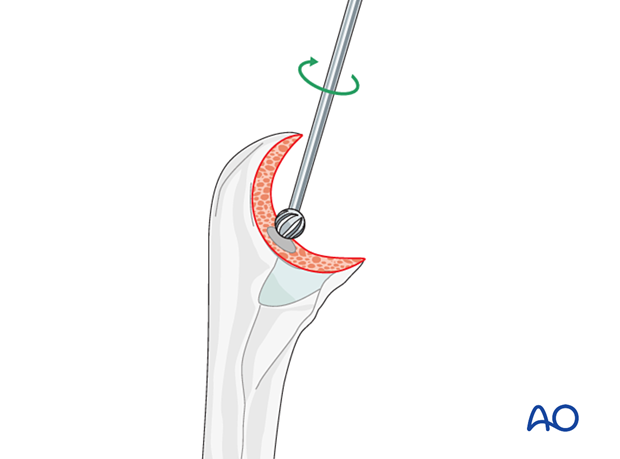
Open the olecranon fossa roof with a high-speed burr or bone nibbler and broach the humeral canal sequentially.
Alternatively, a guide wire and cannulated reamer may be used before broaching.
Implant length
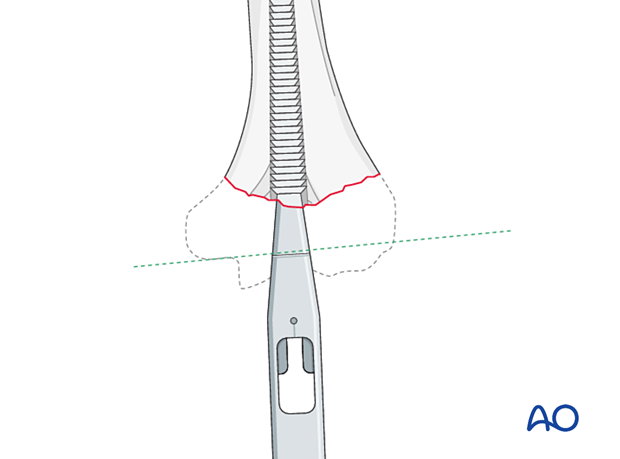
Broach up to the depth where the laser line on the broaching instrument is parallel to the flexion/extension axis of the humerus.
In fractures, the bony landmarks may not be intact, so the olecranon fossa roof should be used as a guide for depth and implant length.
Another way of assessing implant length is to provisionally reduce the fractured condyles around the shaft. The flexion/extension axis lies parallel to the inferior margin of the medial epicondyle.
Remove with a saw, bone nibbler, or rongeur, all remaining bony prominence that will hinder further preparation or proper implant insertion.
Implant rotation
To prepare for the fins of the humeral component, insert the gusset broach in correct rotation into the humerus until the laser line is level with the flexion/extension axis of the humerus.
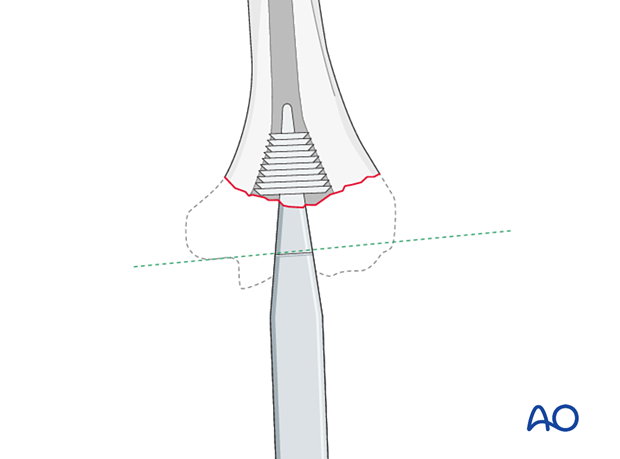
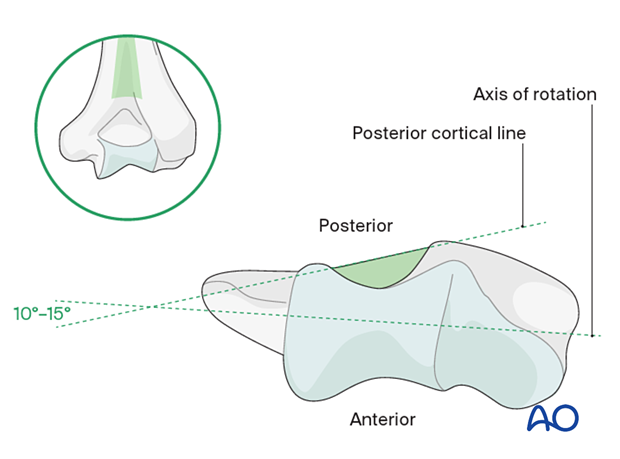
It is important to place the humeral component in the correct rotation. The implant rotation should be parallel to the epicondylar axis.
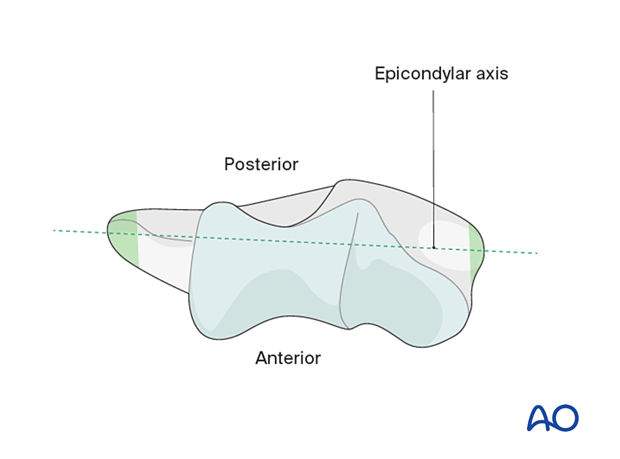
In a fracture, these bony landmarks may be disrupted. In this situation, rotation can be referenced from the flat surface of the intact humerus proximal to the olecranon fossa. The implant should be 10°–15° internally rotated to this landmark to match the correct native rotation.
Humeral trial
Insert the appropriately sized humeral trial and confirm satisfactory position.
4. Ulnar preparation
Removal of the articular surface
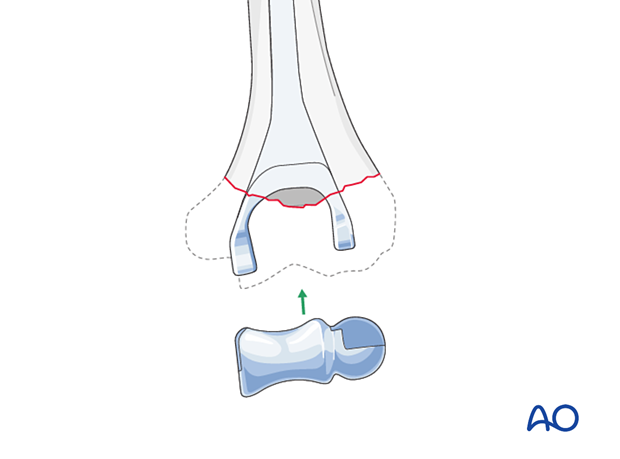
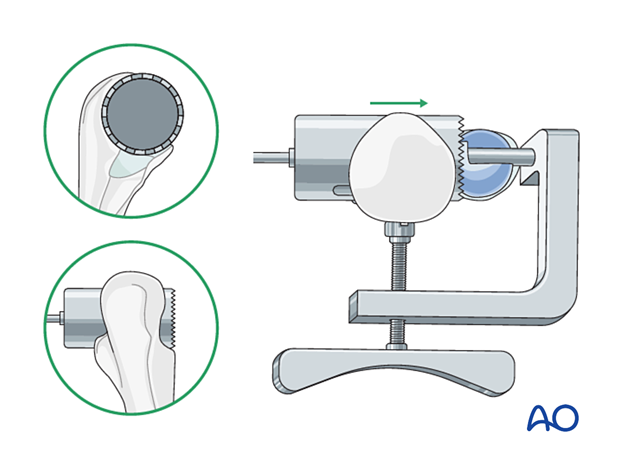
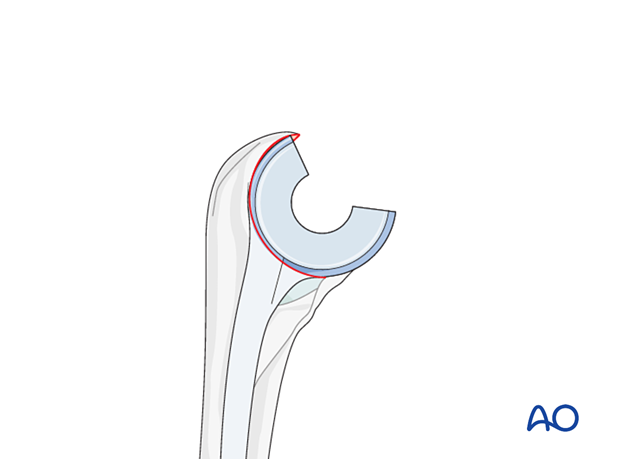
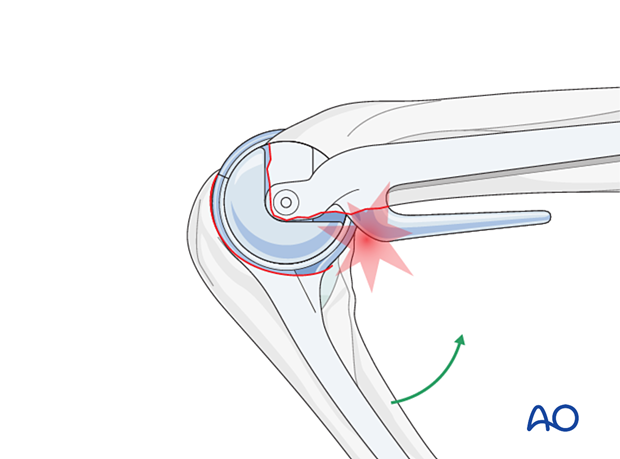
Place the appropriately sized articular spool in the greater sigmoid notch of the ulna.
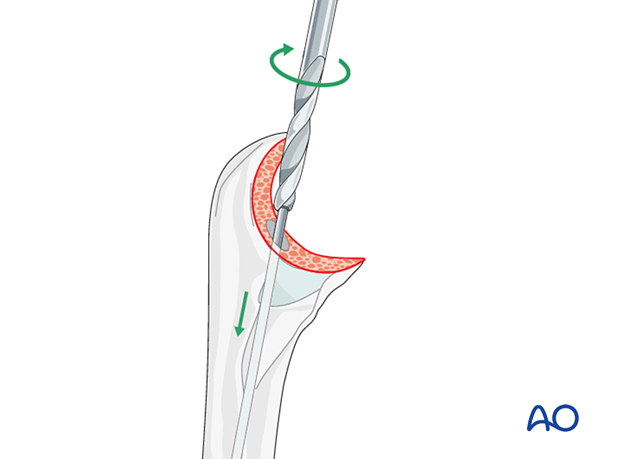
Use the bell saw and jig to remove the articular surface of the olecranon.
An alternative method is to remove the articular surface with a barrel reamer or high-speed burr.
The radial head can be resected at this point if desired.
Opening the medullary canal
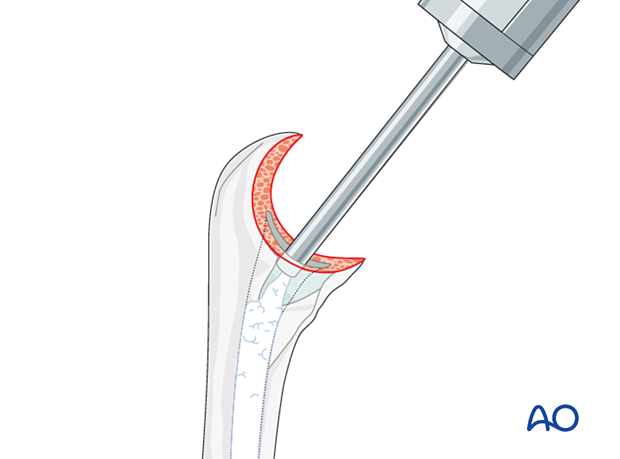
Open the ulnar canal at the base of the coronoid with a high-speed burr.
Ulnar broaching
It may be easier to use a cannulated reamer to expand the ulnar diaphysis before broaching.
Broach the ulna sequentially up to the desired size.
Take care to ensure the ulna is broached in the correct rotation.
This can be referenced from the native radial head and/or the flat dorsal surface of the ulna. The correct ulnar component rotation is parallel to this surface.
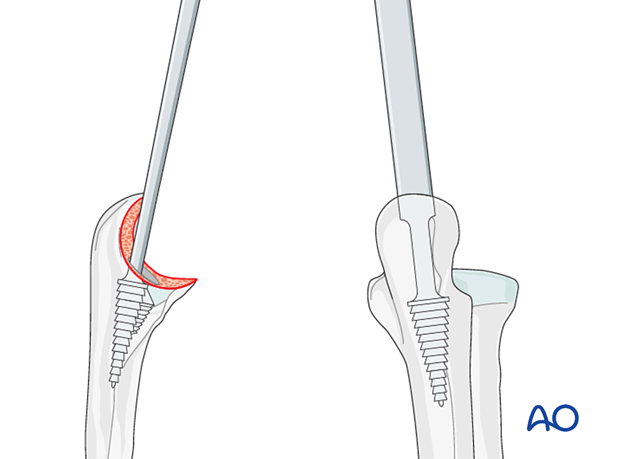
Ulnar trial
Insert the appropriately sized ulnar trial and confirm satisfactory position.
5. Trial, reduction, and implant assembly
Trial and reduction
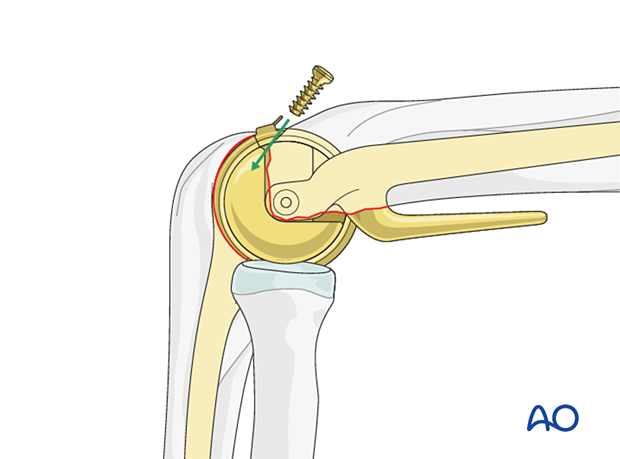
Reduce the two components to each other and link them to the ulnar cap. Check for range of motion and bony impingement.
Final implant assembly
After removal of all trial implants, assemble the chosen components individually and prepare the canals for cementing.
6. Cementing technique and bone graft
A third-generation cementing technique should be used.
Insert low-viscosity cement in a retrograde fashion using a cement gun behind cement restrictors.
Narrow nozzles are required to fit inside the ulna.
Insert the implants individually and remove any excess cement.
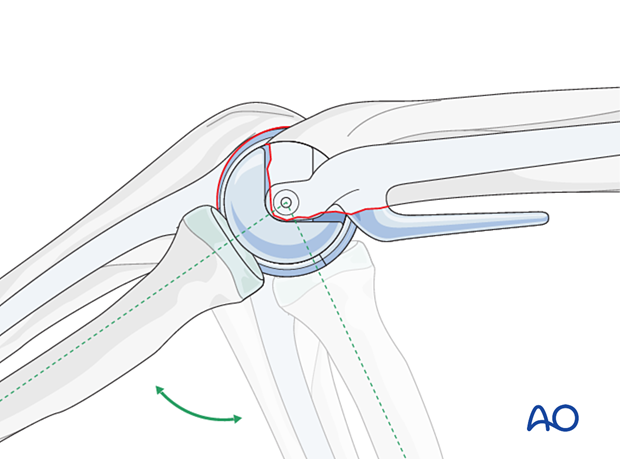
Reduce the joint and link the components.
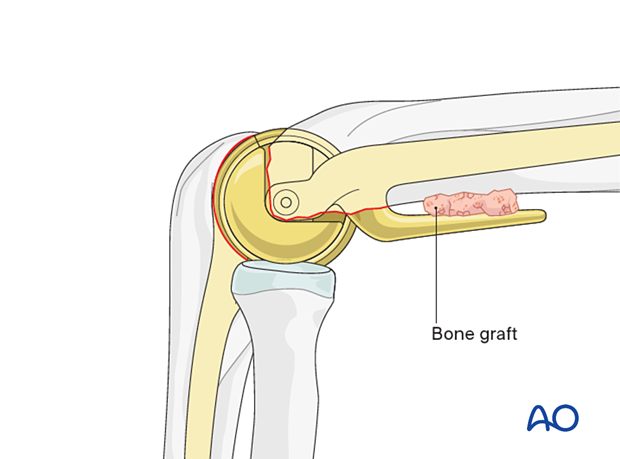
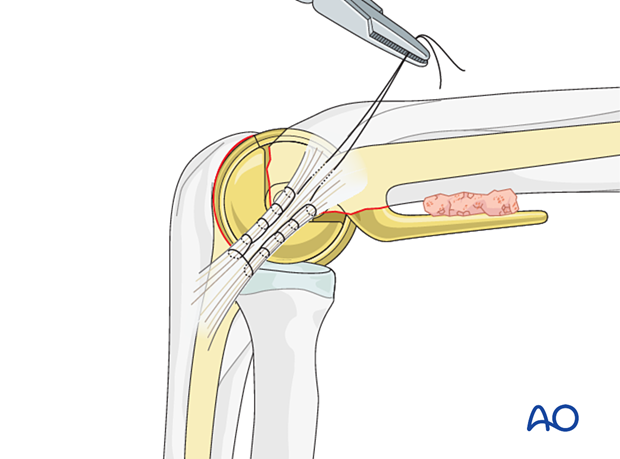
Fashion a wedge-shaped cancellous bone graft from the resected articular fragments and insert it between the anterior humeral cortex and the anterior flange of the humeral component.
7. Closure
In a total elbow replacement for fracture, the fractured condyles and collateral ligaments can be repaired around the humeral component or resected as the implant is linked.
Management of the triceps depends on which approach has been used.
The ulnar nerve should be managed according to surgeon’s preference but should be free of tension or impingement against any metallic or prominent bony surface.
8. Aftercare
Immediate aftercare
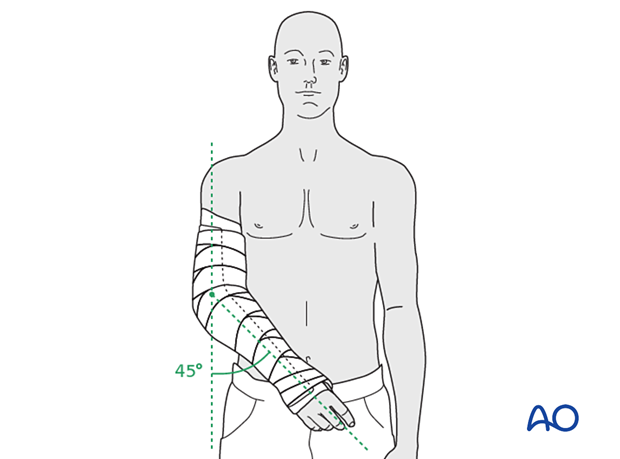
If the soft tissues are vulnerable, it is recommended to rest the elbow in semiextension using a splint for up to 10 days.
Rehabilitation and precautions
If a triceps-reflecting approach has been used, active extension should be avoided for 4–6 weeks to allow bone-tendon healing.
If a triceps-sparing approach has been used, no such restriction is necessary.
Following total elbow replacement, it is recommended that patients avoid lifelong heavy or repetitive use of the operated arm to minimize the risk of early polyethylene wear and stem loosening.













